J Korean Ophthalmol Soc.
2013 Jan;54(1):160-164. 10.3341/jkos.2013.54.1.160.
A Case of IgG4-Related Sclerosing Disease Involving the Eyelid in an Idiopathic Sclerosing Myositis Patient
- Affiliations
-
- 1Department of Ophthalmology, Gachon University Gil Medical Center, Incheon, Korea. cmj@gilhospital.com
- KMID: 2216466
- DOI: http://doi.org/10.3341/jkos.2013.54.1.160
Abstract
- PURPOSE
To report a case of IgG4-related sclerosing disease involving the eyelid in an idiopathic sclerosing myositis patient.
CASE SUMMARY
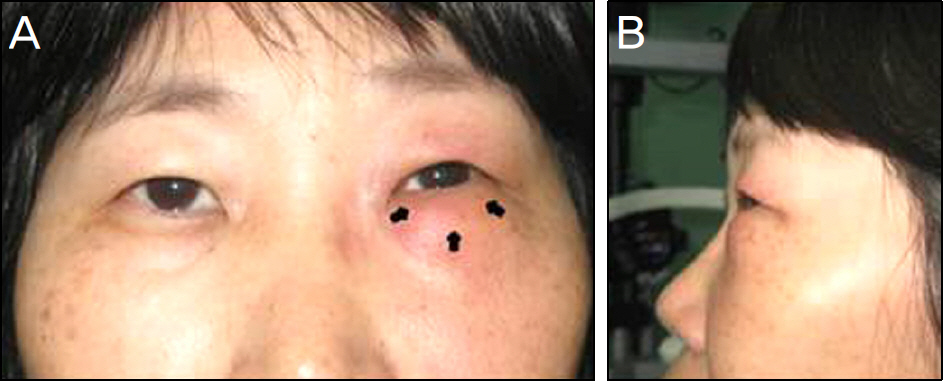
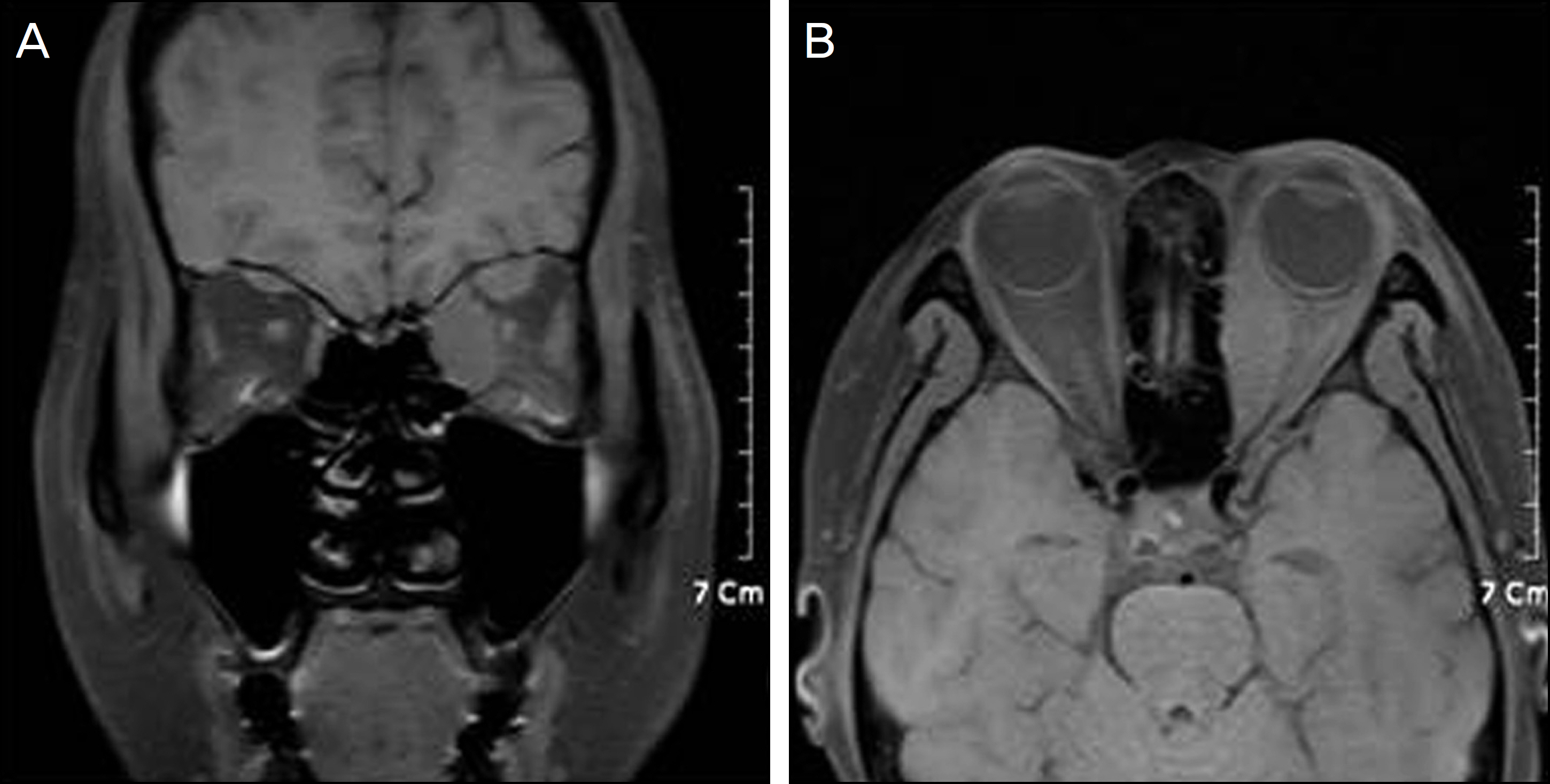
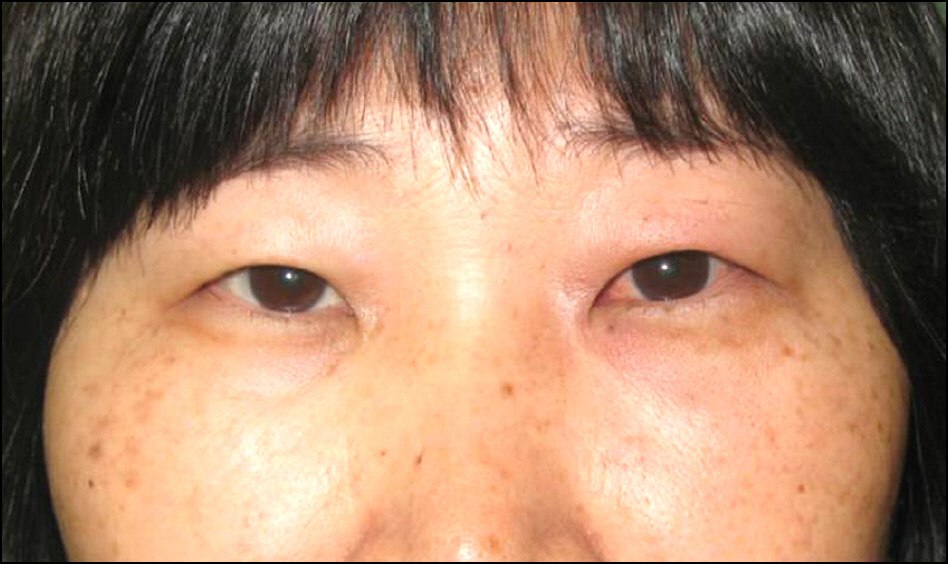
A 51-year-old woman presented with swelling, redness, and tenderness of the left lower eyelid of 1 month duration had taken an immunosuppressant for idiopathic sclerosing myositis. Eye movements showed limitation all directions but there was no exophthalmos. A palpable mass was noted in the left lower eyelid. The left extraocular muscles were hypertrophied but the lacrimal gland was normal on orbital magnetic resonance imaging. IgG4-related sclerosing disease was confirmed by immunostained biopsy from the left lower eyelid, showing infiltration of IgG4-positive lymphoplasmacytic cells. The patient was given oral steroids and an immunosuppressant and the symptoms did not recur for at least 7 months.
CONCLUSIONS
IgG4-related sclerosing disease involving ocular adnexa usually consists of bilateral lacrimal gland involvement. Additionally, the orbital soft tissue involvement without dacryoadenitis is rare. The authors of the present study report a case of IgG4-related sclerosing disease involving the left lower eyelid in an idiopathic sclerosing myositis patient and should be considered in the differential diagnosis of eyelid masses.
MeSH Terms
Figure
Cited by 1 articles
-
IgG4-related Ophthalmic Disease Associated with Adult Xanthogranulomatous Disease
Seunghyun Lee, Sokjoong Chung, Jinhyung Heo, Helen Lew
J Korean Ophthalmol Soc. 2018;59(11):1071-1076. doi: 10.3341/jkos.2018.59.11.1071.
Reference
-
References
1. Plaza JA, Garrity JA, Dogan A, et al. Orbital inflammation with IgG4-positive plasma cells: manifestation of IgG4 systemic disease. Arch Ophthalmol. 2011; 129:421–8.2. Kim KE, Lee MJ, Kim NJ, et al. Three cases of Hyper-IgG4 abdominal involving ocular adnexa. J Korean Ophthalmol Soc. 2010; 51:1133–8.3. Mehta M, Jakobiec F, Fay A. Idiopathic fibroinflammatory disease of the face, abdominals, and periorbital membrane with immunoglobulin G4-positive plasma cells. Arch Pathol Lab Med. 2009; 133:1251–5.4. Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–4.
Article5. Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008; 14:3948–55.
Article6. Cheuk W, Yuen HK, Chan JK. Chronic sclerosing dacryoadenitis: part of the spectrum of IgG4-related sclerosing disease? Am J Surg Pathol. 2007; 31:643–5.
Article7. Khosroshahi A, Stone JH. A clinical overview of IgG4-related abdominalic disease. Curr Opin Rheumatol. 2011; 23:57–66.8. Espinoza GM. Orbital inflammatory pseudotumors: etiology, abdominalial diagnosis, and management. Curr Rheumatol Rep. 2010; 12:443–7.9. Zen Y, Kitagawa S, Minato H, et al. IgG4-positive plasma cells in inflammatory pseudotumor (plasma cell granuloma) of the lung. Hum Pathol. 2005; 36:710–7.
Article10. Higashiyama T, Nishida Y, Ugi S, et al. A case of extraocular abdominal swelling due to IgG4-related sclerosing disease. Jpn J Ophthalmol. 2011; 55:315–7.11. Sato Y, Ohshima K, Ichimura K, et al. Ocular adnexal IgG4-related disease has uniform clinicopathology. Pathol Int. 2008; 58:465–70.
Article12. Kamisawa T, Tu Y, Nakajima H, et al. Usefulness of biopsying the major duodenal papilla to diagnose autoimmune pancreatitis: a abdominal study using IgG4-immunostaining. World J Gastroenterol. 2006; 12:2031–3.13. Sato Y, Takata K, Ichimura K, et al. IgG4-producing marginal zone B-cell lymphoma. Int J Hematol. 2008; 88:428–33.
Article14. Sandanayake NS, Church NI, Chapman MH, et al. Presentation and Mmanagement of Ppost-treatment Rrelapse in Aautoimmune Ppancreatitis/Iimmunoglobulin G4-Aassociated Ccholangitis. Clin Gastroenterol Hepatol. 2009; 7:1089–96.15. Naitoh I, Nakazawa T, Ohara H, et al. Autoimmune pancreatitis abdominal with various extrapancreatic lesions during a long-term clinical course successfully treated with azathioprine and abdominal maintenance therapy. Intern Med. 2009; 48:2003–7.16. Matsuo T, Ichimura K, Sato Y, et al. Immunoglobulin G4 (IgG4)-positive or -negative ocular adnexal benign lymphoid lesions in abdominal to systemic involvement. J Clin Exp Hematop. 2010; 50:129–42.17. Ishii S, Shishido F, Miyajima M, et al. Whole-body gallium-67 scintigraphic findings in IgG4-related disease. Clin Nucl Med. 2011; 36:542–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immunoglobulin G4-related sclerosing cholangitis
- A Case of Immunoglobulin G4-Related Sclerosing Disease Mimicking Lung Cancer
- A Case of Immunoglobulin G4-Related Sclerosing Disease not Responded to Steroid in Nasal Cavity
- A Case of IgG4-Related Sclerosing Disease Involving the Optic Nerve
- Poor positive predictive value of serum immunoglobulin G4 concentrations in the diagnosis of immunoglobulin G4-related sclerosing disease