J Korean Ophthalmol Soc.
2007 Sep;48(9):1220-1226.
Surgical Results and Complications of Implanted Primary Intraocular Lenses in Pediatric Cataract
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Hospital, Pusan, Korea. wansookim@yahoo.com
Abstract
-
PURPOSE: To evaluate surgical results and complications of different intraocular lenses (IOL) implantation in pediatric cataract surgery.
METHODS
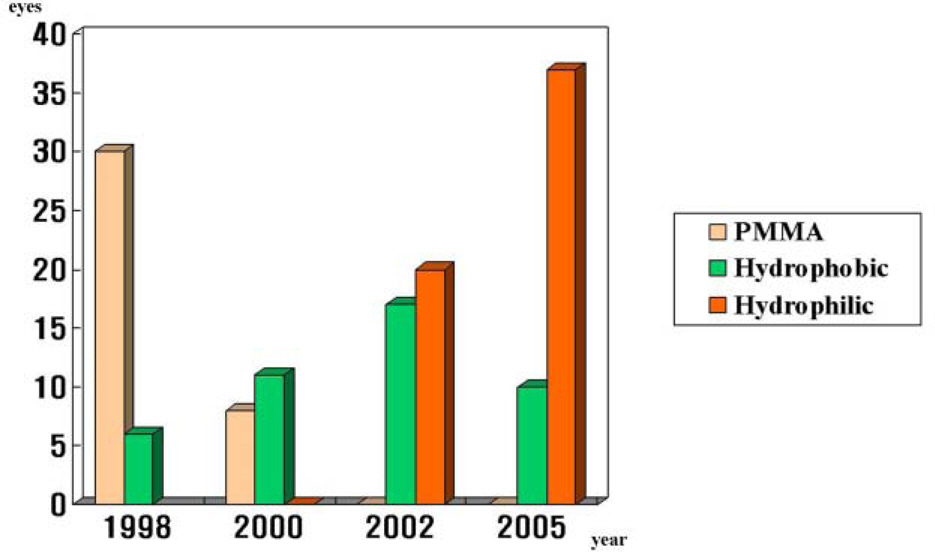
We retrospectively reviewed 139 eyes of 80 patients who had undergone irrigation and aspiration of cataracts and primary posterior chamber intraocular lens implantation with posterior continuous curvilinear capsulorhexis and optic capture from July 1998 to December 2005. All the eyes were divided into three groups into the intraocular lenses implanated: group 1 (n=40), PMMA lens was implantated; group 2 (n=42), hydrophobic acrylic lens was implantated; group 3 (n=57), hydrophilic acrylic lens was implanated. The surgical results and complications was evaluated.
RESULTS
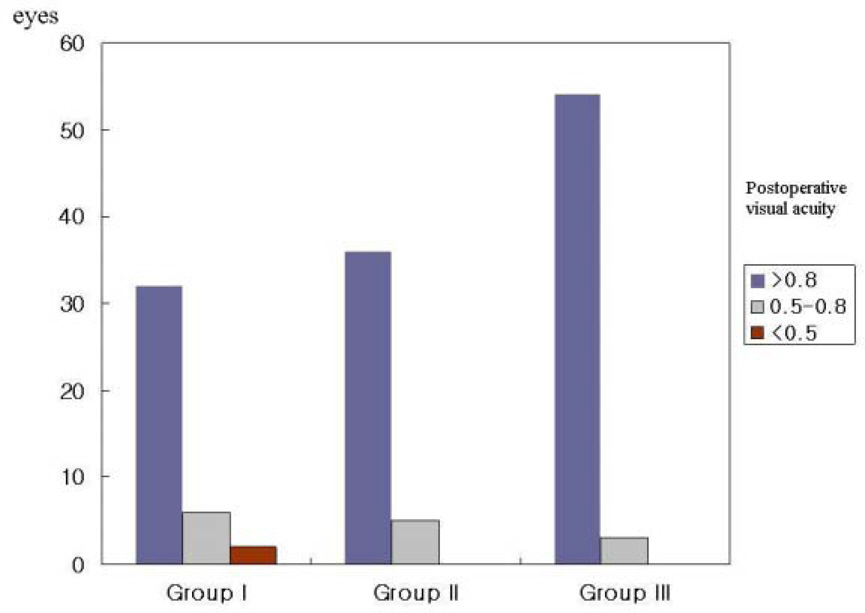
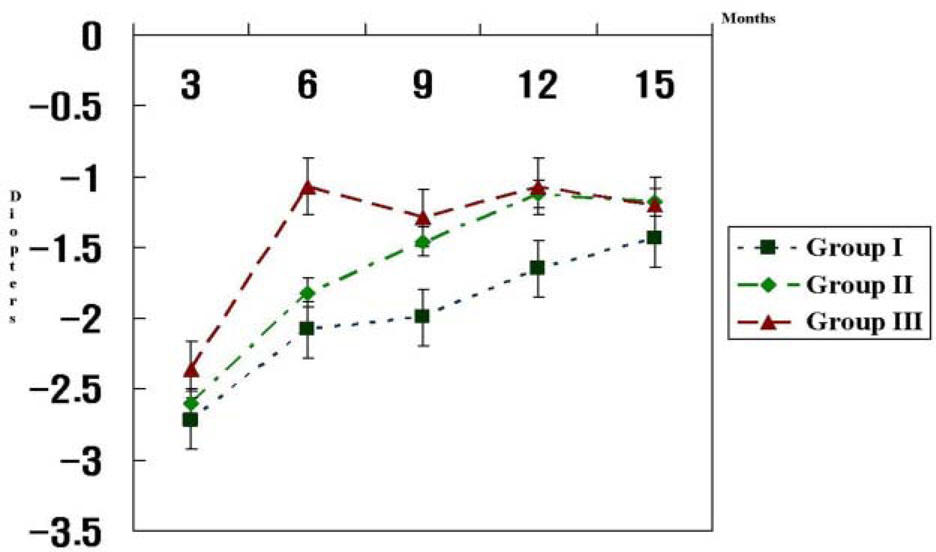
Wound leakage, iris prolapse, shallow anterior chamber during operation were the most common in group 1. Peripheral anterior synechiae, conjuntival cyst, pigment deposition of IOL, exudative membrane, elevated intraocular pressure were also the most common in group 1 (P<0.05). There was no statistically significant defference in the prevalence of intraoperative and postoperative complications between group 2 and 3. Postoperative final visual acuity and astigmatism were not significantly different between the three groups.
CONCLUSIONS
Implantation of hydrophilic acrylic IOLs, as well as hydrophobic acrylic IOLs decrease complications and have good surgical results compared to PMMA IOLs in pediatric cataract surgery.
MeSH Terms
Figure
Reference
-
References
1. Steinert RF. Cataract surgery: Technique, complications, and management. 2nd ed.Philadelphia: WB Saunders;2004. p. 273.2. Kim HY, Yu YS. Effect of posterior chamber intraocular lens implantation on unilateral pediatric cataract. J Korean Ophthalmol Soc. 1997; 38:788–95.3. Sawa M, Sakanishi Y, Shimizu H. Fluorophtometric study of anterior segment barrier functions after extracapsular cataract extraction and posterior chamber intraocular lens implantation. J Cataract Refract Surg. 1996; 22:775–9.4. Kugelberg U, Zetterstorm C, Lundgren B, Syren-Nordqvist S. Ocular growth in newborn rabbit eyes implanted with a poly (methyl methacrylate) or silicone intraocular lens. J Cataract Refract Surg. 1997; 23:629–34.5. Jeon EJ, Kim KB, Yang SW. Cinical results in 1000 cases of Acrysof intraocular lens implantations. J Korean Ophthalmol Soc. 2000; 41:1151–7.6. Dong EY, Joo CK. Four cases of multiple vacuoles inside of Acrysof intraocular lens. J Korean Ophthalmol Soc. 1999; 40:2628–31.7. Argento C, Badoza D, Ugrin C. Optic capture of the Acrysof intraocular lens in pediatric cataract surgery. J Refract Surg. 2001; 27:1638–42.
Article8. Levy JH, Pisacano AM, Chadwick K. Astigmatic changes after cataract surgery with 5.1 mm and 3.5 mm suturless incisions. J Cataract Refract Surg. 1994; 20:630–3.9. Barret GD, Constable IL, Stewart AD. Clinical results of hydrogel lens implantation. J Cataract Refract Surg. 1986; 12:623–31.10. Barret GD, Constable IL. Corneal endothelial loss with new intraocular lenses. Am J Ophthalmol. 1984; 98:157–65.11. Blumenthal M, Chen V. Soft intraocular lenses: evolution and potential. 1st ed.London: Wolfe;1991. p. 122–4.12. Davison JA. Positive and negative dysphotopsia in patients with acrylic intraocular lenses. J Cataract Refract Surg. 1991; 17:32–6.
Article13. Lesegang TJ, Bourne WM, Brubaker RF. The effect of cataract surgery on the blood-aqueous barrier. Streeten BW. Pathology of lens. In : Albert DM, Jakobiec FA, editors. Principles and practice of Ophthalmology. 2nd ed.Philadelphia: WB Saunders;2000. v. 4. chap. 272.14. Carlson KH, Cameron JD, Lindstrom RL. Assessment of blood-aqueous barrier by fluorophotometry following PMMA, silicone and hydrogel lens implanatation in rabbit eyes. J Cataract Refract Surg. 1993; 19:9–15.15. Werner L, Apple DJ, Escobar-Gomez M, et al. Postoperative deposition of calcium on the surface of a hydrogel intraocular lens. Ophthalmology. 2000; 107:2179–85.16. Mamalis N. Complications of foldable intraocular lenses requiring explantation or secondary intervention -2001 survey update. J Cataract Refract Surg. 2002; 28:2193–201.17. Trivedi RH, Werner L, Apple DJ, et al. Post cataract- intraocular lens (IOL) surgery opacification. Eye. 2002; 16:217–41.18. Dorey MW, Brownstein S, Hill VE, et al. Proposed pathogenesis for the delayed postoperative opacification of the Hydroview hydrogel intraocular lens. Am J Ophthalmol. 2003; 135:591–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Nd:YAG Capsulotomy Rates between Spherical and Aspheric Intraocular Lenses
- Aniridia Intraocular Lens
- Implantation of Posterior Chamber Lens in the Absenee of Posterior Capsular Support
- Implantation of Intraocular Lenses in Traumatic Cataract
- Clinical Evaluation of Combined Surgery in Coexisting Glaucoma and Cataract (II)