J Korean Ophthalmol Soc.
2014 Mar;55(3):437-442. 10.3341/jkos.2014.55.3.437.
A Case of Autologous Tragal Perichondrium Graft in a Patient with Mooren's Ulcer
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea. jck50ey@kornet.net
- KMID: 2218276
- DOI: http://doi.org/10.3341/jkos.2014.55.3.437
Abstract
- PURPOSE
To report the effectiveness of an autologous tragal perichondrium graft for an active Mooren's ulcer.
CASE SUMMARY
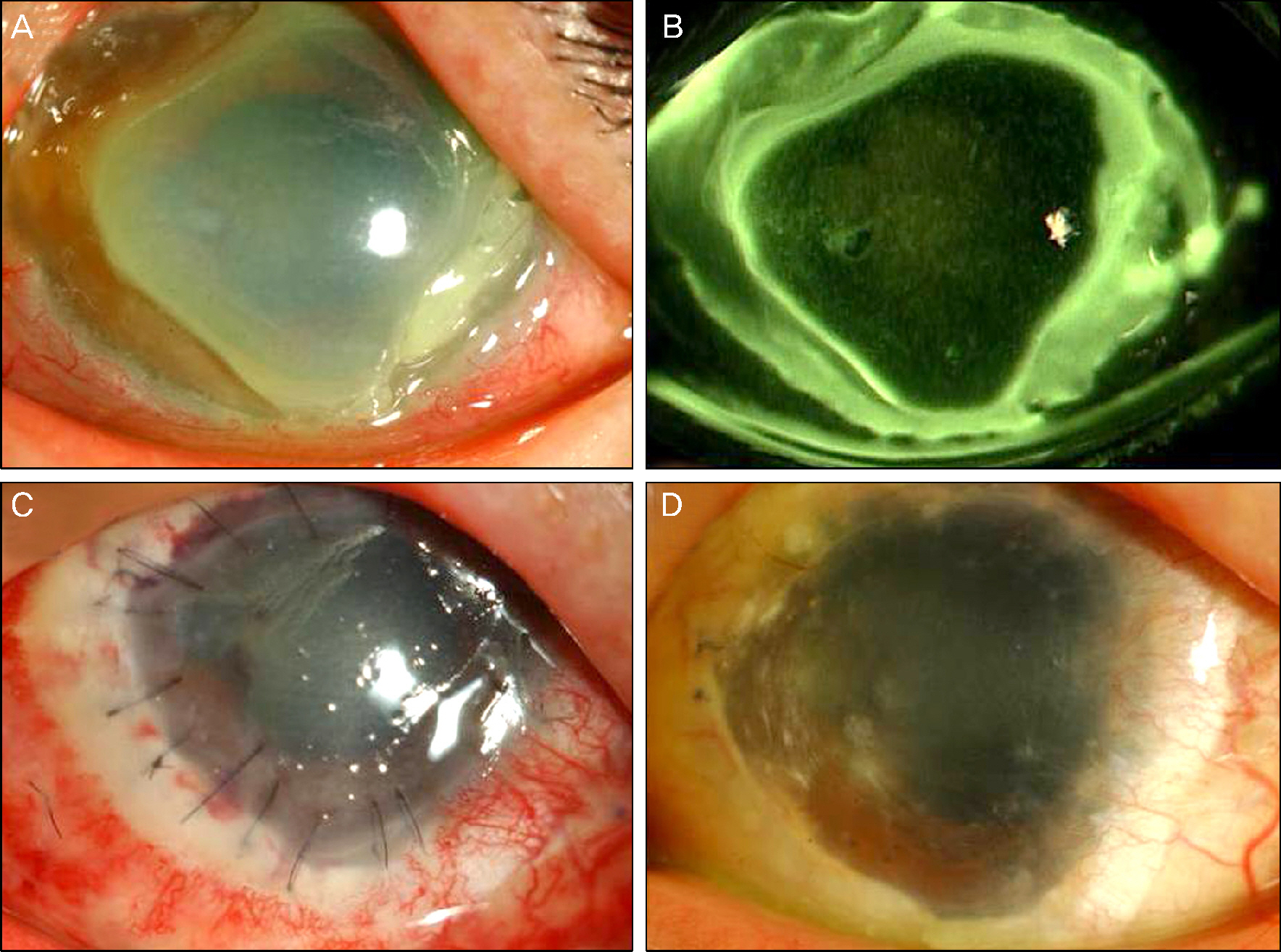
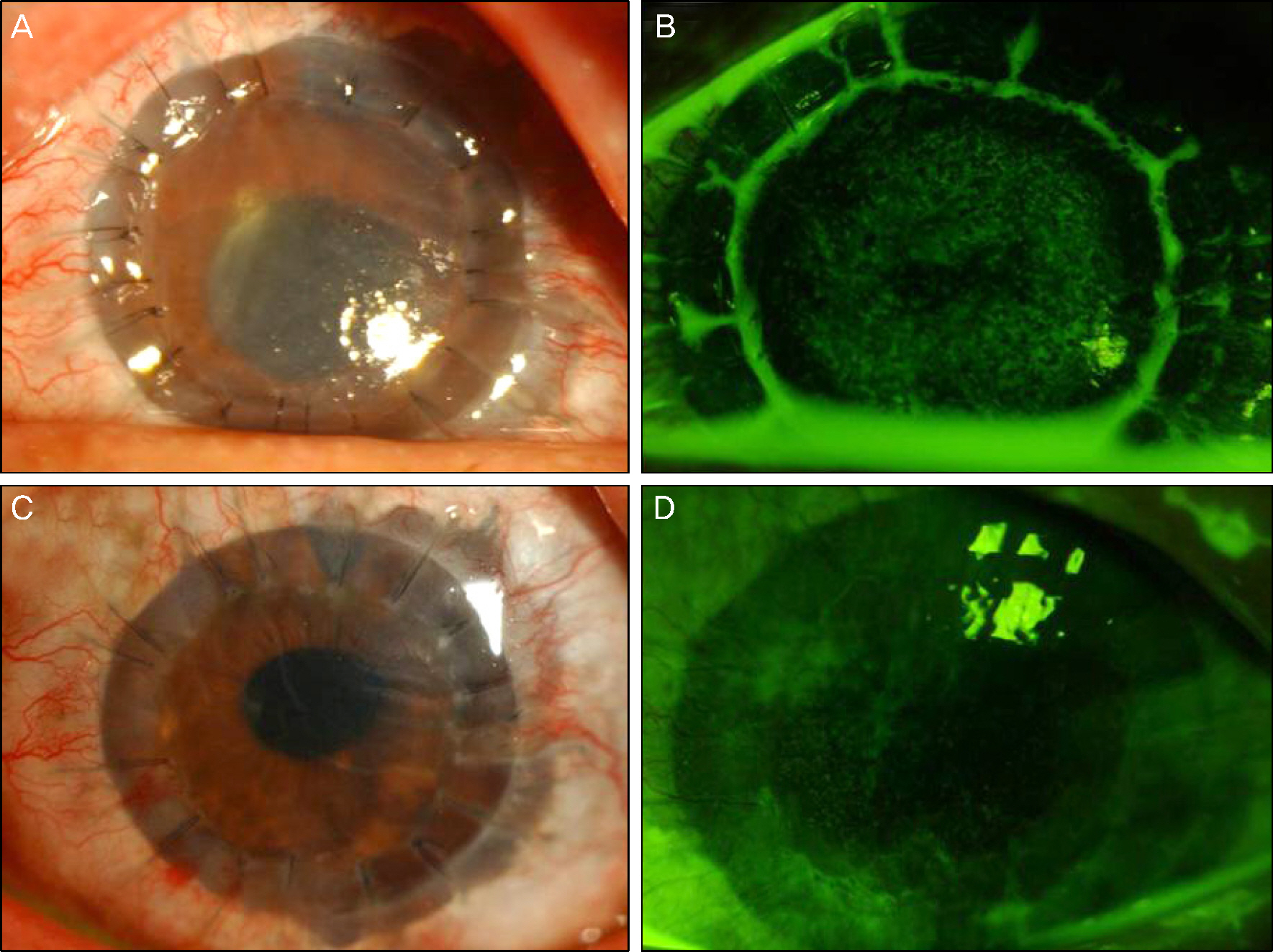
A 49-year-old male was referred to our clinic with Mooren's ulcer in his left eye. On the first visit, the ulcer involved the entire 360 degrees of the peripheral cornea and the visual acuity was 0.04. As the ulcer did not respond to medical treatment and progressed rapidly, the authors decided on surgical treatment. First, the involved cornea and nearby conjunctiva were removed and the defect was successfully reconstructed with autologous tragal perichondrium and allogenic limbal graft. The progression of corneal ulceration ceased after surgery and the patient's symptoms remarkably improved. Additionally, the graft showed rapid vascularization and engraftment within a week. However, as the opacity evolved and progressed to the central cornea, penetrating keratoplasty (PKP) was performed 5 months after the perichondrial graft. There was no rejection and corneal translucency was kept clear with low-dose steroid eye drops until 6 months after PKP without any sign of limbal deficiency. The patient's final best corrected visual acuity was 0.125.
CONCLUSIONS
The present study shows that autologous tragal perichondrium graft is an effective method of treatment for active Mooren's ulcer by defect reconstruction and results in survival of the co-transplanted graft as well as maintaining corneal functions.
MeSH Terms
Figure
Cited by 1 articles
-
A Two Case of 360 Degree Keratolimbal Allograft
Hong Kyu Kim, Kyung Jin Cho
J Korean Ophthalmol Soc. 2015;56(3):432-437. doi: 10.3341/jkos.2015.56.3.432.
Reference
-
References
1. Sangwan VS, Zafirakis P, Foster CS. Mooren's ulcer: current concepts in management. Indian J Ophthalmol. 1997; 45:7–17.2. Watson PG. Management of Mooren's ulceration. Eye (Lond). 1997; 11:349–56.
Article3. Foster CS, Azar DT, Dohlman CH. Mooren's ulcer. Smolin , Thoft , editors. The Cornea. 4th ed.Philadelphia: Lippincott Williams & Wilkins;2005. v. 1:chap. 24.4. Lambiase A, Sacchetti M, Sgrulletta R, et al. Amniotic membrane transplantation associated with conjunctival peritomy in the management of Mooren's ulcer: a case report. Eur J Ophthalmol. 2005; 15:274–6.
Article5. Dingeldein SA, Insler MS, Barron BA, Kaufman H. Mooren's ulcer treated with a periosteal graft. Ann Ophthalmol. 1990; 22:56–7.6. Cavaliere M, Mottola G, Rondinelli M, Iemma M. Tragal cartilage in tympanoplasty: anatomic and functional results in 306 cases. Acta Otorhinolaryngol Ital. 2009; 29:27–32.7. Yoon CH, Kim NJ, Lee MJ, et al. Correction of lower lid retraction using autologous ear cartilage graft. J Korean Ophthalmol Soc. 2011; 52:136–40.
Article8. Nigro MV, Friedhofer H, Natalino RJ, Ferreira MC. Comparative analysis of the influence of perichondrium on conjunctival epithelialization on conchal cartilage grafts in eyelid reconstruction: experimental study in rabbits. Plast Reconstr Surg. 2009; 123:55–63.
Article9. Chow CY, Foster CS. Mooren's Ulcer. Int Ophthalmol Clin. 1996; 36:1–13.
Article10. Kim MJ, Wee WR, Kee JH, Kim MK. The amniotic membrane transplantation in corneal perforation due to Mooren's Ulcer. J Korean Ophthalmol Soc. 2007; 48:438–44.11. Solomon A, Pires RT, Tseng SC. Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology. 2001; 108:449–60.
Article12. Togo T, Utani A, Naitoh M, et al. Identification of cartilage progen-itor cells in the adult ear perichondrium: utilization for cartilage reconstruction. Lab Invest. 2006; 86:445–57.
Article13. Kicic A, Shen W, Rakoczy PE. The potential of marrow stromal cells in stem cell therapy. Eye (Lond). 2001; 15:695–707.
Article14. Park SH, Chun YS, Kim JC. Effective keratocyte culture using amniotic membrane matrix and differentiation of mesenchymal stem cells. J Korean Ophthalmol Soc. 2010; 51:1652–8.
Article15. Duffy MM, Ritter T, Ceredig R, Griffin MD. Mesenchymal stem cell effects on T-cell effector pathways. Stem Cell Res Ther. 2011; 2:34.
Article16. Lee JY, Kim MK, Wee WR. Two cases of whole corneo-limbal transplantation. J Korean Ophthalmol Soc. 2011; 52:1238–43.
Article17. Kim KW, Chun YS, Kim JC. Autologous tragal perichondrium transplantation: a novel approach for the management of painful bullous keratopathy. Korean J Ophthalmol. 2013; 27:149–57.
Article18. Sandinha T, Zaher SS, Roberts F, et al. Superior forniceal conjunctival advancement pedicles (SFCAP) in the management of acute and impending corneal perforations. Eye (Lond). 2006; 20:84–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ocular Reconstruction Using Autologous Tragal Perichondrium for a Refractory Necrotizing Scleral Perforation: A Case Report
- Efficacy of Autologous Tragal Perichondrium Graft after Proper Antifungal Treatment in Fungal Necrotizing Scleritis
- Autologous Tragal Perichondrium Transplantation: A Novel Approach for the Management of Painful Bullous Keratopathy
- Simultaneous Four-site Restoration of Bilateral Scleromalacia Using Autologous Tragal Perichondrium and Preserved Sclera
- The Successful Treatment of Case of Mooren's Ulcer