Korean Circ J.
2015 Sep;45(5):408-415. 10.4070/kcj.2015.45.5.408.
Stepwise Approach Using Combined Management in Patients with Congenital Heart Disease and Borderline Pulmonary Vascular Disease
- Affiliations
-
- 1Department of Pediatrics, Department of Thoracic and Cardiovascular Surgery, Sejong Cardiovascular Institute, Bucheon, Korea.
- 2Department of Pediatrics, Konkuk University School of Medicine, Seoul, Korea. ksoojn@naver.com
- KMID: 2223805
- DOI: http://doi.org/10.4070/kcj.2015.45.5.408
Abstract
- BACKGROUND AND OBJECTIVES
Despite remarkable advances in pediatric cardiology, pulmonary arterial hypertension associated with congenital heart disease remains a major problem. In the past decade new vasodilators have been introduced and appear to be effective in reducing pulmonary vascular resistance (PVR).
SUBJECTS AND METHODS
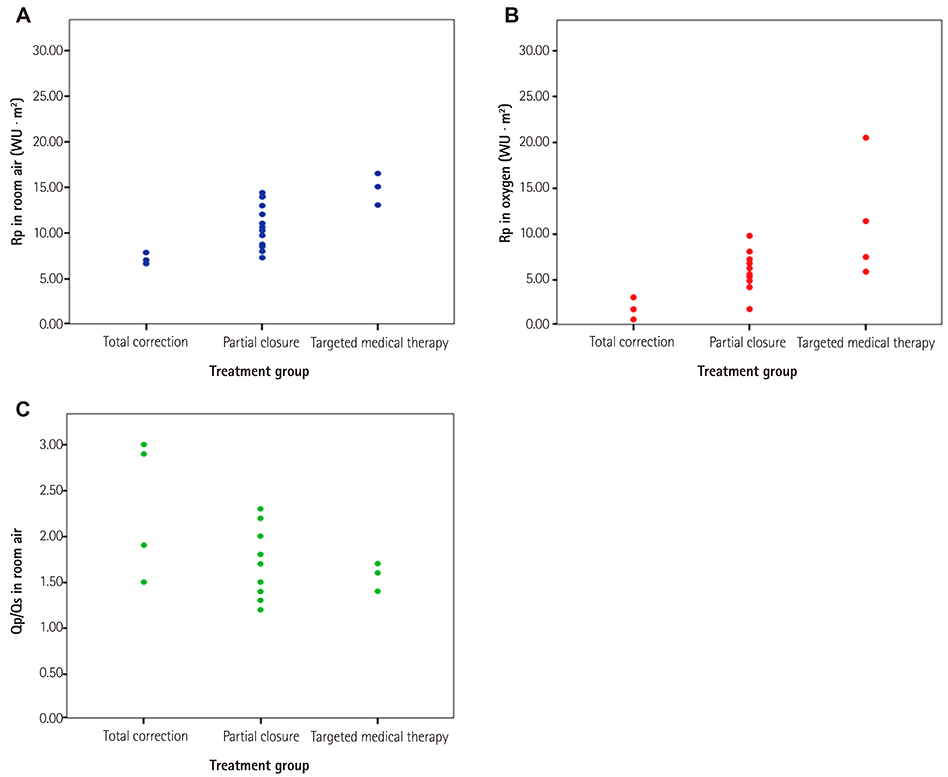
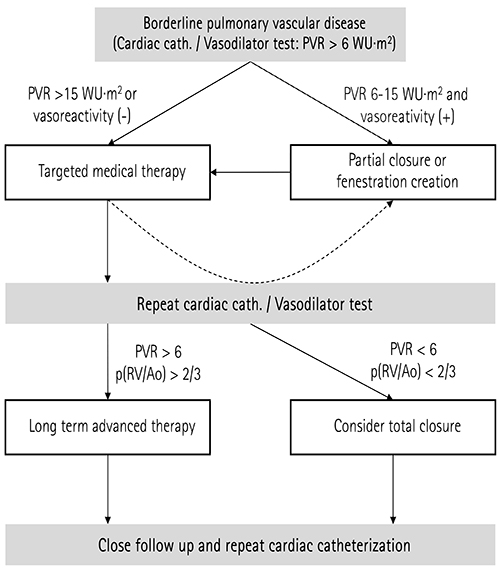
From 2000 to 2011, we retrospectively reviewed the records of 22 patients who had congenital septal defects and borderline pulmonary vascular disease (PVD). The PVR in these patients was from 6 to 16 wood units . m2, and/or the systolic pulmonary arterial pressure was more than 2/3 of the systemic arterial pressure.
RESULTS
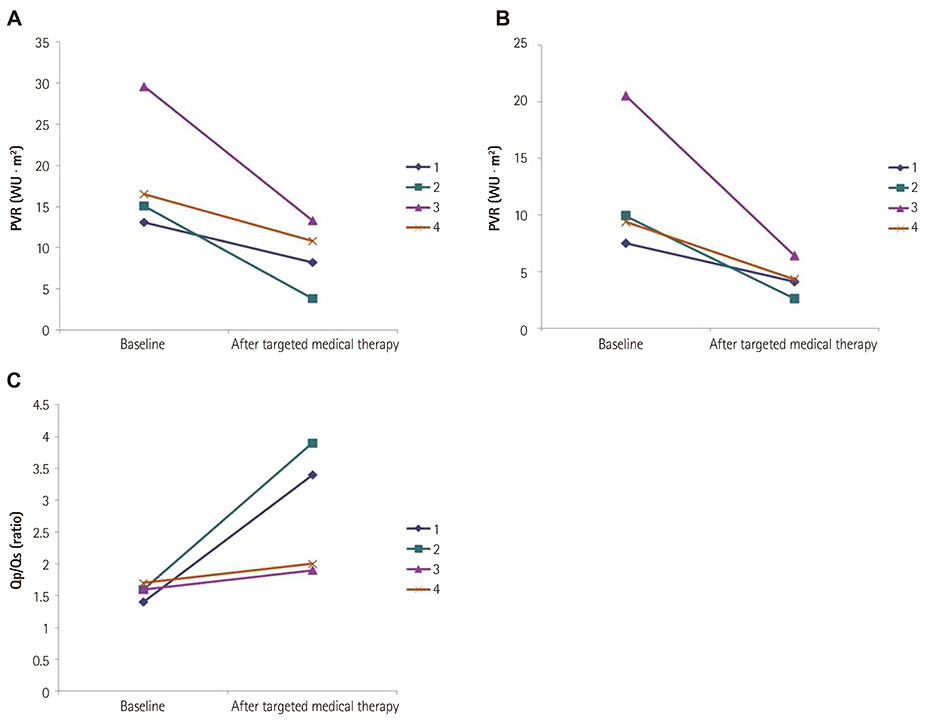
The median age was 16 years (range, 9 months-46 years). The median duration of follow-up was 7.4 years (range, 1.4-11.7 years). According to hemodynamic data and clinical symptoms, the initial management comprised targeted medical therapy in four (18%), complete closure in four (18%), and partial closure in 14 patients (63.6%). In the four patients who had a high PVR and negative vasoreactivity, the PVR decreased and vasoreactivity increased after targeted medical therapy; three of these patients underwent cardiac surgery later. Finally, 11 (50%) received targeted medical therapy and 21 patients (95.4%) underwent cardiac surgery. Complete closure resulted in six patients and partial closure in 17 patients. Mortality was observed in two patients. The other 19 patients (91%) had New York Heart Association functional class I.
CONCLUSION
Targeted medical therapy may be effective in reducing PVR in patients with congenital heart disease and borderline PVD. A stepwise approach may help to achieve improved outcomes in these patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Galiè N, Torbicki A, Barst R, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The task force on diagnosis and treatment of pulmonary arterial hypertension of the European Society of Cardiology. Eur Heart J. 2004; 25:2243–2278.2. Farber HW, Loscalzo J. Pulmonary arterial hypertension. N Engl J Med. 2004; 351:1655–1665.3. McLaughlin VV, Genthner DE, Panella MM, Rich S. Reduction in pulmonary vascular resistance with long-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension. N Engl J Med. 1998; 338:273–277.4. Rosenzweig EB, Kerstein D, Barst RJ. Long-term prostacyclin for pulmonary hypertension with associated congenital heart defects. Circulation. 1999; 99:1858–1865.5. Ghofrani HA, Wiedemann R, Rose F, et al. Sildenafil for treatment of lung fibrosis and pulmonary hypertension: a randomised controlled trial. Lancet. 2002; 360:895–900.6. LaFarge CG, Miettinen OS. The estimation of oxygen consumption. Cardiovasc Res. 1970; 4:23–30.7. Jin H, Yang J, Zhang Q, Du J. Epidemiology and clinical management of pulmonary hypertension in children. Korean Circ J. 2012; 42:513–518.8. Dimopoulos K, Peset A, Gatzoulis MA. Evaluating operability in adults with congenital heart disease and the role of pretreatment with targeted pulmonary arterial hypertension therapy. Int J Cardiol. 2008; 129:163–171.9. Steele PM, Fuster V, Cohen M, Ritter DG, McGoon DC. Isolated atrial septal defect with pulmonary vascular obstructive disease--long-term follow-up and prediction of outcome after surgical correction. Circulation. 1987; 76:1037–1042.10. Rabinovitch M, Haworth SG, Castaneda AR, Nadas AS, Reid LM. Lung biopsy in congenital heart disease: a morphometric approach to pulmonary vascular disease. Circulation. 1978; 58:1107–1122.11. Balzer DT, Kort HW, Day RW, et al. Inhaled nitric oxide as a preoperative test (INOP Test I): the INOP Test Study Group. Circulation. 2002; 106:12 Suppl 1. I76–I81.12. Sitbon O, Humbert M, Jaïs X, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation. 2005; 111:3105–3111.13. Ivy DD, Abman SH, Barst RJ, et al. Pediatric pulmonary hypertension. J Am Coll Cardiol. 2013; 62:25 Suppl. D117–D126.14. Galiè N, Beghetti M, Gatzoulis MA, et al. Bosentan therapy in patients with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation. 2006; 114:48–54.15. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004; 351:1425–1436.16. Schwerzmann M, Zafar M, McLaughlin PR, Chamberlain DW, Webb G, Granton J. Atrial septal defect closure in a patient with "irreversible" pulmonary hypertensive arteriopathy. Int J Cardiol. 2006; 110:104–107.17. Frost AE, Quiñones MA, Zoghbi WA, Noon GP. Reversal of pulmonary hypertension and subsequent repair of atrial septal defect after treatment with continuous intravenous epoprostenol. J Heart Lung Transplant. 2005; 24:501–503.18. Yamauchi H, Yamaki S, Fujii M, Iwaki H, Tanaka S. Reduction in recalcitrant pulmonary hypertension after operation for atrial septal defect. Ann Thorac Surg. 2001; 72:905–906. discussion 906-719. Eicken A, Balling G, Gildein HP, Genz T, Kaemmerer H, Hess J. Transcatheter closure of a non-restrictive patent ductus arteriosus with an Amplatzer muscular ventricular septal defect occluder. Int J Cardiol. 2007; 117:e40–e42.20. Khan SA, Gelb BD, Nguyen KH. Evaluation of pulmonary artery banding in the setting of ventricular septal defects and severely elevated pulmonary vascular resistance. Congenit Heart Dis. 2006; 1:244–250.21. Marie Valente A, Rhodes JF. Current indications and contraindications for transcatheter atrial septal defect and patent foramen ovale device closure. Am Heart J. 2007; 153:4 Suppl. 81–84.22. Allcock RJ, O'Sullivan JJ, Corris PA. Atrial septostomy for pulmonary arterial hypertension. Heart. 2003; 89:1344–1347.23. Diller GP, Dimopoulos K, Kaya MG, et al. Long-term safety, tolerability and efficacy of bosentan in adults with pulmonary arterial hypertension associated with congenital heart disease. Heart. 2007; 93:974–976.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Arterial Hypertension with Congenital Heart Diseases
- Pulmonary Arterial Hypertension of Congenital Heart Diseases: From Reversible Pulmonary Hypertension to Eisenmenger Syndrome
- Nitric oxide and pulmonary hypertension
- Comparatives Study of Pulmonary Artery and Pulmonary Venous Wedge Pressure in Congenital Heart Disease
- Clinical Year in Review of Pulmonary Vascular Disease