J Breast Cancer.
2009 Sep;12(3):170-178. 10.4048/jbc.2009.12.3.170.
The Usefulness and Limitations of Intraoperative Frozen Section Analysis of Sentinel Lymph Nodes in Patients with Breast Cancer
- Affiliations
-
- 1Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea. ykbae@ynu.ac.kr
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 3Department of Preventive Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- KMID: 2242008
- DOI: http://doi.org/10.4048/jbc.2009.12.3.170
Abstract
- PURPOSE
Intraoperative frozen sectioning (FS) of sentinel lymph nodes (SLNs) is widely used to determine whether total axillary lymph node dissection should be performed in patients with breast cancer. We evaluated the usefulness and limitations of the FS protocol, which has been used in our institution for the intraoperative SLN examination.
METHODS
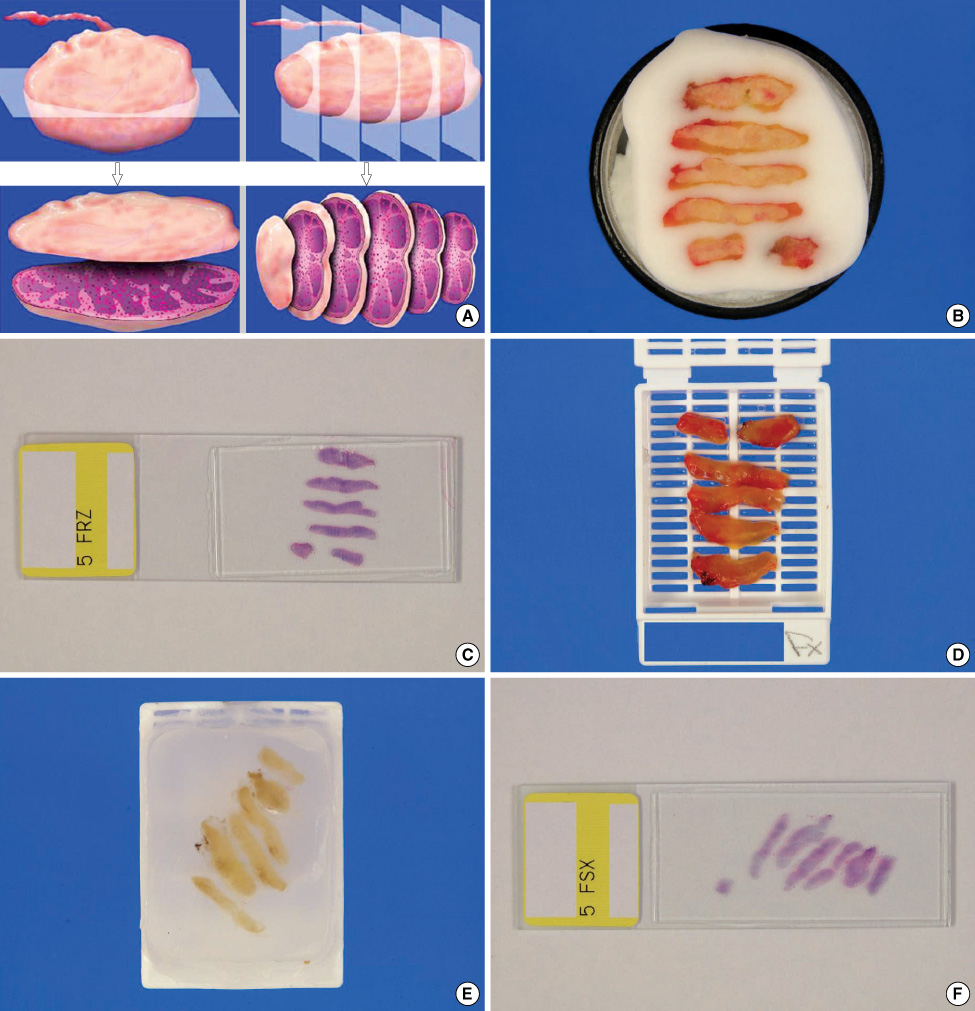
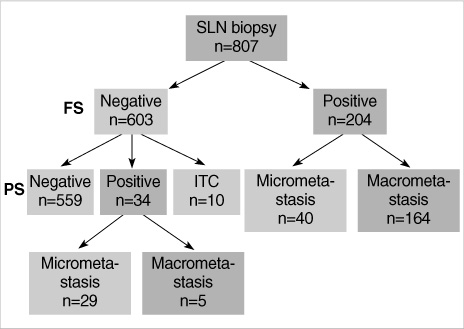
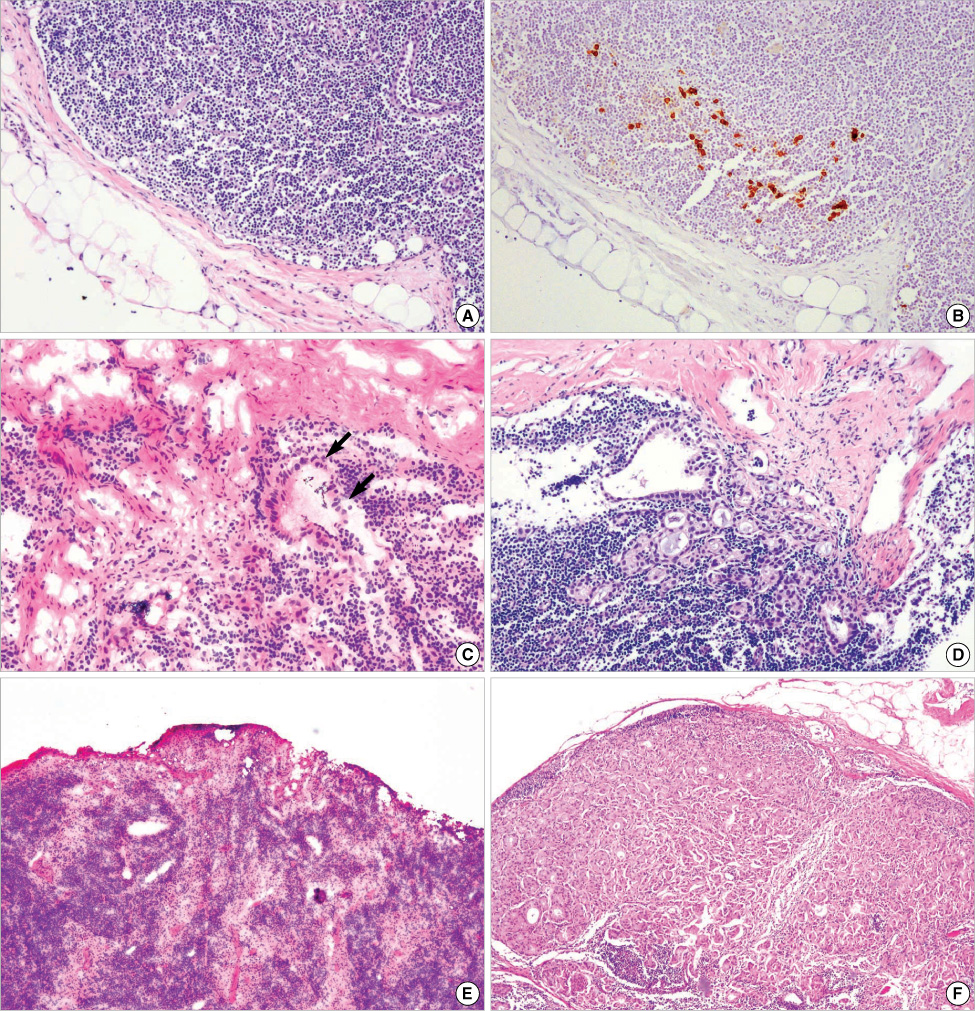
We analyzed the FS results of SLNs in 807 invasive breast carcinoma patients who underwent intraoperative SLN biopsy between January 2005 and December 2007. Lymph nodes larger than 5 mm were sliced at 2 mm intervals and all the slices were submitted for FS. The remaining tissue of the SLN was formalin-fixed and paraffin-embedded for permanent sectioning (PS). If the FS result was negative for tumor cells, then immunohistochemical stain for pancytokeratin was performed. The metastatic SLNs were graded according to the AJCC cancer staging manual (6th edition). The results of FS and PS were compared with regard to the pathologic diagnosis.
RESULTS
The average number of SLNs was 2.9 per patients. A total of 204 (25.3%) patients were reported to have a metastatic SLN(s) on the FS. Among the 603 patients with negative FS results, 34 (5.6%) patients showed metastasis on the PS. Another 10 (1.7%) patients who had negative results on FS showed isolated tumor cells on the PS or on the cytokeratin immunohistochemistry. Twenty-nine of the 34 (85.3%) false negative cases showed micrometastasis on the PS. Ten (29.4%) false negative results were caused by interpretation errors and 24 (70.6%) were caused by technical problems.
CONCLUSION
The false negative rate of our protocol for FS of a SLN was low. The failure of FS was largely caused by the failure to detect micrometastasis. FS is a reliable method for an intraoperative SLN examination if a very stringent protocol is used.
MeSH Terms
Figure
Cited by 1 articles
-
One-step Nucleic Acid Amplification (OSNA): Intraoperative Rapid Molecular Diagnostic Method for the Detection of Sentinel Lymph Node Metastases in Breast Cancer Patients in Korean Cohort
Yoon-La Choi, Soo Kyung Ahn, Young Kyung Bae, In Ae Park, Jun Won Min, Kyu-Won Lee, Jin hye Bae, Wonshik Han, Jung-Eun Choi, Eun Yoon Cho, Sangmin Kim, Hye Sook Lee, Seok Jin Nam, Jeong Eon Lee, Soo-Jung Lee, Dong-Young Noh, Jung-Hyun Yang
J Breast Cancer. 2010;13(4):366-374. doi: 10.4048/jbc.2010.13.4.366.
Reference
-
1. Langer I, Guller U, Berclaz G, Koechli OR, Schaer G, Fehr MK, et al. Morbidity of sentinel lymph node biopsy (SLN) alone versus SLN and completion axillary lymph node dissection after breast cancer surgery: a prospective Swiss multicenter study on 659 patients. Ann Surg. 2007. 245:452–461.
Article2. Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006. 98:599–609.
Article3. Langer I, Guller U, Berclaz G, Koechli OR, Moch H, Schaer G, et al. Accuracy of frozen section of sentinel lymph nodes: a prospective analysis of 659 breast cancer patients of the Swiss multicenter study. Breast Cancer Res Treat. 2009. 113:129–136.
Article4. van de Vrande S, Meijer J, Rijnders A, Klinkenbijl JH. The value of intraoperative frozen section examination of sentinel lymph nodes in breast cancer. Eur J Surg Oncol. 2009. 35:276–280.
Article5. Schwartz GF, Krill LS, Palazzo JP, Dasgupta A. Value of intraoperative examination of axillary sentinel nodes in carcinoma of the breast. J Am Coll Surg. 2008. 207:758–762.
Article6. Ali R, Hanly AM, Naughton P, Castineira CF, Landers R, Cahill RA, et al. Intraoperative frozen section assessment of sentinel lymph nodes in the operative management of women with symptomatic breast cancer. World J Surg Oncol. 2008. 6:69.
Article7. Kim HJ, Chang MA, Hong SJ, Lee JS, Jung MS, Kim MJ, et al. Result of sentinel lymph node biopsy using radioisotope in clinically lymph node negative breast cancer. J Breast Cancer. 2007. 10:141–146.
Article8. Lee DH, Kim BS, Kang SH, Lee NH, Lee SJ, Bae YK. Prediction of nonsentinel lymph node (NSLN) metastasis in breast cancer patients; the usefulness of isotope counts for sentinel lymph node (SLN) classification. J Korean Surg Soc. 2006. 70:341–348.9. Lee HD, Choi JW, Kim DY, Park BW, Lee IK, Song HJ, et al. Clinical experience for sentinel lymphadenectomy alone in early breast cancer. J Korean Breast Cancer Soc. 2003. 6:263–270.
Article10. Nurko J, Broadwater JR, Edwards MJ. Winchester DJ, Winchester DP, Hudis CA, Norton L, editors. Axillary staging and therapeutics. Breast cancer. 2006. 2nd ed. Hamilton: BC Decker;302–311.11. Zavagno G, De Salvo GL, Bozza F, Scalco G, Marconato R, Valletta S, et al. Number of metastatic sentinel nodes as predictor of axillary involvement in patients breast cancer. Breast Cancer Res Treat. 2004. 86:171–179.
Article12. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, editors. Breast. AJCC Cancer Staging Manual. 2002. 6th ed. New York: Springer;223–240.
Article13. Tasmuth T, von Smitten K, Kalso E. Pain and other symptoms during the first year after radical and conservative surgery for breast cancer. Br J Cancer. 1996. 74:2024–2031.
Article14. Shaw JH, Rumball EM. Complications and local recurrence following lymphadenectomy. Br J Surg. 1990. 77:760–764.
Article15. Chao C. The use of frozen section and immunohistochemistry for sentinel lymph node biopsy in breast cancer. Am Surg. 2004. 70:414–419.16. Yun HR, Yoo KE, Choi YJ, Woo SU, Choi YL, Kim JH, et al. Intraoperative examination of sentinel lymph nodes by rapid immunohistochemistry in breast cancer. J Korean Surg Soc. 2006. 70:275–280.17. Tsujimoto M, Nakabayashi K, Yoshidome K, Kaneko T, Iwase T, Akiyama F, et al. One-step nucleic acid amplification for intraoperative detection of lymph node metastasis in breast cancer patients. Clin Cancer Res. 2007. 13:4807–4816.
Article18. Visser M, Jiwa M, Horstman A, Brink AA, Pol RP, van Diest P, et al. Intra-operative rapid diagnostic method based on CK19 mRNA expression for the detection of lymph node metastases in breast cancer. Int J Cancer. 2008. 122:2562–2567.
Article19. Weiser MR, Montgomery LL, Susnik B, Tan LK, Borgen PI, Cody HS. Is routine intraoperative frozen-section examination of sentinel lymph nodes in breast cancer worthwhile? Ann Surg Oncol. 2000. 7:651–655.
Article20. Grabau DA, Rank F, Friis E. Intraoperative frozen section examination of axillary sentinel lymph nodes in breast cancer. APMIS. 2005. 113:7–12.
Article21. Goyal A, Newcombe RG, Mansel RE. Clinical relevance of multiple sentinel nodes in patients with breast cancer. Br J Surg. 2005. 92:438–442.
Article22. McCarter MD, Yeung H, Fey J, Borgen PI, Cody HS 3rd. The breast cancer patient with multiple sentinel nodes: when to stop? J Am Coll Surg. 2001. 192:692–697.
Article23. Fitzgibbons PL, Page DL, Weaver D, Thor AD, Allred DC, Clark GM, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000. 124:966–978.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is the intraoperative frozen section analysis of sentinel lymph nodes necessary in clinically negative node breast cancer?
- Short Term Follow-up Data in Breast Cancer Patients with Sentinel Lymph Node Biopsy Alone
- Reliability of Sentinel Lymph Node Biopsy after Neoadjuvant Chemotherapy in Breast Cancer Patients
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Application of Raman spectroscopy in breast cancer surgery