Korean Circ J.
2014 Nov;44(6):400-405. 10.4070/kcj.2014.44.6.400.
Slow Coronary Flow Phenomenon and Increased Platelet Volume Indices
- Affiliations
-
- 1Department of Cardiology, Seyyed-al-Shohada Heart Center, Urmia University of Medical Sciences, Urmia, Iran. khademvatan2002@yahoo.com
- 2Department of Cardiology, Firoozgar Hospital, Iran University of Medical Sciences, Tehran, Iran.
- 3Seyyed-al-Shohada Heart Center, Urmia University of Medical Sciences, Urmia, Iran.
- KMID: 2223856
- DOI: http://doi.org/10.4070/kcj.2014.44.6.400
Abstract
- BACKGROUND AND OBJECTIVES
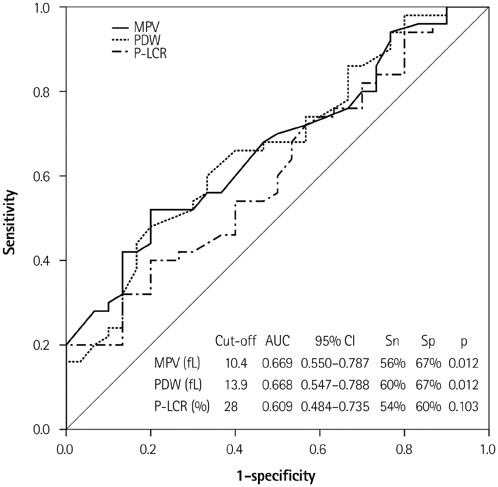
We sought to determine the relationship between mean platelet volume (MPV), platelet distribution width (PDW), and platelet larger cell ratio (P-LCR) with slow coronary flow (SCF).
SUBJECTS AND METHODS
Eighty participants who underwent coronary angiography were divided into two groups, 50 participants with SCF as case group, and 30 with normal coronary flow (NCF) as control group. Baseline characteristics and laboratory data were collected before angiography.
RESULTS
Platelet volume indices MPV (10.8+/-1.2 fL), PDW (14.5+/-2.2 fL), and P-LCR (30.5+/-8.1%) in the SCF group were significantly (p<0.05) higher than those (10.1+/-0.9 fL, 13.2+/-1.8 fL, and 26.8+/-6.8%, respectively) in the NCF group. The patients with three SCF arteries had significantly higher platelet volume indices compared to those with NCF arteries; however, the patients with one SCF artery did not. Based on linear regression model, MPV, PDW, and P-LCR were independent predictors of mean infarction frame counting (TFC). In multivariate analysis, MPV {odds ratio (OR)=32.393, 95% confidence interval (CI)=1.189-882.606, p=0.039} and P-LCR (OR=0.566, 95% CI=0.330-0.937, p=0.028) were independent predictors of SCF.
CONCLUSION
Platelet volume indices MPV, PDW, and P-LCR were associated with both the presence and extent of SCF.
Keyword
MeSH Terms
Figure
Reference
-
1. Goel PK, Gupta SK, Agarwal A, Kapoor A. Slow coronary flow: a distinct angiographic subgroup in syndrome X. Angiology. 2001; 52:507–514.2. Tambe AA, Demany MA, Zimmerman HA, Mascarenhas E. Angina pectoris and slow flow velocity of dye in coronary arteries--a new angiographic finding. Am Heart J. 1972; 84:66–71.3. Mosseri M, Yarom R, Gotsman MS, Hasin Y. Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation. 1986; 74:964–972.4. Li JJ, Qin XW, Li ZC, et al. Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow. Clin Chim Acta. 2007; 385:43–47.5. Turhan H, Saydam GS, Erbay AR, et al. Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow. Int J Cardiol. 2006; 108:224–230.6. Cakmak M, Tanriverdi H, Cakmak N, Evrengul H, Cetemen S, Kuru O. Simvastatin may improve myocardial perfusion abnormality in slow coronary flow. Cardiology. 2008; 110:39–44.7. Gökçe M, Kaplan S, Tekelioğlu Y, Erdoğan T, Küçükosmanoğlu M. Platelet function disorder in patients with coronary slow flow. Clin Cardiol. 2005; 28:145–148.8. Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007; 357:2482–2494.9. van der Loo B, Martin JF. A role for changes in platelet production in the cause of acute coronary syndromes. Arterioscler Thromb Vasc Biol. 1999; 19:672–679.10. Seyyed-Mohammadzad MH, Eskandari R, Rezaei Y, et al. Prognostic value of mean platelet volume in patients undergoing elective percutaneous coronary intervention. Anadolu Kardiyol Derg. 2014; DOI: 10.5152/akd.2014.5169.11. Celik T, Yuksel UC, Bugan B, et al. Increased platelet activation in patients with slow coronary flow. J Thromb Thrombolysis. 2010; 29:310–315.12. Vagdatli E, Gounari E, Lazaridou E, Katsibourlia E, Tsikopoulou F, Labrianou I. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia. 2010; 14:28–32.13. Grotto HZ, Noronha JF. Platelet larger cell ratio (P-LCR) in patients with dyslipidemia. Clin Lab Haematol. 2004; 26:347–349.14. Gibson CM, Cannon CP, Daley WL, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996; 93:879–888.15. Chu SG, Becker RC, Berger PB, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010; 8:148–156.16. Elsherbiny IA, Shoukry A, El Tahlawi MA. Mean platelet volume and its relation to insulin resistance in non-diabetic patients with slow coronary flow. J Cardiol. 2012; 59:176–181.17. Nurkalem Z, Alper AT, Orhan AL, et al. Mean platelet volume in patients with slow coronary flow and its relationship with clinical presentation. Turk Kardiyol Dern Ars. 2008; 36:363–367.18. Sen N, Basar N, Maden O, et al. Increased mean platelet volume in patients with slow coronary flow. Platelets. 2009; 20:23–28.19. Isik T, Ayhan E, Uyarel H, et al. Increased mean platelet volume associated with extent of slow coronary flow. Cardiol J. 2012; 19:355–362.20. Albayrak S, Ordu S, Yuksel H, Ozhan H, Yazgan O, Yazici M. Efficacy of nebivolol on flow-mediated dilation in patients with slow coronary flow. Int Heart J. 2009; 50:545–553.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coronary Slow Flow Phenomenon Leads to ST Elevation Myocardial Infarction
- Coronary Flow Doppler Profile in No-Reflex Phenomenon after Direct PTCA in Acute Myocardial Infarction
- Effects of Platelet Number and Platelet Indices on Platelet Reactivity in Patients Treated with Clopidogrel or Ticagrelor
- Evolution of Diastolic Dysfunction in Patients with Coronary Slow Flow Phenomenon and Acute Non-ST Segment Elevation Myocardial Infarction
- Slow flow and mural thrombus in aortic diseases: Spin-echo MR findings and their differentiation