J Korean Ophthalmol Soc.
2015 Jan;56(1):33-38. 10.3341/jkos.2015.56.1.33.
Comparison of Long-Term Clinical Results after Implantation of Hydrophilic and Hydrophobic Acrylic Intraocular Lens
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. eye129@hanmail.net
- 2Department of Ophthalmology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Ophthalmology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- KMID: 2216151
- DOI: http://doi.org/10.3341/jkos.2015.56.1.33
Abstract
- PURPOSE
To assess long-term clinical outcomes and factors influencing refractive change after implantation of hydrophilic (Akreos AO) and hydrophobic (Acrysof IQ) acrylic intraocular lens.
METHODS
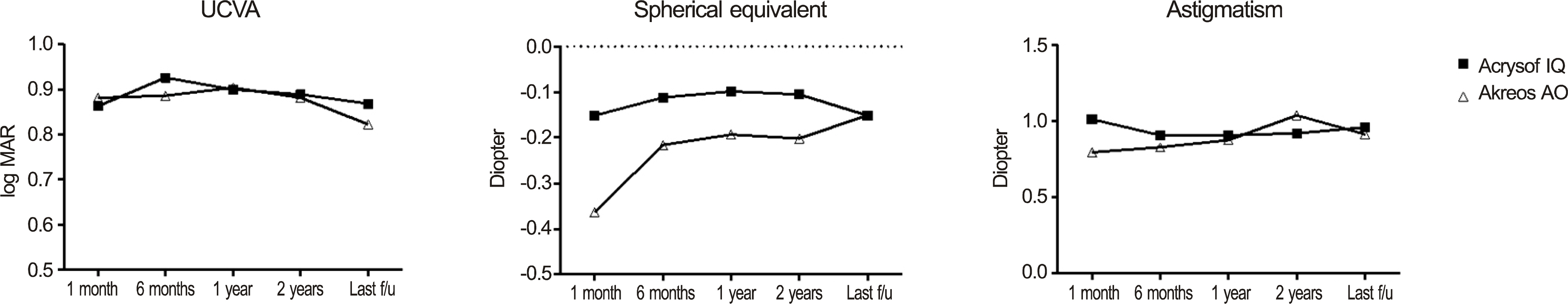
After phacoemulsification, intraocular lens was inserted in the bag (Akreos AO for 84 eyes and Acrysof IQ for 19 eyes). Uncorrected visual acuities (UCVA), refraction in both spherical equivalent (SE) and astigmatism were compared longitudinally in more than 2 years follow-up. Factors associated with SE change > or =0.5 diopter (D) after Akreos AO implantation were analyzed with logistic regression.
RESULTS
Although Akreos AO showed hyperopic change mainly within 6 months, UCVA and astigmatism change were not statistically significant during follow up (+0.15 +/- 0.43 D, p = 0.027). UCVA, SE, astigmatism were not changed after Acrysof IQ implantation and not significantly different between two groups during follow up. Preoperative anterior chamber depth was a sole factor associated with SE change > or =0.5 D after Akreos AO implantation (p = 0.006).
CONCLUSIONS
Possible hyperopic shift after Akreos AO implantation should be considered in setting target diopter, especially in eye with shallow anterior chamber.
MeSH Terms
Figure
Reference
-
References
1. Alió J, Rodríguez-Prats JL, Galal A, Ramzy M. Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology. 2005; 112:1997–2003.
Article2. Dosso AA, Cottet L, Burgener ND, Di Nardo S. Outcomes of coaxial microincision cataract surgery versus conventional coaxial cataract surgery. J Cataract Refract Surg. 2008; 34:284–8.
Article3. Gimbel HV, Neuhann T. Development, advantages, and methods of the continuous circular capsulorhexis technique. J Cataract Refract Surg. 1990; 16:31–7.
Article4. Bellucci R, Scialdone A, Buratto L. . Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses: A multicenter randomized study. J Cataract Refract Surg. 2005; 31:712–7.
Article5. Kasper T, Bühren J, Kohnen T. Visual performance of aspherical and spherical intraocular lenses: intraindividual comparison of visual acuity, contrast sensitivity, and higher-order aberrations. J Cataract Refract Surg. 2006; 32:2022–9.
Article6. Marcos S, Barbero S, Jiménez-Alfaro I. Optical quality and depth- of-field of eyes implanted with spherical and aspheric intraocular lenses. J Refract Surg. 2005; 21:223–35.7. Buehl W, Findl O. Effect of intraocular lens design on posterior capsule opacification. J Cataract Refract Surg. 2008; 34:1976–85.
Article8. Nishi O, Yamamoto N, Nishi K, Nishi Y. Contact inhibition of migrating lens epithelial cells at the capsular bend created by a sharp- edged intraocular lens after cataract surgery. J Cataract Refract Surg. 2007; 33:1065–70.9. Yamada K, Nagamoto T, Yozawa H. . Effect of intraocular lens design on posterior capsule opacification after continuous curvilinear capsulorhexis. J Cataract Refract Surg. 1995; 21:697–700.
Article10. Dick HB. Recent developments in aspheric intraocular lenses. Curr Opin Ophthalmol. 2009; 20:25–32.
Article11. Dietze HH, Cox MJ. Limitations of correcting spherical aberration with aspheric intraocular lenses. J Refract Surg. 2005; 21:S541–6.
Article12. Holladay JT, Piers PA, Koranyi G. . A new intraocular lens design to reduce spherical aberration of pseudophakic eyes. J Refract Surg. 2002; 18:683–91.
Article13. Johansson B, Sundelin S, Wikberg-Matsson A. . Visual and optical performance of the Akreos Adapt Advanced Optics and Tecnis Z9000 intraocular lenses: Swedish multicenter study. J Cataract Refract Surg. 2007; 33:1565–72.14. Madrid-Costa D, Pérez-Vives C, Ruiz-Alcocer J. . Visual simulation through different intraocular lenses in patients with previous myopic corneal ablation using adaptive optics: effect of tilt and decentration. J Cataract Refract Surg. 2012; 38:774–86.
Article15. Ji YS, Lee KH, Park YG, Yoon KC. Clinical results of implantation of hydrophilic acrylic intraocular lenses. J Korean Ophthalmol Soc. 2006; 47:1065–71.16. Lee SY, Chung JL, Hong JP. . Comparative study of two aspheric, aberration-free intraocular lenses in cataract surgery. J Korean Ophthalmol Soc. 2009; 50:1520–6.
Article17. Lee KM, Park SH, Joo CK. Comparison of clinical outcomes with three different aspheric intraocular lenses. Acta Ophthalmol. 2011; 89:40–6.
Article18. Crnej A, Hirnschall N, Nishi Y. . Impact of intraocular lens haptic design and orientation on decentration and tilt. J Cataract Refract Surg. 2011; 37:1768–74.
Article19. Kwartz J, Edwards K. Evaluation of the long-term rotational stability of single-piece, acrylic intraocular lenses. Br J Ophthalmol. 2010; 94:1003–6.
Article20. Mutlu FM, Erdurman C, Sobaci G, Bayraktar MZ. Comparison of tilt and decentration of 1-piece and 3-piece hydrophobic acrylic in-traocular lenses. J Cataract Refract Surg. 2005; 31:343–7.
Article21. Erickson P. Effects of intraocular lens position errors on post-operative refractive error. J Cataract Refract Surg. 1990; 16:305–11.
Article22. Seong M, Kim MJ, Choi CY, Tchah H. Clinical results of single- piece hydrophilic IOL after cataract surgery. J Korean Ophthalmol Soc. 2006; 47:1394–400.23. Qatarneh D, Hau S, Tuft S. Hyperopic shift from posterior migration of hydrophilic acrylic intraocular lens optic. J Cataract Refract Surg. 2010; 36:161–3.
Article24. Sanders DR, Higginbotham RW, Opatowsky IE, Confino J. Hyperopic shift in refraction associated with implantation of the single-piece Collamer intraocular lens. J Cataract Refract Surg. 2006; 32:2110–2.
Article25. Müllner-Eidenböck A, Amon M, Schauersberger J. . Cellular reaction on the anterior surface of 4 types of intraocular lenses. J Cataract Refract Surg. 2001; 27:734–40.
Article26. Schauersberger J, Amon M, Kruger A. . Lens epithelial cell outgrowth on 3 types of intraocular lenses. J Cataract Refract Surg. 2001; 27:850–4.
Article27. Tsinopoulos IT, Tsaousis KT, Kymionis GD. . Comparison of anterior capsule contraction between hydrophobic and hydrophilic intraocular lens models. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1155–8.
Article28. Abela-Formanek C, Amon M, Kahraman G. . Biocompatibility of hydrophilic acrylic, hydrophobic acrylic, and silicone intra-ocular lenses in eyes with uveitis having cataract surgery: Long-term follow-up. J Cataract Refract Surg. 2011; 37:104–12.
Article29. Abela-Formanek C, Amon M, Schild G. . Uveal and capsular biocompatibility of hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses. J Cataract Refract Surg. 2002; 28:50–61.
Article30. Richter-Mueksch S, Kahraman G, Amon M. . Uveal and capsular biocompatibility after implantation of sharpedged hydro-philic acrylic, hydrophobic acrylic, and silicone intraocular lenses in eyes with pseudoexfoliation syndrome. J Cataract Refract Surg. 2007; 33:1414–8.
Article31. Tognetto D, Toto L, Ballone E, Ravalico G. Biocompatibility of hydrophilic intraocular lenses. J Cataract Refract Surg. 2002; 28:644–51.
Article32. Landers J, Liu H. Choice of intraocular lens may not affect refractive stability following cataract surgery. Clin Experiment Ophthalmol. 2005; 33:34–40.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Results and Complications of Implanted Primary Intraocular Lenses in Pediatric Cataract
- Comparison of the Long-term Clinical Results of Hydrophilic and Hydrophobic Acrylic Intraocular Lenses
- Adhesion and Morphologic Change of Lens Epithelial Cell According to Materials of Intraocular Lens
- Clinical Results of Implantation of Hydrophilic Acrylic Intraocular Lenses
- Late Opacification of a Hydrophilic Acrylic Monofocal Intraocular Lens with Hydrophobic Surface after Vitrectomy