J Korean Ophthalmol Soc.
2012 Jan;53(1):168-174. 10.3341/jkos.2012.53.1.168.
Two Cases of Young Patients with Bilateral Posterior Scleritis Accompanied with Serous Retinal Detachment
- Affiliations
-
- 1Department of Ophthalmology, Konyang University Hospital, Daejeon, Korea. idoc@kimeye.com
- KMID: 2215261
- DOI: http://doi.org/10.3341/jkos.2012.53.1.168
Abstract
- PURPOSE
To report 2 young female patients with bilateral posterior scleritis and serous retinal detachment.
CASE SUMMARY
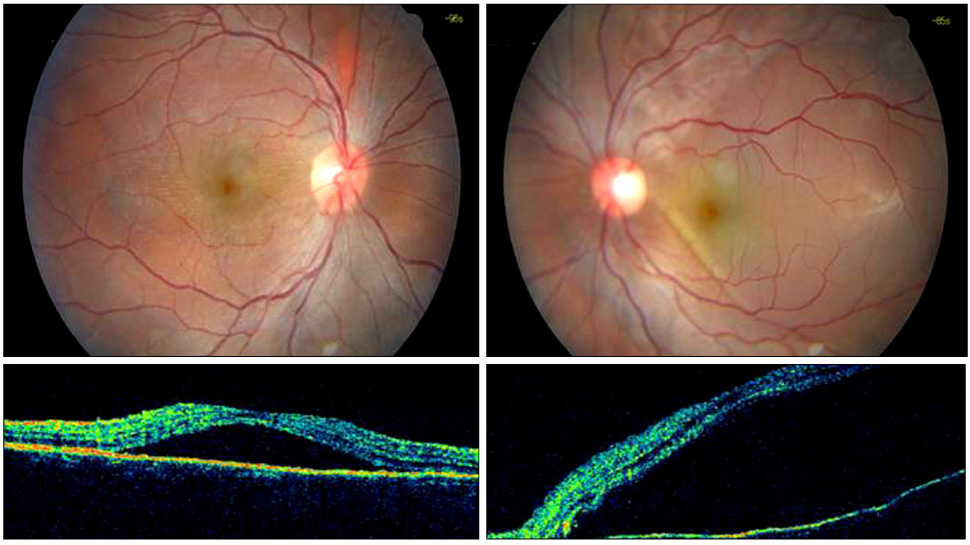
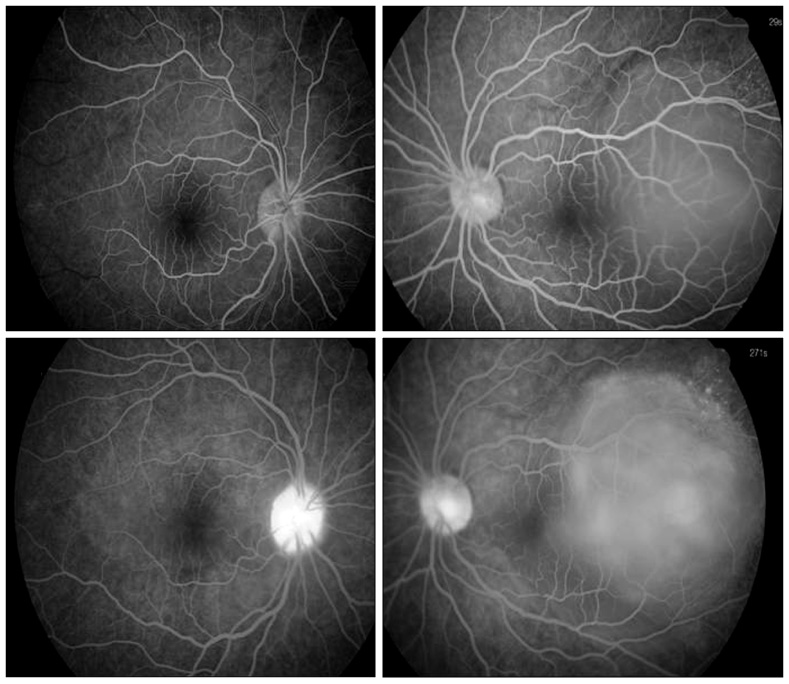
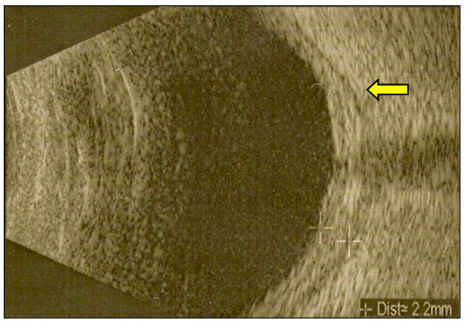
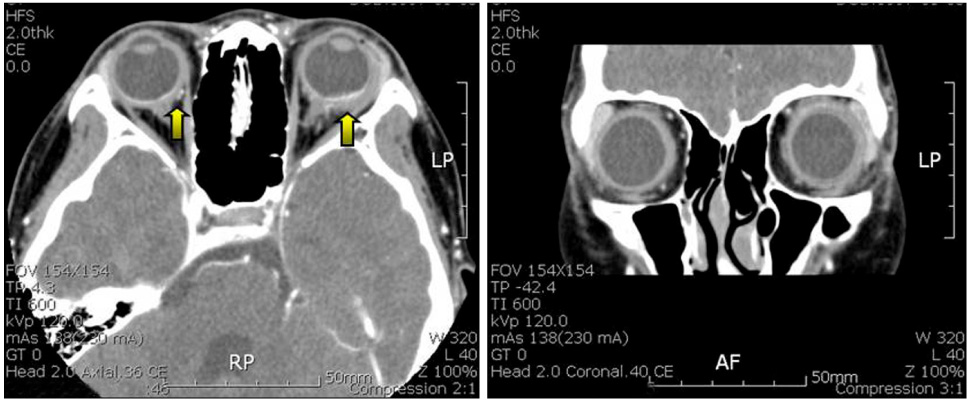
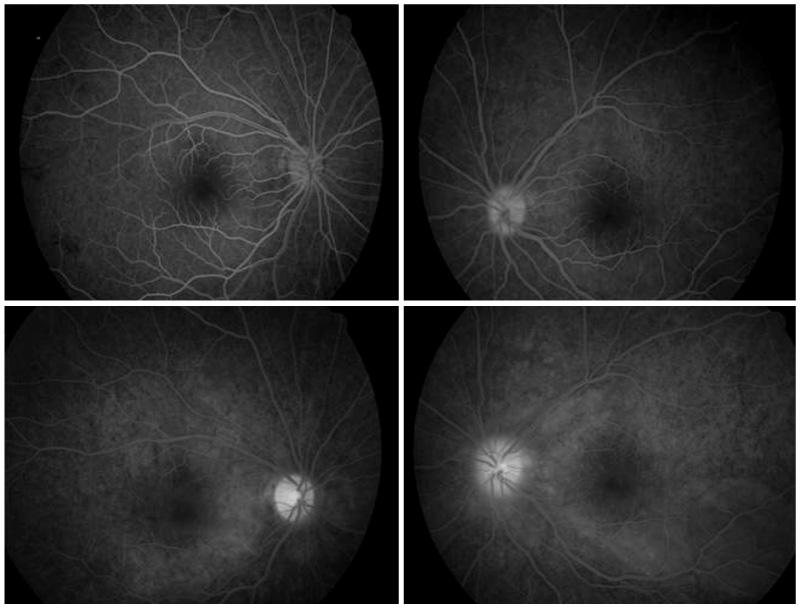
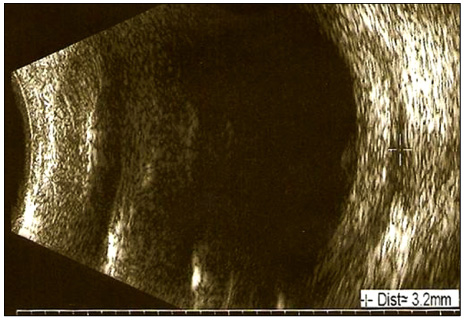
An 11-year-old girl (Case 1) and a 16-year-old girl (Case 2) visited our clinic with bilateral ocular pain, redness, and blurred vision. Slit lamp examinations revealed severe bilateral scleral injection and mild anterior chamber reactions. Fundus examinations showed bilateral serous retinal detachments in the macular area. In both patients, diffuse multifocal leaking and pooling were found at the macula in the early and late phase fluorescein angiography, respectively. On the B-mode ultrasounds and orbital images (MRI or CT), scleral thickening with retention of subtenons fluid were found. There were no systemic diseases associated with the conditions. We diagnosed the patients with bilateral posterior scleritis and administered systemic steroids. After systemic steroid treatment, all of the symptoms were alleviated. Three months after the regression, bilateral posterior scleritis recurred in patient 2. Oral cyclosporine 100 mg was additionally prescribed in addition to the previous medications that she had taken during her first treatment.
CONCLUSIONS
Two young patients diagnosed with posterior scleritis and serous retinal detachment was treated with systemic steroids. With proper examination and treatment, posterior scleritis can be treated with no complications.
MeSH Terms
Figure
Reference
-
1. McCluskey PJ, Watson PG, Lightman S, et al. Posterior scleritis: clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999. 106:2380–2386.2. Benson WE. Posterior scleritis. Surv Ophthalmol. 1988. 32:297–316.3. Wald KJ, Spaide R, Patalano VJ, et al. Posterior scleritis in children. Am J Ophthalmol. 1992. 113:281–286.4. Tsujikawa A, Yamashiro K, Yamamoto K, et al. Retinal cystoid spaces in acute Vogt-Koyanagi-Harada syndrome. Am J Ophthalmol. 2005. 139:670–677.5. Erdol H, Kola M, Turk A. Optical coherence tomography findings in a child with posterior scleritis. Eur J Ophthalmol. 2008. 18:1007–1010.6. Jensen JE, Fledelius HC, Prause JU, Scherfig E. An unusual ophthalmic tumour in a 5-year-old boy. Acta Ophthalmol Suppl. 1992. 204:110–102.7. Foster CS, de la Maza M Sa. The sclera. 1994. New York: Springer-Verlag;112–123.8. Woon WH, Stanford MR, Graham EM. Severe idiopathic posterior scleritis in children. Eye. 1995. 9:570–574.9. Watson PG, Young RD. Scleral structure, organisation and disease. A review. Exp Eye Res. 2004. 78:609–623.10. McCluskey P, Wakefield D. Intravenous pulse methylprednisolone in scleritis. Arch Ophthalmol. 1987. 105:793–797.11. Wakefield D, McCluskey P. Cyclosporin therapy for severe scleritis. Br J Ophthalmol. 1989. 73:743–746.12. Horo S, Sudharshan S, Biswas J. Recurrent posterior scleritis-report of a case. Ocul Immunol Inflamm. 2006. 14:51–56.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retinal Pigment Epithelial Detachment in Posterior Scleritis
- Serous Retinal Detachment Following Laser Peripheral Iridotomy for the Angle Closure Secondary to Posterior Scleritis
- A Case of Post. Scleritis Associated with Ciliochoroidal Detachment and Ant. Uveitis in Background Diabetic Retinopathy Patient
- Infectious Scleritis Featuring Kissing Choroidal Detachment and Serous Retinal Detachment
- Bilateral Serous Retinal Detachment Associated With Alport's Syndrome