J Rheum Dis.
2011 Sep;18(3):203-207. 10.4078/jrd.2011.18.3.203.
A Case of Dermatomyositis Presenting with Rhabdomyolysis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. tykang@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2223151
- DOI: http://doi.org/10.4078/jrd.2011.18.3.203
Abstract
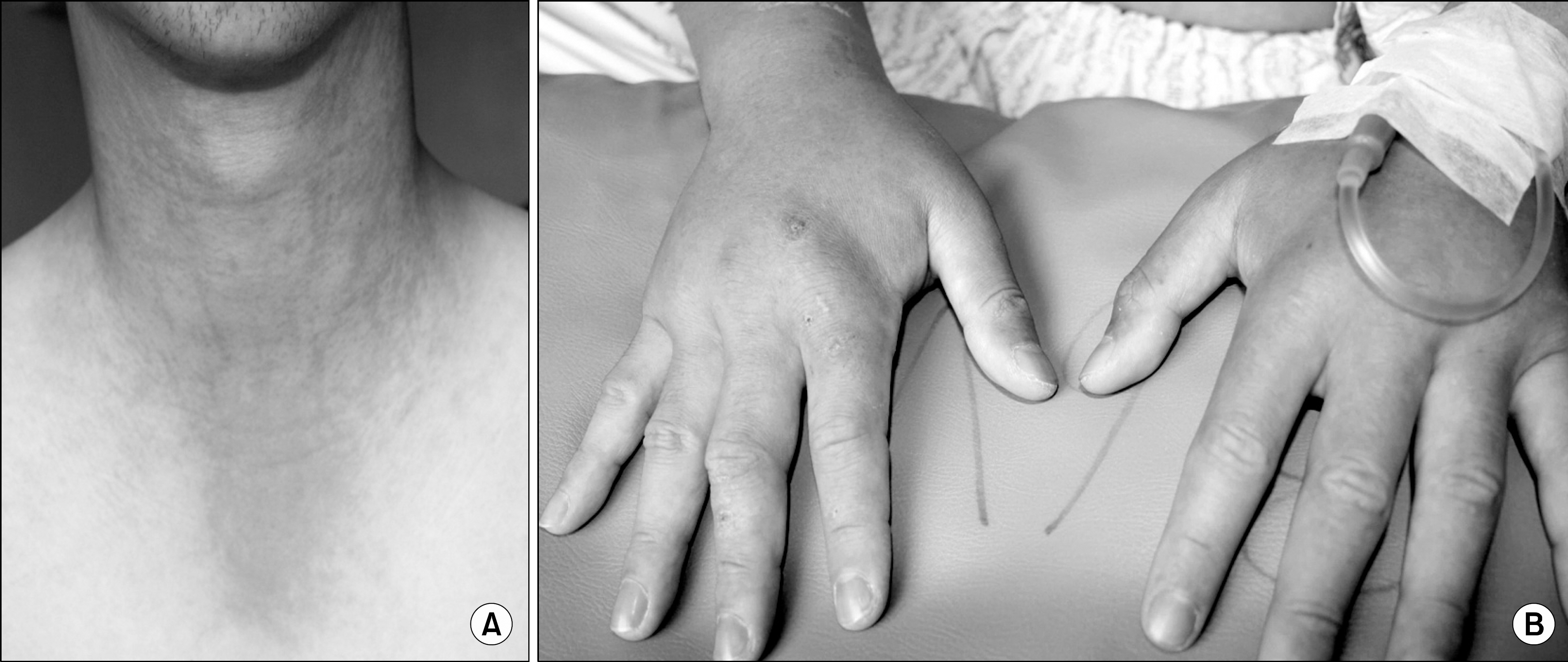
- Rhabdomyolysis is caused by injury to skeletal muscle and it involves leakage of intracellular contents into the plasma. Rhabdomyolysis is an extremely rare manifestation of dermatomyositis. Dermatomyositis is a rare idiopathic inflammatory myopathy that is characterized by chronic inflammation of skeletal muscles and skin, resulting in muscle weakness. A 20 year old Korean male soldier presented with acute muscle pain, weakness and skin rashes over the face, neck and anterior chest. He received military training with carrying a radio set one week previouslyago. The patient was treated for rhabdomyolysis. However, the patient's symptoms did not improve. Muscle biopsy results suggested the diagnosis of rhabdomyolysis. Nevertheless, the features of skin and muscle inflammation raised the possibility of dermatomyositis. High dose steroid treatment was started, and then the symptoms and signs of muscle inflammation were improved. Rhabdomyolysis as the presenting sign of dermatomyositis has not been reported in Korea. Thus, we report on this case with a literature review.
MeSH Terms
Figure
Reference
-
References
1. Warren JD, Blumbergs PC, Thompson PD. Rhabdomyolysis: a review. Muscle Nerve. 2002; 25:332–47.
Article2. Luck RP, Verbin S. Rhabdomyolysis: a review of clinical presentation, etiology, diagnosis, and management. Pedi-atr Emerg Care. 2008; 24:262–8.3. Joshi D, Kumar N, Rai A. Dermatomyositis presenting with rhabdomyolysis and acute renal failure; an uncommon manifestation. Ann Indian Acad Neurol. 2009; 12:45–7.4. Kofteridis DP, Malliotakis PI, Sotsiou F, Vardakis NK, Vamvakas LN, Emmanouel DS. Acute onset of dermatomyositis presenting in pregnancy with rhabdomyolysis and fetal loss. Scand J Rheumatol. 1999; 28:192–4.5. Marks SH, McShane DJ, Mitchell DM. Dermatomyositis following rhabdomyolysis. J Rheumatol. 1976; 3:224–6.6. Yum JH, Jung YK, Kim YH, Ahn BJ, Son JH, Jeon YD, et al. A case of acute renal failure due to rhabdomyolysis associated with dermatomyositis in breast cancer. Korean J Nephrol. 1999; 18:334–8.7. Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975; 292:403–7.8. Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975; 292:344–7.9. Gerami P, Schope JM, McDonald L, Walling HW, Sontheimer RD. A systematic review of adult-onset clinically amyopathic dermatomyositis (dermatomyositis siné myositis): a missing link within the spectrum of the idiopathic inflammatory myopathies. J Am Acad Dermatol. 2006; 54:597–613.
Article10. Kim SM, Choi YH, OH MD, Nam TS, Chung MH, Pai HJ, et al. A clinical analysis of 100 patients with dermatomyositis-polymyositis. Korean J Med. 1990; 39:812–22.11. Feldman BM, Reichlin M, Laxer RM, Targoff IN, Stein LD, Silverman ED. Clinical significance of specific auto-antibodies in juvenile dermatomyositis. J Rheumatol. 1996; 23:1794–7.12. Santos J Jr. Exertional rhabdomyolysis. Potentially life- threatening consequence of intense exercise. JAAPA. 1999; 12:46–9. 53-5.13. Khan FY. Rhabdomyolysis: a review of the literature. Neth J Med. 2009; 67:272–83.14. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis - an overview for clinicians. Crit Care. 2005; 9:158–69.15. Ahn YJ, Yi SR, Yoo JH, Zoo MH, Kim SW, Park JM, et al. Clinical study of rhabdomyolysis after exercise. J Korean Orthop Sports Med. 2007; 6:110–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermatomyositis First Presenting as Panniculitis
- A Case of Acute Renal Failure due to Rhabdomyolysis Associated with Dermatomyositis in Breast Cancer
- A case of morphine induced rhabdomyolysis
- Amyopathic Dermatomyositis with Interstitial Lung Disease: A Case Report
- Dermatomyositis Presenting with Isolated Dysphagia: A Case Report