J Korean Ophthalmol Soc.
2013 Mar;54(3):540-544. 10.3341/jkos.2013.54.3.540.
A Case of Invasive Aspergillosis Involving the Orbital Apex and Occipital Lobe:Successful Treatment with Voriconazole
- Affiliations
-
- 1Department of Ophthalmology, Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea. limkh@ewha.ac.kr
- 2Department of Pathology, Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2216780
- DOI: http://doi.org/10.3341/jkos.2013.54.3.540
Abstract
- PURPOSE
To report an immunocompetent patient with more than 1-year survival after treatment with voriconazole, despite invasive paranasal sinus aspergillosis involving the orbital apex.
CASE SUMMARY
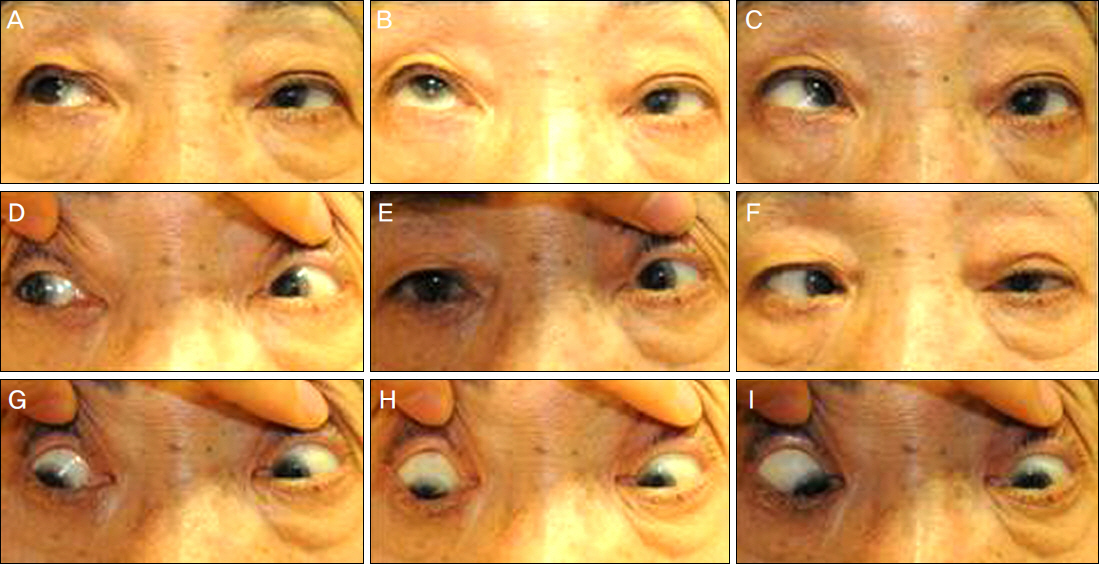
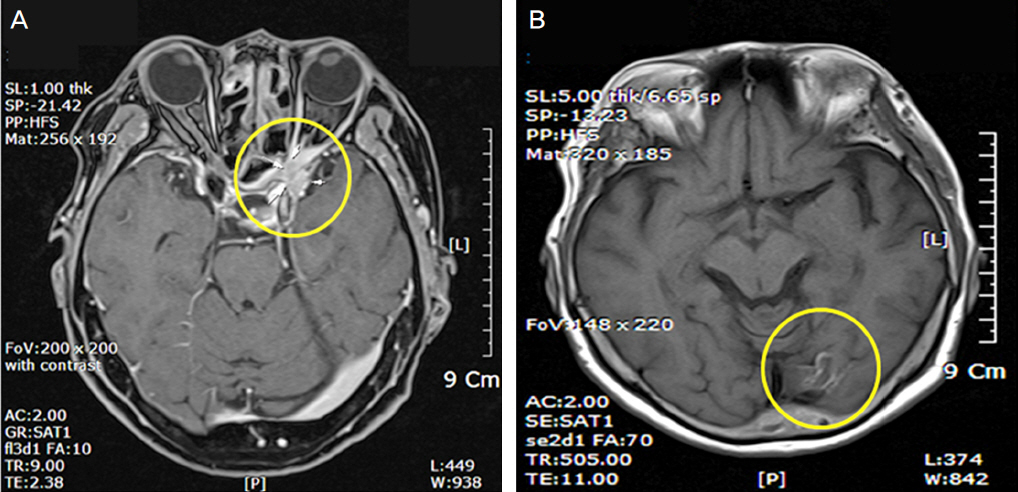
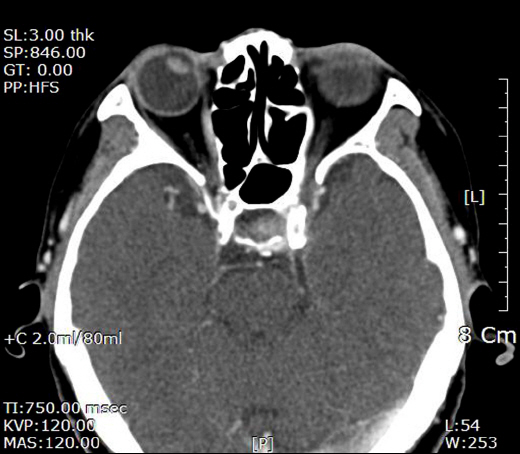
A 74-year-old woman with only preexisting hypertension visited our clinic complaining of pain and immovable left eye that occurred approximately 4 days prior. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a sphenoid sinusitis with suspicious lesion involving the orbital apex of the left eye. A biopsy by functional endoscopic sphenoid surgery (FESS) was performed through the sphenoid sinus, which enabled us to diagnose aspergillosis. The patient had esotropia, ophthalmoplegia, positive RAPD, and ptosis in the left eye. On follow-up, a new MRI showed acute to subacute stage infarction at the left occipital lobe. After the patient was treated with intravenous voriconazole, ptosis, and ophthalmoplegia improved. At the 13-month follow-up, she was alive with no disease recurrence.
CONCLUSIONS
Invasive aspergillosis of orbit and cerebrum in healthy patients is a rare clinical entity. In case of central nervous system involvement, the survival outcome is poor with high mortality; however, good results can be obtained by treatment with voriconazole.
MeSH Terms
Figure
Cited by 1 articles
-
A Case of the Third, Fourth, and Sixth Nerve Palsy in a Patient with Cerebral Aspergillosis
Sung Soo Hwang, Soo Jung Lee
J Korean Ophthalmol Soc. 2015;56(3):471-476. doi: 10.3341/jkos.2015.56.3.471.
Reference
-
References
1. Shamim MS, Siddiqui AA, Enam SA, et al. Craniocerebral aspergillosis in immunocompetent hosts: surgical perspective. Neurol India. 2007; 55:274–81.
Article2. Kim DG, Hong SC, Kim HJ, et al. Cerebral aspergillosis in immunologically competent patients. Surg Neurol. 1993; 40:326–31.
Article3. Myoken Y, Sugata T, Kyo TI, Fujihara M. Pathological features of invasive oral aspergillosis in patients with hematologic malignancies. J Oral Maxillofac Surg. 1996; 54:263–70.4. Alrajhi AA, Enani M, Mahasin Z, Al-Omran K. Chronic invasive aspergillosis of the paranasal sinuses in immunocompetent hosts from Saudi Arabia. Am J Trop Med Hyg. 2001; 65:83–6.
Article5. Lee DC, Lee JH, Choi WS. A case of the sino-orbital-cerebral aspergillosis. J Korean Ophthalmol Soc. 1999; 40:1678–83.6. Aisner J, Schimpff SC, Bennett JE, et al. Aspergillus infection in cancer patients. Association with fireproofing materials in a new hospital. JAMA. 1976; 235:411–2.7. Sivak-Callcott JA, Livesley N, Nugent RA, et al. Localised invasive sino-orbital aspergillosis: characteristic features. Br J Ophthalmol. 2004; 88:681–7.
Article8. Groll AH, Shah PM, Mentzel C, et al. Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect. 1996; 33:23–32.
Article9. Miyabe S, Koizuka I, Ochi K, et al. Two cases of Aspergillus sinusitis with bone destruction. Auris Nasus Larynx. 2003; 30:S115–21.
Article10. Johnson TE, Casiano RR, Kronish JW, et al. Sino-orbital aspergil-losis in acquired immunodeficiency syndrome. Arch Ophthalmol. 1999; 117:57–64.
Article11. Chopra H, Dua K, Malhotra V, et al. Invasive fungal sinusitis of isolated sphenoid sinus in immunocompetent subjects. Mycoses. 2006; 49:30–6.
Article12. Siddiqui AA, Shah AA, Bashir SH. Craniocerebral aspergillosis of sinonasal origin in immunocompetent patients: clinical spectrum and outcome in 25 cases. Neurosurgery. 2004; 55:602–11. discussion 611-3.
Article13. Wipfler P, Pilz G, Golaszewski S, et al. Invasive aspergillosis presenting with a painless complete ophthalmoplegia. Clin Neurol Neurosurg. 2010; 112:85–7.
Article14. Siddiqui AA, Bashir SH, Shah AA, Enam SA. Complications in craniocerebral aspergillosis of sino-nasal origin in immunocompetent patients. Pan Arab journal of neurosurgery : official journal of Pan Arab Neurosurgical Society. 2010; 14:99–103.15. Gupta AK, Mann SB, Khosla VK, et al. Non-randomized comparison of surgical modalities for paranasal sinus mycoses with intracranial extension. Mycoses. 1999; 42:225–30.16. Streppel M, Bachmann G, Arnold G, et al. Successful treatment of an invasive aspergillosis of the skull base and paranasal sinuses with liposomal amphotericin B and intraconazole. Ann Otol Rhinol Laryngol. 1999; 108:205–7.17. Espinel-Ingroff A, Boyle K, Sheehan DJ. In vitro antifungal activities of voriconazole and reference agents as determined by NCCLS methods: review of the literature. Mycopathologia. 2001; 150:101–15.18. Diekema DJ, Messer SA, Hollis RJ, et al. Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J Clin Microbiol. 2003; 41:3623–6.
Article19. Baumann A, Zimmerli S, Hausler R, Caversaccio M. Invasive sphenoidal aspergillosis: successful treatment with sphenoidotomy and voriconazole. ORL J Otorhinolaryngol Relat Spec. 2007; 69:121–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Aspergillosis of the Paranasal Sinuses Invading Skull Base : Successful Treatment with Voriconazole
- New Treatment for Isolated Invasive Aspergillosis of Sphenoid Sinus in Immunocompetent Subjects: Sphenoid Nasalization Combined with Voriconazole
- One Case of Invasive bone Aspergillosis
- Invasive Aspergillosis Complicated by Occlusion of Internal Carotid Artery and Cerebral Infarction
- Voriconazole-refractory invasive aspergillosis