J Korean Ophthalmol Soc.
2012 Jan;53(1):11-19. 10.3341/jkos.2012.53.1.11.
LASIK for Myopia with Presbyopia Using the Aspheric Micro-Monovision Technique
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. eschung@skku.edu
- 2Nune Eye Hospital, Seoul, Korea.
- KMID: 2215240
- DOI: http://doi.org/10.3341/jkos.2012.53.1.11
Abstract
- PURPOSE
To evaluate the efficacy, safety, and satisfaction of patients who underwent the aspheric micro-monovision protocol for the correction of myopia with presbyopia.
METHODS
A retrospective, noncomparative study included 40 eyes of 20 consecutive patients with myopia and presbyopia who were treated with LASIK-induced micro-monovision. Monocular and binocular visual outcomes of uncorrected and best-corrected distance, intermediate, and near visual acuity were measured. Depth of focus, spherical aberration, stereopsis and satisfaction were evaluated before surgery and 3 months after surgery.
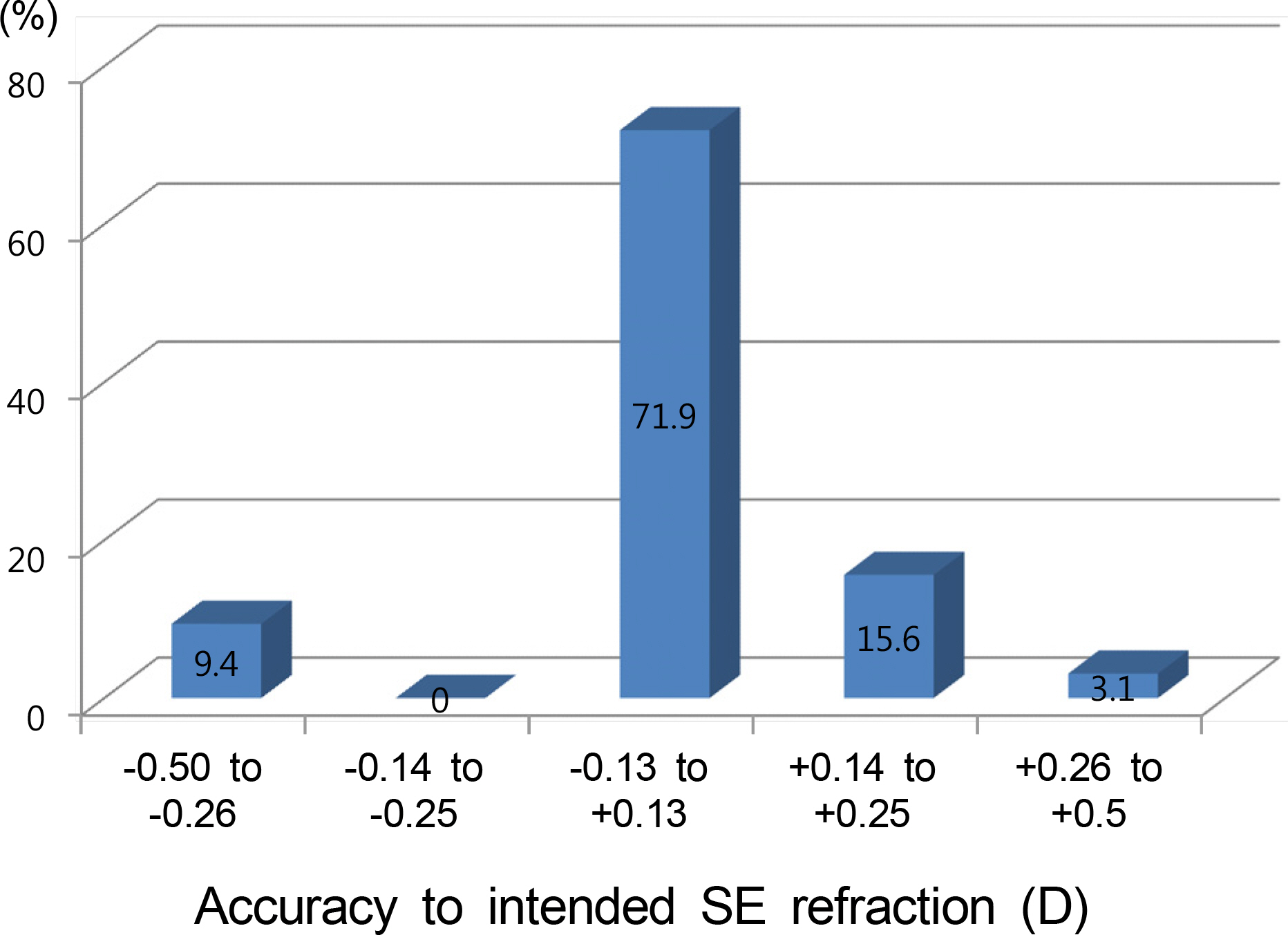
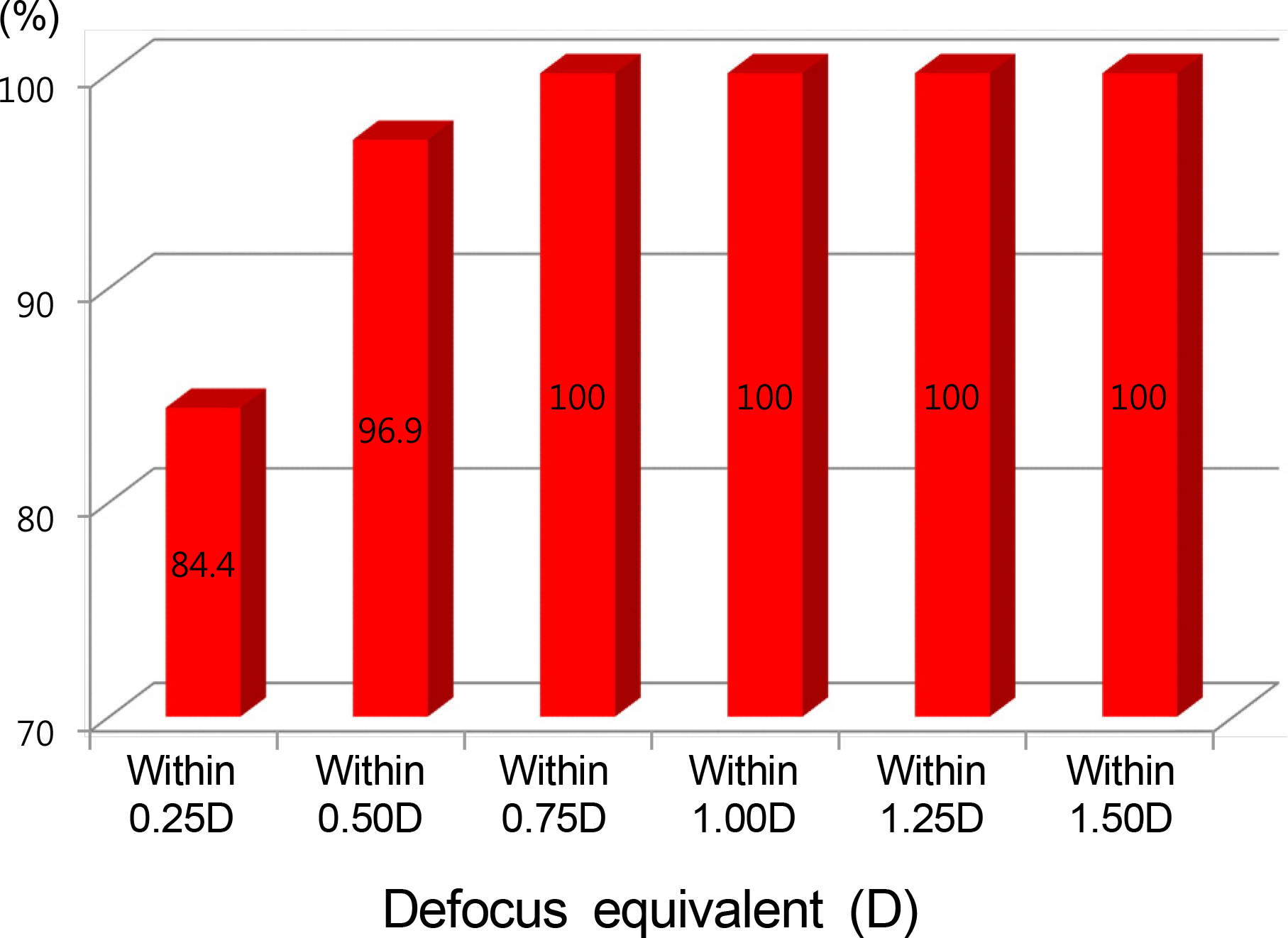
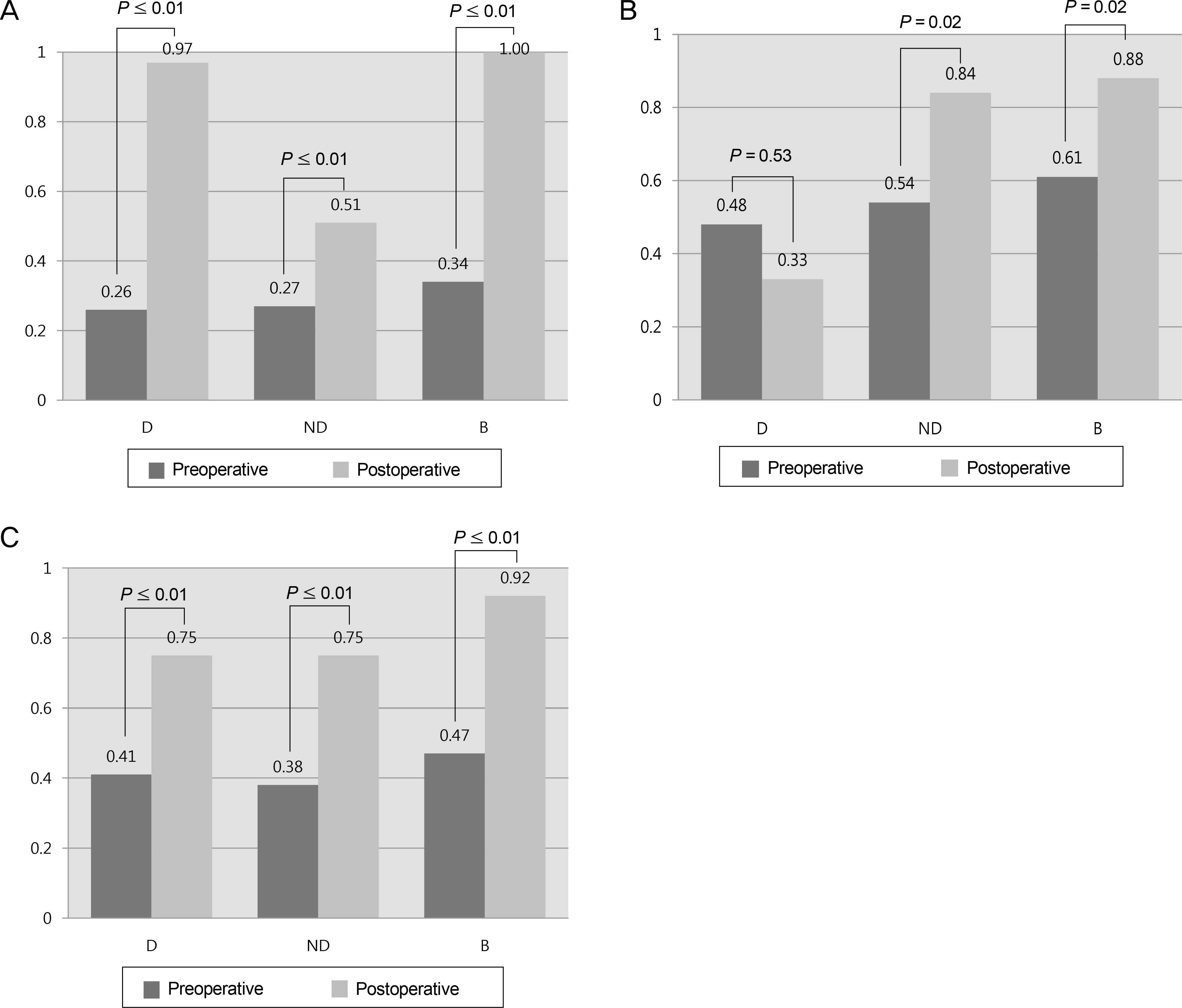
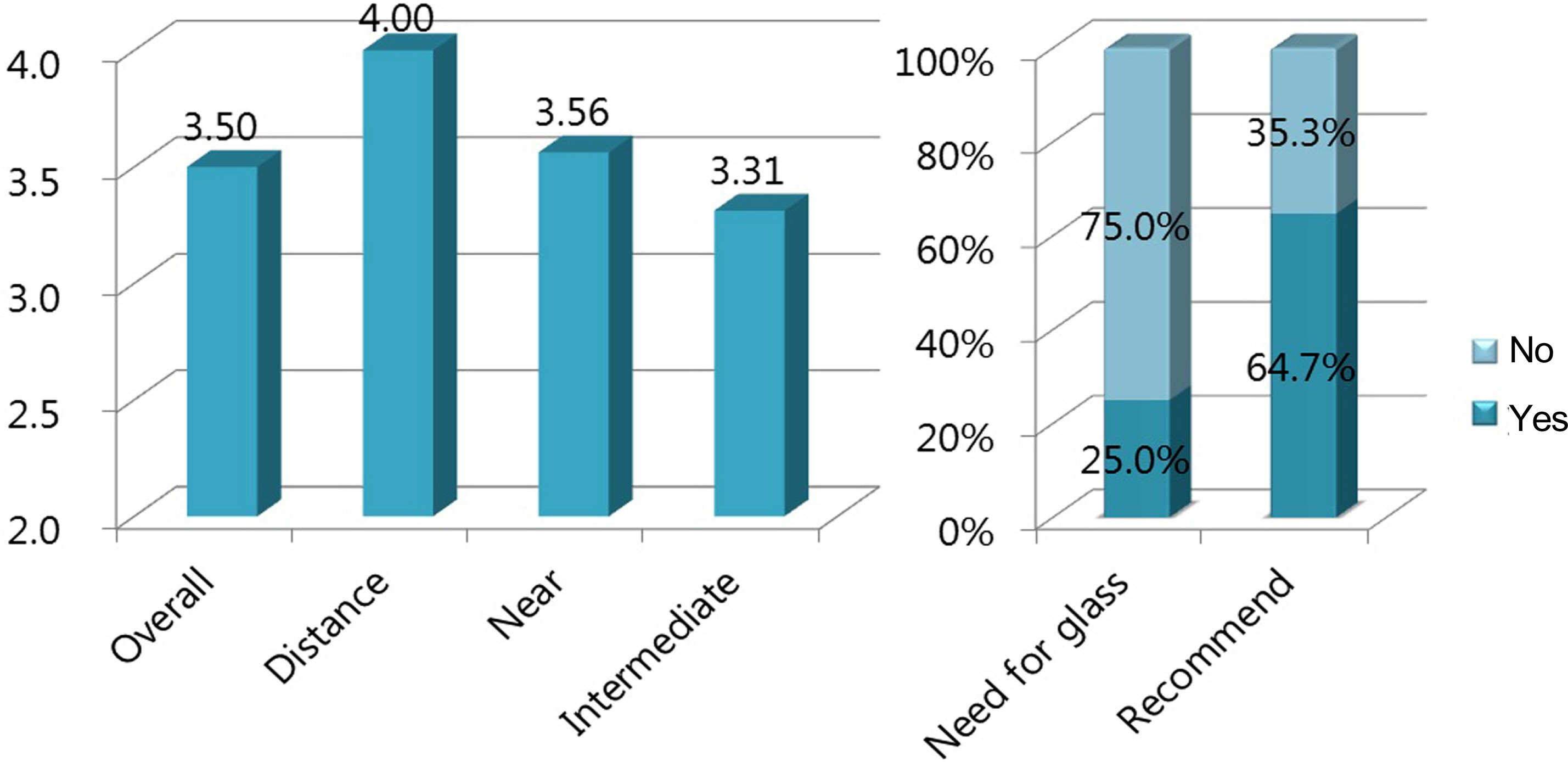
RESULTS
Mean patient age was 48.7 years. Monocular uncorrected distance visual acuity was 0.8 in 94% of dominant eyes, and monocular uncorrected near visual acuity was J3 in 94% in non-dominant eyes. Binocular uncorrected near visual acuity was J2 in 94% and J5 in 100% of dominant and non-dominant patient eyes, respectively. Binocular uncorrected distance visual acuity was 1.0 in 100% of patients, and binocular uncorrected near visual acuity was J2 in 94% of patients. Our results showed a significant improvement in depth of focus and a positive shift in spherical aberration in dominant eyes; however, there were no significant changes in the non-dominant eyes. There was no change in stereopsis or contrast sensitivity at any of the tested spatial frequencies. Satisfactory scores were achieved in all eyes.
CONCLUSIONS
The aspheric myopic micro-monovision protocol was well-tolerated, stable, and effective for treating patients with presbyopia in myopic astigmatism.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Clinical Outcomes between Laser Blended Vision and Monovision Laser Refractive Surgery for Presbyopia
Suchan Lee, Cheolwon Jang, Seok Joon Kong, Jae Woo Kim, Young Joo Cho, Tae Hyung Lim, Kee Yong Choi, Beom Jin Cho
J Korean Ophthalmol Soc. 2016;57(12):1840-1848. doi: 10.3341/jkos.2016.57.12.1840.
Reference
-
References
1. Heatley CJ, Spalton DJ, Boyce JF, Marshall J. A mathematical model of factors that influence the performance of accommodative intraocular lenses. Ophthalmic Physiol Opt. 2004; 24:111–8.
Article2. Hersh PS. Optics of conductive keratoplasty: implications for presbyopia management. Trans Am Ophthalmol Soc. 2005; 103:412–56.
Article3. Haw WW, Manche EE. Conductive keratoplasty and laser thermal keratoplasty. Int Ophthalmol Clin. 2002; 42:99–106.
Article4. Wright KW, Guemes A, Kapadia MS, Wilson SE. Binocular function and patient satisfaction after monovision induced by myopic photorefractive keratectomy. J Cataract Refract Surg. 1999; 25:177–82.5. Vinciguerra P, Nizzola GM, Nizzola F, et al. Zonal photorefractive keratectomy for presbyopia. J Refract Surg. 1998; 14:S218–21.
Article6. Bauerberg JM. Centered vs. inferior off-center ablation to correct hyperopia and presbyopia. J Refract Surg. 1999; 15:66–9.7. Williams DK. One-year results of laser vision correction for low to moderate hyperopia. Ophthalmology. 2000; 107:72–5.
Article8. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001; 27:1449–55.
Article9. Miranda D, Krueger RR. Monovision laser in situ keratomileusis for pre-presbyopic and presbyopic patients. J Refract Surg. 2004; 20:325–8.
Article10. Alió JL, Chaubard JJ, Caliz A, et al. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK). J Refract Surg. 2006; 22:453–60.
Article11. Reinstein DZ, Couch DG, Archer TJ. LASIK for hyperopic astigmatism and presbyopia using micro-monovision with the Carl Zeiss Meditec MEL80 platform. J Refract Surg. 2009; 25:37–58.
Article12. Reinstein DZ, Archer TJ, Gobbe M. LASIK for Myopic Astigmatism and Presbyopia Using Non-Linear Aspheric Micro-Monovision with the Carl Zeiss Meditec MEL 80 Platform. J Refract Surg. 2011; 27:23–37.
Article13. Fukuyama M, Oshika T, Amano S, Yoshitomi F. Relationship between apparent accomodation and corneal multifocality in pseudophakic eyes. Ophthalmology. 1999; 106:1178–81.14. Oshika T, Mimura T, Tanaka S, et al. Apparent accommodation and corneal wavefront aberration in pseudophakic eyes. Invest Ophthalmol Vis Sci. 2002; 43:2882–6.15. Michaels DD. Visual Optics and Refraction: A Clinical Approach. 1st ed.St Louis: Mosby;1975. p. 273–4.16. Kurtz D. Presbyopia. Brookman KE, editor. Refractive Management of Ametropia. Boston: Butterworth-Heinemann;1996. p. 145–79.17. Adler F. Physiology of the Eye: Clinical Application. 8th ed.St Louis: Mosby;1987. p. 200–1.18. Goldberg DB. Comparison of myopes and hyperopes after laser in situ keratomileusis monovision. J Cataract Refract Surg. 2003; 29:1695–701.
Article19. Yasuda A, Yamaguchi T. Steepening of corneal curvature with contraction of the ciliary muscle. J Cataract Refract Surg. 2005; 31:1177–81.
Article20. Glasser A, Troilo D, Howland HC. The mechanism of corneal accommodation in chicks. Vision Res. 1994; 34:1549–66.
Article21. Artola A, Patel S, Schimchak P, et al. Evidence for delayed presbyopic after photorefractive keratectomy for myopia. Ophthalmology. 2006; 113:735–41.e1.22. Marcos S, Moreno E, Navarro R. The depth-of-field of the human eye from objective and subjective measurements. Vision Res. 1999; 39:2039–49.
Article23. Nio YK, Jansonius NM, Wijdh RH, et al. Effect of methods of myopia correction on visual acuity, contrast sensitivity, and depth of focus. J Cataract Refract Surg. 2003; 29:2082–95.
Article24. Ninomiya S, Fujikado T, Kuroda T, et al. Changes of ocular aberration with accommodation. Am J Ophthalmol. 2002; 134:924–6.
Article25. Chun YS, Lee HI, Dausch D, Kim JC. Long-term results of presbyopic corneal surface ablation with eximer laser. J Korean Ophthalmol Soc. 2008; 49:1061–70.
Article26. Jain S, Ou R, Azar DT. Monovision outcomes in presbyopic in-dividuals after refractive surgery. Ophthalmology. 2001; 108:1430–3.27. Ang RE, Chan WK, Wee TL, et al. Efficacy of an aspheric treatment algorithm in decreasing induced spherical aberration after laser in situ keratomileusis. J Cataract Refract Surg. 2009; 35:1348–57.
Article28. Holladay JT, Van Dijk H, Lang A, et al. Optical performance of multifocal intraocular lenses. J Cataract Refract Surg. 1990; 16:413–22.
Article29. Oshika T, Klyce SD, Applegate RA, et al. Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol. 1999; 127:1–7.
Article30. Marcos S, Barbero S, Llorente L, Merayo-Lloves J. Optical response to LASIK surgery for myopia from total and corneal aberration measurements. Invest Ophthalmol Vis Sci. 2001; 42:3349–56.31. Duane A. Normal values of the accommodation at all ages. JAMA. 1912; 52:1010–3.
Article32. Heatley CJ, Spalton DJ, Hancox J, et al. Fellow eye comparison between the 1CU accommodative intraocular lens and the Acrysof MA30 monofocal intraocular lens. Am J Ophthalmol. 2005; 140:207–13.
Article33. Hancox J, Spalton D, Heatley C, et al. Objective measurement of intraocular lens movement and dioptric change with a focus shift accommodating intraocular lens. J Cataract Refract Surg. 2006; 32:1098–103.
Article34. Chiam PJ, Chan JH, Haider SI, et al. Functional vision with bi-lateral ReZoom and ReSTOR intraocular lenses 6 months after cataract surgery. J Cataract Refract Surg. 2007; 33:2057–61.
Article35. Schmidinger G, Simader C, Dejaco-Ruhswurm I, et al. Contrast sensitivity function in eyes with diffractive bifocal intraocular lenses. J Cataract Refract Surg. 2005; 31:2076–83.
Article36. Kohnen T, Allen D, Boureau C, et al. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology. 2006; 113:584.e1.
Article37. Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007; 33:1244–7.
Article38. Wachler BS, Krueger RR. Normalized contrast sensitivity values. J Refract Surg. 1998; 14:463–6.
Article39. Reinstein DZ, Archer TJ, Couch D, et al. A new night vision disturbances parameter and contrast sensitivity as indicators of success in wavefront-guided enhancement. J Refract Surg. 2005; 21:S535–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Results of LASIK for Presbyopia Correction in Myopic Patients Using Aspheric Micro-Monovision
- Surgical treatment of presbyopia I
- Surgical treatment of presbyopia
- Comparison of Clinical Outcomes between Laser Blended Vision and Monovision Laser Refractive Surgery for Presbyopia
- Clinical Evaluation of Monovision After Cataract Surgery