Korean Circ J.
2012 Mar;42(3):184-191. 10.4070/kcj.2012.42.3.184.
The Effect of Enalapril and Carvedilol on Left Ventricular Dysfunction in Middle Childhood and Adolescent Patients With Muscular Dystrophy
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea. chungnoh@snu.ac.kr
- KMID: 2225032
- DOI: http://doi.org/10.4070/kcj.2012.42.3.184
Abstract
- BACKGROUND AND OBJECTIVES
In Duchenne and Becker muscular dystrophies, cardiac function deteriorates with time resulting in heart failure which is often fatal. We prospectively evaluated the effect of enalapril and carvedilol on left ventricular (LV) dysfunction in middle childhood and adolescent patients with muscular dystrophy.
SUBJECTS AND METHODS
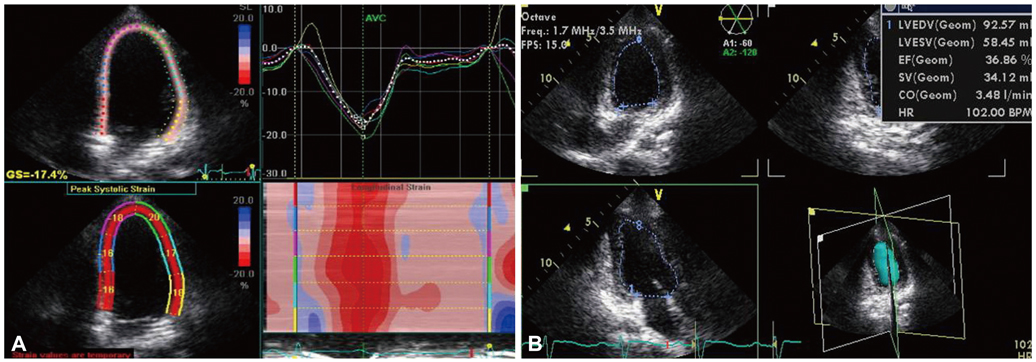
Twenty-three patients with LV dysfunction (22 with Duchenne muscular dystrophy, 1 with Becker muscular dystrophy) were enrolled. We prescribed enalapril (13 patients) or carvedilol (10 patients) randomly from July 2008 to August 2010 and followed up the patients until September 2011. The changes in LV function parameters before and after the treatment were evaluated by echocardiography.
RESULTS
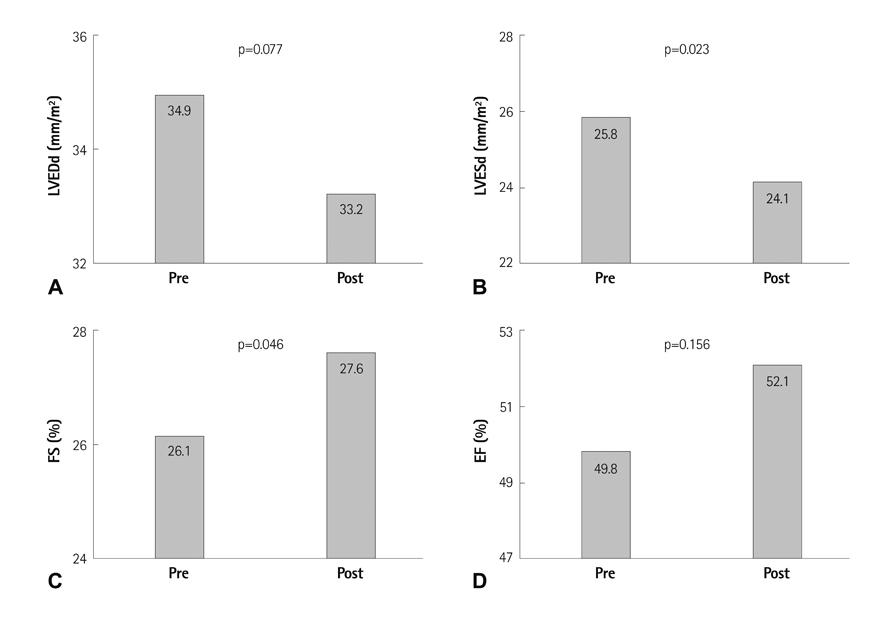
The mean age at the start of treatment with enalapril or carvedilol was 12.6+/-3.7 years (median 13 years), and mean follow-up duration was 20.1+/-8.9 months. In the enalapril group, LV fractional shortening (FS) increased from 25.8+/-2.1 to 26.6+/-3.0 (p=0.241). In the carvedilol group, LV FS increased from 26.4+/-1.1 to 28.6+/-4.2 (p=0.110). In all 23 patients, LV FS significantly increased from 26.1+/-1.7 (before) to 27.6+/-3.7 (after treatment) (p<0.046). Indexed LV dimension at end diastole and LV end-diastolic volume decreased slightly, but without statistical significance by tri-plane volumetry. LV diastolic functional parameters were maintained during follow-up period.
CONCLUSION
Enalapril or carvedilol could improve LV systolic function in middle childhood and adolescent patients with muscular dystrophy without significant adverse effects.
MeSH Terms
Figure
Reference
-
1. Emery AE. The muscular dystrophies. Lancet. 2002. 359:687–695.2. Emery AE. Population frequencies of inherited neuromuscular diseases: a world survey. Neuromuscul Disord. 1991. 1:19–29.3. Finsterer J, Stöllberger C. The heart in human dystrophinopathies. Cardiology. 2003. 99:1–19.4. McNally EM. Duchenne muscular dystrophy: how bad is the heart? Heart. 2008. 94:976–977.5. Kaspar RW, Allen HD, Montanaro F. Current understanding and management of dilated cardiomyopathy in Duchenne and Becker muscular dystrophy. J Am Acad Nurse Pract. 2009. 21:241–249.6. Jefferies JL, Eidem BW, Belmont JW, et al. Genetic predictors and remodeling of dilated cardiomyopathy in muscular dystrophy. Circulation. 2005. 112:2799–2804.7. Duboc D, Meune C, Lerebours G, Devaux JY, Vaksmann G, Bécane HM. Effect of perindopril on the onset and progression of left ventricular dysfunction in Duchenne muscular dystrophy. J Am Coll Cardiol. 2005. 45:855–857.8. Duboc D, Meune C, Pierre B, et al. Perindopril preventive treatment on mortality in Duchenne muscular dystrophy: 10 years' follow-up. Am Heart J. 2007. 154:596–602.9. Giglio V. Left ventricular function and response to enalapril in patients with Duchenne muscular dystrophy during the second decade of life. Am J Cardiol. 2007. 99:147–148.10. Saito T, Matsumura T, Miyai I, Nozaki S, Shinno S. Carvedilol effectiveness for left ventricular-insufficient patients with Duchenne muscular dystrophy. Rinsho Shinkeigaku. 2001. 41:691–694.11. Reisner SA, Lysyansky P, Agmon Y, Mutlak D, Lessick J, Friedman Z. Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr. 2004. 17:630–633.12. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978. 58:1072–1083.13. Garcia MJ, Thomas JD, Klein AL. New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol. 1998. 32:865–875.14. Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function: a study in normals and dilated cardiomyopathy. J Cardiol. 1995. 26:357–366.15. Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997. 30:474–480.16. Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man: anatomic validation of method. Circulation. 1977. 55:613–618.17. Lamparter S, Sun Y, Weber KT. Angiotensin II receptor blockade during gestation attenuates collagen formation in the developing rat heart. Cardiovasc Res. 1999. 43:165–172.18. Bernal J, Pitta SR, Thatai D. Role of the renin-angiotensin-aldosterone system in diastolic heart failure: potential for pharmacologic intervention. Am J Cardiovasc Drugs. 2006. 6:373–381.19. Ramaciotti C, Heistein LC, Coursey M, et al. Left ventricular function and response to enalapril in patients with Duchenne muscular dystrophy during the second decade of life. Am J Cardiol. 2006. 98:825–827.20. Francis GS, Benedict C, Johnstone DE, et al. Comparison of neuroendocrine activation in patients with left ventricular dysfunction with and without congestive heart failure: a substudy of the Studies of Left Ventricular Dysfunction (SOLVD). Circulation. 1990. 82:1724–1729.21. Cha DH, Cha YS, Kook JH, et al. Clinical efficacy of carvedilol in patients with moderate to severe congestive heart failure. Korean Circ J. 1998. 28:523–531.22. Bruns LA, Chrisant MK, Lamour JM, et al. Carvedilol as therapy in pediatric heart failure: an initial multicenter experience. J Pediatr. 2001. 138:505–511.23. Ishikawa Y, Bach JR, Minami R. Cardioprotection for Duchenne's muscular dystrophy. Am Heart J. 1999. 137:895–902.24. Kajimoto H, Ishigaki K, Okumura K, et al. Beta-blocker therapy for cardiac dysfunction in patients with muscular dystrophy. Circ J. 2006. 70:991–994.25. Ogata H, Ishikawa Y, Ishikawa Y, Minami R. Beneficial effects of beta-blockers and angiotensin-converting enzyme inhibitors in Duchenne muscular dystrophy. J Cardiol. 2009. 53:72–78.26. American Academy of Pediatrics Section on Cardiology and Cardiac Surgery. Cardiovascular health supervision for individuals affected by Duchenne or Becker muscular dystrophy. Pediatrics. 2005. 116:1569–1573.27. Bahler RC, Mohyuddin T, Finkelhor RS, Jacobs IB. Contribution of Doppler tissue imaging and myocardial performance index to assessment of left ventricular function in patients with Duchenne's muscular dystrophy. J Am Soc Echocardiogr. 2005. 18:666–673.28. Giatrakos N, Kinali M, Stephens D, Dawson D, Muntoni F, Nihoyannopoulos P. Cardiac tissue velocities and strain rate in the early detection of myocardial dysfunction of asymptomatic boys with Duchenne's muscular dystrophy: relationship to clinical outcome. Heart. 2006. 92:840–842.29. Ogata H, Nakatani S, Ishikawa Y, et al. Myocardial strain changes in Duchenne muscular dystrophy without overt cardiomyopathy. Int J Cardiol. 2007. 115:190–195.30. Tsutamoto T, Wada A, Maeda K, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997. 96:509–516.31. Mori K, Manabe T, Nii M, Hayabuchi Y, Kuroda Y, Tatara K. Plasma levels of natriuretic peptide and echocardiographic parameters in patients with Duchenne’s progressive muscular dystrophy. Pediatr Cardiol. 2002. 23:160–166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Becker Muscular Dystrophy Associated With Dilated Cardiomyopathy
- Electron Microscopic Study of Enalapril Effect on Left Ventricular Hypertrophy in Spontaneously Hypertensive Rat
- Two Cases of Oculopharyngeal Muscular Dystrophy in One Family
- A Clinical Study on Duchenne Muscular Dystrophy in Childhood
- A Case of Oculopharyngeal Muscular Dystrophy