J Korean Med Assoc.
2019 Dec;62(12):616-622. 10.5124/jkma.2019.62.12.616.
Surgical treatment of presbyopia I
- Affiliations
-
- 1Saevit Eye Hospital, Goyang, Korea. joohyun@saeviteye.com
- KMID: 2465355
- DOI: http://doi.org/10.5124/jkma.2019.62.12.616
Abstract
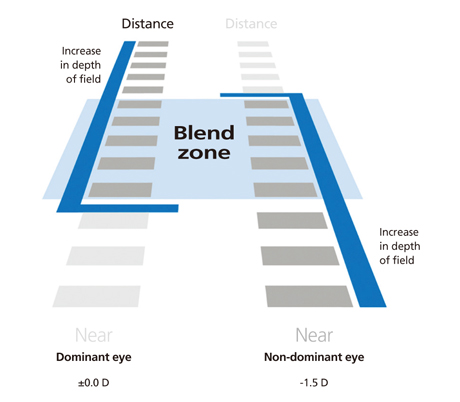
- Presbyopia is an age-related condition that progressively decreases the ability to focus on near objects. Minimally invasive surgical techniques have been developed to improve near vision, including laser in situ keratomileuses (LASIK) and corneal inlay. Most have similar approaches using monovision or increasing the depth of focus. Monovision laser refractive surgery is a combination of conventional LASIK, LASIK which creates a multifocal cornea (central near or peripheral near) and aspheric micro-monovision LASIK with a special ablation profile, which develops spherical aberration. Conductive keratoplasty is a method that uses radiofrequency energy to shrink the mid-peripheral corneal stromal tissue. However, it is not used because of regression. A corneal inlay is a small device that is implanted in the corneal flap or pocket made by a femtosecond laser. It is inserted into the non-dominant eye. There are various inlays such as the Flexivue Microlens (refractive), Raindrop (corneal shape-changing), and KAMRA (small-aperture) inlays. However, the safety and effectiveness of these inlays have not been proven over a long follow-up period, so care is required when performing inlay implantation. All presbyopia treatments can improve near vision but also have limitations and side effects such as reduced far vision, contrast sensitivity, or increased glare. Therefore, it is essential to select patients carefully. Mechanisms associated with presbyopia are not fully understood, and presbyopia remains challenging for ophthalmologists.
MeSH Terms
Figure
Reference
-
1. Duane A. A modified accommodation line and Prince's rule. Trans Am Ophthalmol Soc. 1921; 19:178–179.2. Lebow KA, Goldberg JB. Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses. J Am Optom Assoc. 1975; 46:1116–1123.3. Kohnen T, Allen D, Boureau C, Dublineau P, Hartmann C, Mehdorn E, Rozot P, Tassinari G. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology. 2006; 113:584.e1.
Article4. Malandrini A, Martone G, Menabuoni L, Catanese AM, Tosi GM, Balestrazzi A, Corsani C, Fantozzi M. Bifocal refrac-tive corneal inlay implantation to improve near vision in emmetropic presbyopic patients. J Cataract Refract Surg. 2015; 41:1962–1972.
Article5. Heatley CJ, Spalton DJ, Boyce JF, Marshall J. A mathematical model of factors that influence the performance of accom-modative intraocular lenses. Ophthalmic Physiol Opt. 2004; 24:111–118.
Article6. Schor C, Landsman L, Erickson P. Ocular dominance and the interocular suppression of blur in monovision. Am J Optom Physiol Opt. 1987; 64:723–730.
Article7. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001; 27:1449–1455.
Article8. Miranda D, Krueger RR. Monovision laser in situ kerato-mileusis for pre-presbyopic and presbyopic patients. J Refract Surg. 2004; 20:325–328.
Article9. Reinstein DZ, Archer TJ, Gobbe M. LASIK for myopic astigmatism and presbyopia using non-linear aspheric micro-monovision with the Carl Zeiss Meditec MEL 80 platform. J Refract Surg. 2011; 27:23–37.
Article10. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012; 28:531–541.
Article11. Pallikaris IG, Panagopoulou SI. PresbyLASIK approach for the correction of presbyopia. Curr Opin Ophthalmol. 2015; 26:265–272.
Article12. Menassa N, Fitting A, Auffarth GU, Holzer MP. Visual outcomes and corneal changes after intrastromal femtosecond laser correction of presbyopia. J Cataract Refract Surg. 2012; 38:765–773.
Article13. Holzer MP, Knorz MC, Tomalla M, Neuhann TM, Auffarth GU. Intrastromal femtosecond laser presbyopia correction: 1-year results of a multicenter study. J Refract Surg. 2012; 28:182–188.
Article14. Ayoubi MG, Leccisotti A, Goodall EA, McGilligan VE, Moore TC. Femtosecond laser in situ keratomileusis versus conductive keratoplasty to obtain monovision in patients with emmetropic presbyopia. J Cataract Refract Surg. 2010; 36:997–1002.
Article15. Park JH, Kim MJ. Surgical treatment of presbyopia. J Korean Med Assoc. 2014; 57:520–524.
Article16. Steinert RF, Storie B, Smith P, McDonald MB, van Rij G, Bores LD, Colin JP, Durrie DS, Kelley C, Price F Jr, Rostron C, Waring GO 3rd, Nordan LT. Hydrogel intracorneal lenses in aphakic eyes. Arch Ophthalmol. 1996; 114:135–141.
Article17. Barraquer JI. Modification of refraction by means of intracor-neal inclusions. Int Ophthalmol Clin. 1966; 6:53–78.
Article18. Gil-Cazorla R, Shah S, Naroo SA. A review of the surgical options for the correction of presbyopia. Br J Ophthalmol. 2016; 100:62–70.
Article19. Beer SMC, Santos R, Nakano EM, Hirai F, Nitschke EJ, Francesconi C, Campos M. One-year clinical outcomes of a corneal inlay for presbyopia. Cornea. 2017; 36:816–820.
Article20. Beer SMC, Werner L, Nakano EM, Santos RT, Hirai F, Nitschke EJ, Francesconi Benicio C, Campos MSQ. A 3-year follow-up study of a new corneal inlay: clinical results and outcomes. Br J Ophthalmol. 2019; 08. 24. DOI: 10.1136/bjophthalmol-2019-314314. [Epub].
Article21. Whitman J, Hovanesian J, Steinert RF, Koch D, Potvin R. Through-focus performance with a corneal shape-changing inlay: One-year results. J Cataract Refract Surg. 2016; 42:965–971.
Article22. Dexl AK, Jell G, Strohmaier C, Seyeddain O, Riha W, Ruckl T, Bachernegg A, Grabner G. Long-term outcomes after mono-cular corneal inlay implantation for the surgical compensation of presbyopia. J Cataract Refract Surg. 2015; 41:566–575.
Article23. Larrea X, De Courten C, Feingold V, Burger J, Buchler P. Oxygen and glucose distribution after intracorneal lens implantation. Optom Vis Sci. 2007; 84:1074–1081.
Article24. Lang AJ, Holliday K, Chayet A, Barragan-Garza E, Kathuria N. Structural changes induced by a corneal shape-changing inlay, deduced from optical coherence tomography and wave-front measurements. Invest Ophthalmol Vis Sci. 2016; 57:OCT154–OCT161.
Article25. Garza EB, Gomez S, Chayet A, Dishler J. One-year safety and efficacy results of a hydrogel inlay to improve near vision in patients with emmetropic presbyopia. J Refract Surg. 2013; 29:166–172.
Article26. Garza EB, Chayet A. Safety and efficacy of a hydrogel inlay with laser in situ keratomileusis to improve vision in myopic presbyopic patients: one-year results. J Cataract Refract Surg. 2015; 41:306–312.
Article27. Moshirfar M, Desautels JD, Wallace RT, Koen N, Hoopes PC. Comparison of FDA safety and efficacy data for KAMRA and Raindrop corneal inlays. Int J Ophthalmol. 2017; 10:1446–1451.
Article28. Moshirfar M, Buckner B, Rosen DB, Heiland MB, Ronquillo YC, Skanchy DF, Liu HY, Melton T, Werner L, Hoopes PC. Visual prognosis after explantation of a corneal shape-chang-ing hydrogel inlay in presbyopic eyes. Med Hypothesis Discov Innov Ophthalmol. 2019; 8:139–144.29. Seyeddain O, Hohensinn M, Riha W, Nix G, Ruckl T, Grabner G, Dexl AK. Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up. J Cataract Refract Surg. 2012; 38:35–45.
Article30. Dexl AK, Seyeddain O, Riha W, Ruckl T, Bachernegg A, Emesz M, Ruckhofer J, Grabner G. Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up. J Cataract Refract Surg. 2012; 38:1808–1816.
Article