Korean J Crit Care Med.
2014 Nov;29(4):313-319. 10.4266/kjccm.2014.29.4.313.
Change in Red Cell Distribution Width as Predictor of Death and Neurologic Outcome in Patients Treated with Therapeutic Hypothermia after Out-of-Hospital Cardiac Arrest
- Affiliations
-
- 1Emergency Medicine, Gil Medical Center, Gachon University, Incheon, Korea. truecho@hanmail.net
- KMID: 2227739
- DOI: http://doi.org/10.4266/kjccm.2014.29.4.313
Abstract
- BACKGROUND
The prognostic significance of change in red cell distribution width (RDW) during hospital stays in patients treated with therapeutic hypothermia (TH) after out-of-hospital cardiac arrest (OHCA) was investigated.
METHODS
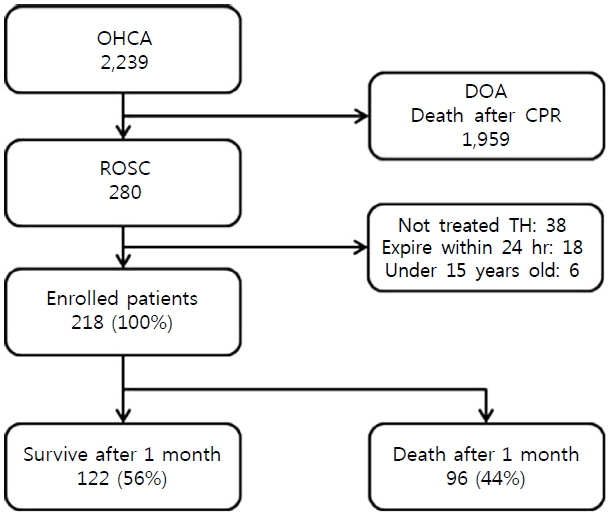
Patients treated with TH after OHCA between January 2009 and August 2013 were reviewed. Patients with return of spontaneous circulation (ROSC) were assessed according to Utstein Style. Hematologic variables including RDW, hematocrit, white blood cell count, and platelets were also obtained. RDW changes during the 72 hours after ROSC were categorized into five groups as follows: Group 1 (-0.8-0.1%), Group 2 (0.2-0.3%), Group 3 (0.4-0.5%), Group 4 (0.6-0.8%), and Group 5 (>0.8%).
RESULTS
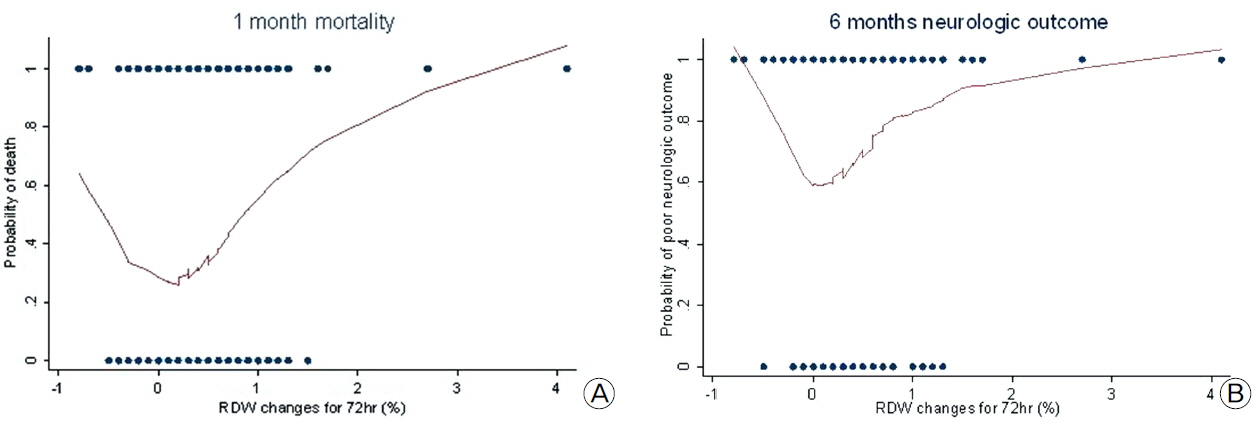
A total of 218 patients were enrolled in the study. RDW changes during the 72 hours after ROSC in Group 4 (HR 3.56, 95% CI 1.25-10.20) and Group 5 (HR 5.07, 95% CI 1.73-14.89) were associated with a statistically significant difference in one-month mortality. RDW changes were associated with statistically significant differences in neurologic outcome at 6 months after ROSC (Group 3 [HR 2.45, 95% CI 1.17-5.14], Group 4 [HR 2.79, 95% CI 1.33-5.84], Group 5 [HR 3.50, 95% CI 1.35-7.41]). Other significant variables were location of arrest, cause of arrest, serum albumin, and advanced cardiac life support time.
CONCLUSIONS
RDW change during the 72 hours after ROSC is a predictor of mortality and neurologic outcome in patients treated with TH after OHCA.
MeSH Terms
Figure
Reference
-
References
1). Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2013 update: a report from the American heart association. Circulation. 2013; 127:e1–240.2). Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM. Presentation, management, and outcome of out of hospital cardiopulmonary arrest: comparison by underlying aetiology. Heart. 2003; 89:839–42.
Article3). Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005; 67:75–80.
Article4). Temple A, Porter R. Predicting neurological outcome and survival after cardiac arrest. Continuing Education in Anaesthesia, Critical Care & Pain. [serial on the internet]. 2012. May. [2012 May 21]. Available from http://ceaccp.oxfordjournals.org/content/early/2012/05/20/bjaceaccp.mks029.full.
Article5). Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttige BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International liaison committee on resuscitation (American heart association, Australian and New Zealand Council on resuscitation, European resuscitation council, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation council of Asia, and the resuscitation council of Southern Africa); the American heart association emergency cardiovascular care committee; the council on cardiovascular surgery and anesthesia; the council on cardiopulmonary, perioperative, and critical care; the council on clinical cardiology; and the stroke council. Circulation. 2008; 118:2452–83.6). Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part 9: post-cardiac arrest care 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010; 122:S768–86.7). Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3:63–81.8). Fugate JE, Wijdicks EF, Mandrekar J, Claassen DO, Manno EM, White RD, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. 2010; 68:907–14.
Article9). Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007; 33:237–45.
Article10). Scolletta S, Donadello K, Santonocito C, Franchi F, Taccone FS. Biomarkers as predictors of outcome after cardiac arrest. Expert Rev Clin Pharmacol. 2012; 5:687–99.
Article11). Morris M, Davey FR. Basic examination of blood. Clinical diagnosis and management by laboratory methods. 20th ed.Henry JB, editor. Philadelphia: W.B. Saunders Company;2001. p. 544–5.12). Demir A, Yarali N, Fisgin T, Duru F, Kara A. Most reliable indices in differentiation between thalassemia and trait and iron deficiency anemia. Pediatr Int. 2002; 44:612–6.13). Majercik S, Fox J, Knight S, Horne BD. Red cell distribution width is predictive of mortality in trauma patients. J Trauma Acute Care Surg. 2013; 74:1021–6.
Article14). Kim J, Kim K, Lee JH, Jo YH, Rhee JE, Kim TY, et al. Red blood cell distribution width as an independent predictor of all-cause mortality in out of hospital cardiac arrest. Resuscitation. 2012; 83:1248–52.
Article15). Lee JH, Chung HJ, Kim K, Jo YH, Rhee JE, Kim YJ, et al. Red cell distribution width as a prognostic marker in patients with community-acquired pneumonia. Am J Emerg Med. 2013; 31:72–9.
Article16). Slaughter E, Mount C, Schofield C. Changes in red blood cell width distribution as a novel biomarker for bacteremia. Crit Care Med. 2013; 41:A259.17). Kim CH, Park JT, Kim EJ, Han JH, Han JS, Choi JY, et al. An increase in red blood cell distribution width from baseline predicts mortality in patients with severe sepsis or septic shock. Critical Care. [serial on the internet]. 2013; Dec. [2013 Dec 9]. Available from http://ccforum.com/content/17/6/R282.
Article18). Cavusoglu E, Chopra V, Gupta A, Battala VR, Poludasu S, Eng C, et al. Relation between red blood cell distribution width (RDW) and all-cause mortality at two years in an unselected population referred for coronary angiography. Int J Cardiol. 2010; 141:141–6.
Article19). Al-Najjar Y, Goode KM, Zhang J, Cleland JG, Clark AL. Red cell distribution width: an inexpensive and powerful prognostic marker in heart failure. Eur J Heart Fail. 2009; 11:1155–62.
Article20). Chen PC, Sung FC, Chien KL, Hsu HC, Su TC, Lee YT. Red blood cell distribution width and risk of cardiovascular events and mortality in a community cohort in Taiwan. Am J Epidemiol. 2010; 171:214–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Mild Therapeutic Hypothermia on the non-Vf Cardiac arrest
- Clinical Implementation of Therapeutic Hypothermia after Cardiac Arrest
- A Report of Three Cases where Therapeutic Hypothermia was done After the Return of Spontaneous Circulation After Out-of-Hospital Cardiac Arrest in Children and Adolescents
- The Relationship between EEG Findings and Prognosis in Out-of-Hospital Cardiac Arrest Patients during Therapeutic Hypothermia
- The Relation between Time-weighted Mean Oxygen Tension and Outcome in Out-of-hospital Cardiac Arrest Survivors Treated with Therapeutic Hypothermia