Infect Chemother.
2010 Jun;42(3):181-186. 10.3947/ic.2010.42.3.181.
A Case of Cerebral Toxoplasmosis Following Tandem Autologous Stem Cell Transplantation in a Multiple Myeloma Patient
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. molder@unitel.co.kr
- KMID: 2170307
- DOI: http://doi.org/10.3947/ic.2010.42.3.181
Abstract
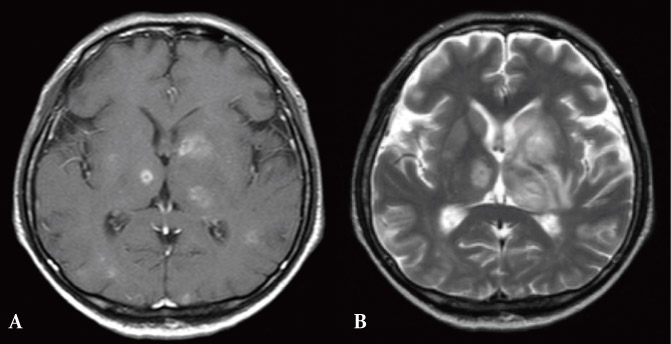
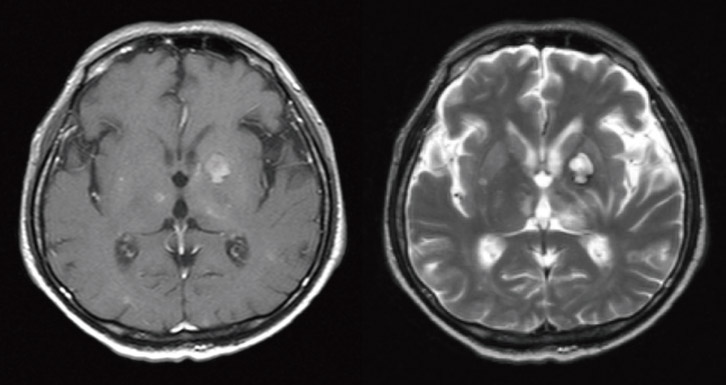
- Toxoplasmosis is a rare but fatal complication in hematopoietic stem cell transplant recipients, usually associated with allogeneic hematopoietic stem cell transplantation (HSCT). We report a case of cerebral toxoplasmosis in a patient with multiple myeloma, following tandem autologous stem cell transplantation. A 55-year-old Korean male presented with weakness in both legs that had progressed to both arms. A magnetic resonance imaging scan of the brain revealed multiple, variable-sized ring-enhancing lesions with surrounding edema in the cerebral hemispheres and brain stem. Stereotactic biopsy revealed bradyzoites of Toxoplasma gondii in the brain tissue. The patient received trimethoprim-sulfamethoxazole, followed by pyrimethamine and sulfadiazine, accompanying treatment for progressive multiple myeloma. Cerebral toxoplasmosis should be considered as one of the differential diagnoses in patients with neurologic signs following autologous HSCT.
MeSH Terms
-
Arm
Biopsy
Brain
Brain Stem
Cerebrum
Diagnosis, Differential
Edema
Hematopoietic Stem Cell Transplantation
Hematopoietic Stem Cells
Humans
Leg
Magnetic Resonance Imaging
Male
Middle Aged
Multiple Myeloma
Neurologic Manifestations
Pyrimethamine
Stem Cell Transplantation
Stem Cells
Sulfadiazine
Toxoplasma
Toxoplasmosis
Toxoplasmosis, Cerebral
Trimethoprim, Sulfamethoxazole Drug Combination
Pyrimethamine
Sulfadiazine
Figure
Reference
-
1. Mele A, Paterson PJ, Prentice HG, Leoni P, Kibbler CC. Toxoplasmosis in bone marrow transplantation: a report of two cases and systematic review of the literature. Bone Marrow Transplant. 2002. 29:691–698.
Article2. Kotton CN. Zoonoses in solid-organ and hematopoietic stem cell transplant recipients. Clin Infect Dis. 2007. 44:857–866.
Article3. Pagano L, Trapè G, Putzulu R, Caramatti C, Picardi M, Nosari A, Cinieri S, Caira M, Del Favero A. GIMEMA (Gruppo Italiano Malattie Ematologiche dell'Adulto)-Infection Program. Toxoplasma gondii infection in patients with hematological malignancies. Ann Hematol. 2004. 83:592–595.
Article4. Roemer E, Blau IW, Basara N, Kiehl MG, Bischoff M, Günzelmann S, Kirsten D, Sanchez H, Wocker EL, Fauser AA. Toxoplasmosis, a severe complication in allogeneic hematopoietic stem cell transplantation: successful treatment strategies during a 5-year single-center experience. Clin Infect Dis. 2001. 32:E1–E8.
Article5. Martino R, Bretagne S, Rovira M, Ullmann AJ, Maertens J, Held T, Deconinck E, Cordonnier C. Toxoplasmosis after hematopoietic stem transplantation. Report of a 5-year survey from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2000. 25:1111–1114.
Article6. Edvinsson B, Lundquist J, Ljungman P, Ringdén O, Evengård B. A prospective study of diagnosis of Toxoplasma gondii infection after bone marrow transplantation. APMIS. 2008. 116:345–351.
Article7. Jones JL, Kruszon-Moran D, Wilson M, McQuillan G, Navin T, McAuley JB. Toxoplasma gondii infection in the United States: seroprevalence and risk factors. Am J Epidemiol. 2001. 154:357–365.
Article8. Lee YH, Noh HJ, Hwang OS, Lee SK, Shin DW. Seroepidemiological study of Toxoplasma gondii infection in the rural area Okcheon-gun, Korea. Korean J Parasitol. 2000. 38:251–256.
Article9. Yang HJ, Jin KN, Park YK, Hong SC, Bae JM, Lee SH, Choi HS, Hwang HS, Chung YB, Lee NS, Nam HW. Seroprevalence of toxoplasmosis in the residents of Cheju island, Korea. Korean J Parasitol. 2000. 38:91–93.
Article10. Song KJ, Shin JC, Shin HJ, Nam HW. Seroprevalence of toxoplasmosis in Korean pregnant women. Korean J Parasitol. 2005. 43:69–71.
Article11. Shin DW, Cha DY, Hua QJ, Cha GH, Lee YH. Seroprevalence of Toxoplasma gondii Infection and characteristics of sero-positive patients in general hospitals in Daejeon, Korea. Korean J Parasitol. 2009. 47:125–130.
Article12. Kim BH, Lee SI, Lee CH, Cha SH, Lee TH, Lee SH, Chung JS, Cho GJ. A case of cerebral toxoplasmosis in a patient with acquired immune defeciency syndrome. Infect Chemother. 2004. 36:181–184.13. Nam TS, Seo KS, Lee KI, Kim YS, Hong JH, Kim GH, Jeong JH, Chu HJ, Park SK, Seoung NH, Jung JS, Cho GJ. The clinical study of hematoimmunologic features and opportunistic infections of patients with AIDS. Korean J Med. 1997. 52:15–23.14. Chandrasekar PH, Momin F. Bone Marrow Transplant Team. Disseminated toxoplasmosis in marrow recipients: a report of three cases and a review of the literature. Bone Marrow Transplant. 1997. 19:685–689.
Article15. de Medeiros BC, de Medeiros CR, Werner B, Loddo G, Pasquini R, Bleggi-Torres LF. Disseminated toxoplasmosis after bone marrow transplantation: report of 9 cases. Transpl Infect Dis. 2001. 3:24–28.
Article16. Anaissie E, Nucci M. Bowden RA, Ljungman P, Paya CV, editors. Risk and epidemiology of infections after autologous hemopoietic stem cell transplantation. Transplant infections. 2003. 2nd ed. Philadelphia: Lippincott Winlliams & Wilkins;39–50.17. Martino R. Bowden RA, Ljungman P, Paya CV, editors. Toxoplasmosis after hematopoietic stem cell transplantation. Transplant Infections. 2003. 2nd ed. Philadelphia: Lippincott Winlliams & Wilkins;535–540.
Article18. López-Duarte M, Insunza A, Conde E, Iriondo A, Mazorra F, Zubizarreta A. Cerebral toxoplasmosis after autologous peripheral blood stem cell transplantation. Eur J Clin Microbiol Infect Dis. 2003. 22:548–550.
Article19. Duband S, Cornillon J, Tavernier E, Dumollard JM, Guyotat D, Péoc'h M. Toxoplasmosis with hemophagocytic syndrome after bone marrow transplantation: diagnosis at autopsy. Transpl Infect Dis. 2008. 10:372–374.
Article20. Mileshkin L, Stark R, Day B, Seymour JF, Zeldis JB, Prince HM. Development of neuropathy in patients with myeloma treated with thalidomide: patterns of occurrence and the role of electrophysiologic monitoring. J Clin Oncol. 2006. 24:4507–4514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pre-transplant Disease Status is Important for an Improved Outcome of the Second Stem Cell Transplantation in the Myeloma Patients Receiving the First Autologous Stem Cell Transplantation
- Skin Graft-versus-host Disease Following Autologous Stem Cell Transplantation for Multiple Myeloma
- HBV reactivation in a HBsAg-negative patient with multiple myeloma treated with prednisolone maintenance therapy after autologous HSCT
- Successful Chemotherapy Following Autologous Stem Cell Transplantation in Multiple Myeloma and Multi-organ Dysfunction with Infiltration of Eosinophils: A Case Report
- Emergence of chronic myeloid leukemia following autologous stem cell transplantation in a young woman with multiple myeloma