J Korean Ophthalmol Soc.
2011 Dec;52(12):1399-1404. 10.3341/jkos.2011.52.12.1399.
Long-Term Results after Three or More Penetrating Keratoplasties and Risk Factors for Graft Failure
- Affiliations
-
- 1Department of Ophthalmology, Chonnam National University Medical School, Gwangju, Korea. kcyoon@chonnam.ac.kr
- 2Department of Ophthalmology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2215141
- DOI: http://doi.org/10.3341/jkos.2011.52.12.1399
Abstract
- PURPOSE
To evaluate the primary indications, surgical outcomes, causes and risk factors for graft failure in patients with three or more penetrating keratoplasty (PKP) surgeries.
METHODS
We retrospectively analyzed indications for the initial corneal graft, survival periods, causes and risk factors for failure in 25 patients (26 eyes) who had undergone three or more PKP with minimum follow-up periods of nine months.
RESULTS
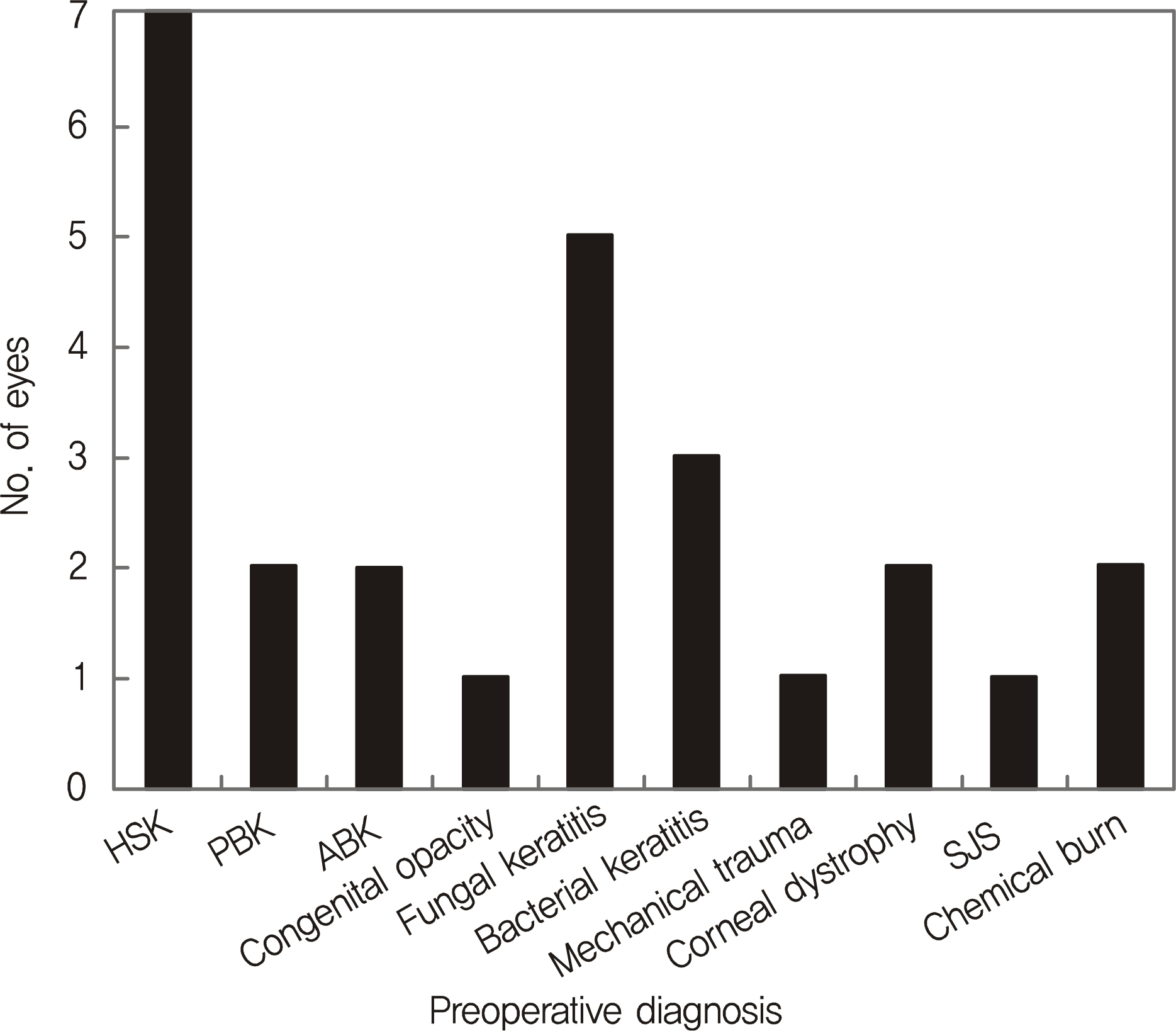
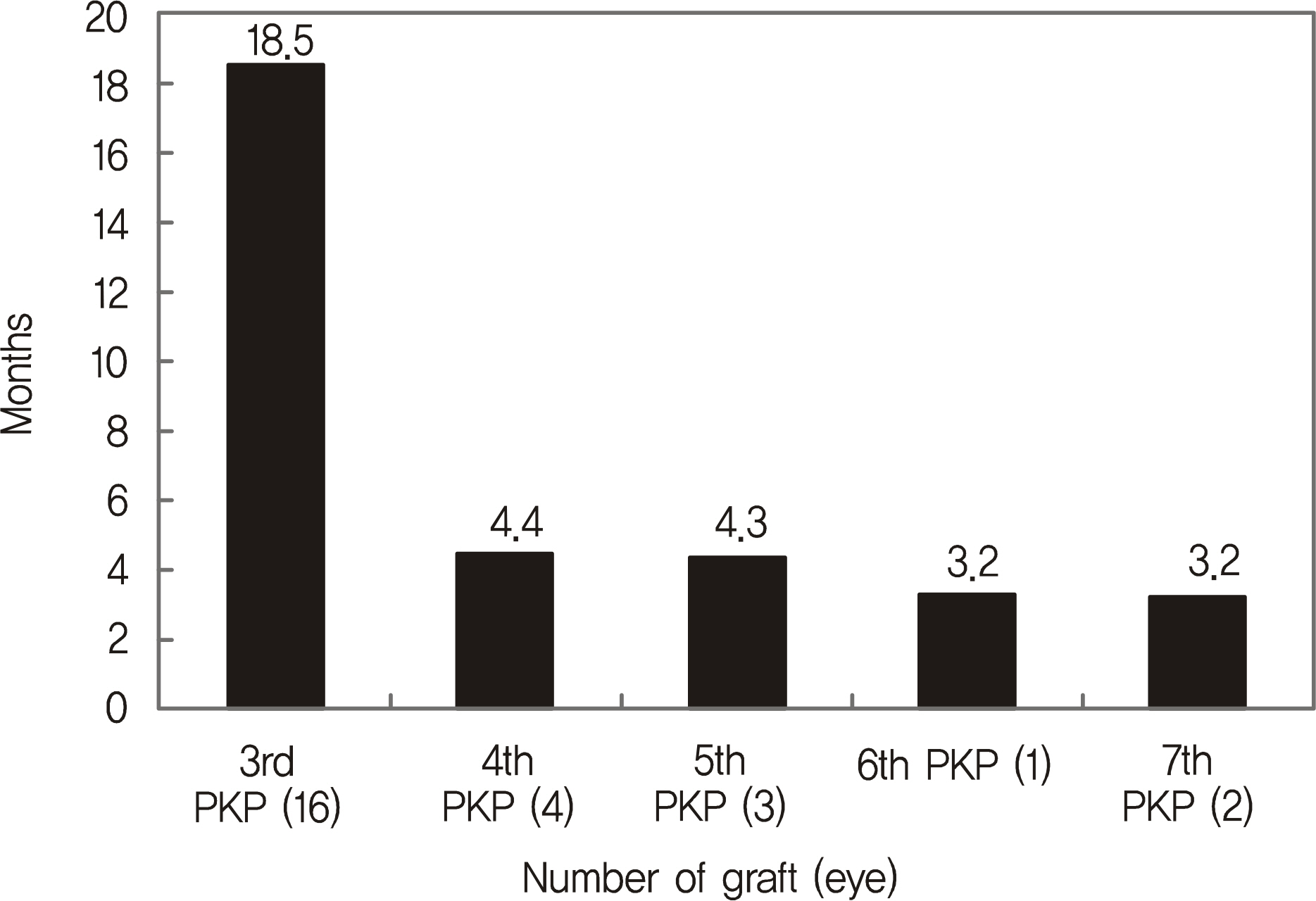
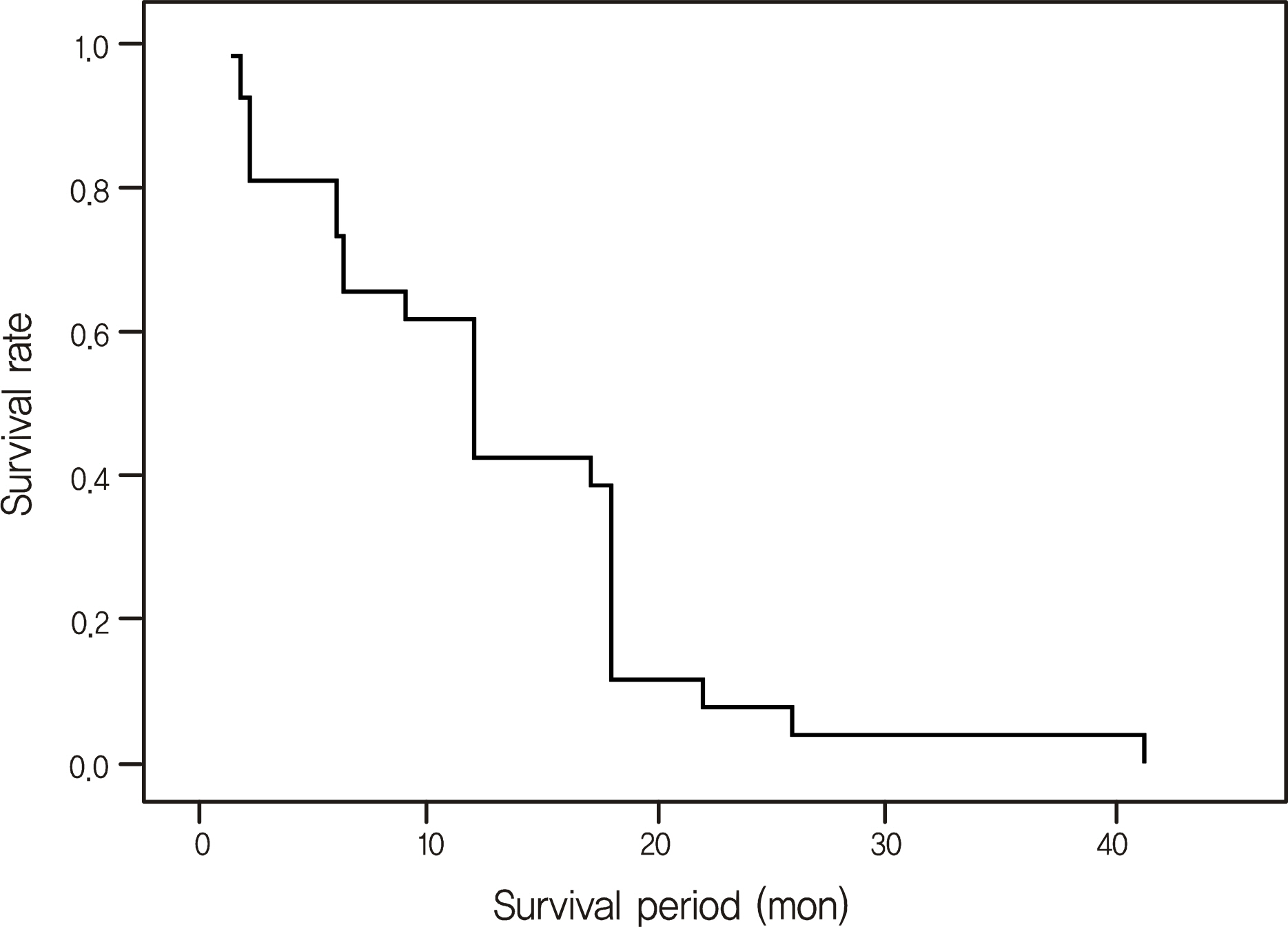
The most common primary indications were herpes simplex keratitis (26.9%), followed by fungal keratitis (19.2%) and bacterial keratitis (11.5%). The average survival period of graft in three or more PKP was 12.9 +/- 9.1 months. As the frequency of PKP increased, the survival period became shorter; the survival period was the longest in pseudophakic bullous keratopathy and the shortest in herpes simplex keratitis. The most common cause of graft failure was allograft rejection (82.8%), and the risk factors for graft failure were short interval between penetrating keratoplasties and corneal neovascularization.
CONCLUSIONS
In three or more PKP, as the frequency of PKP increases, the survival period becomes shorter. Short interval between keratoplasties and cornel neovascularization were risk factors for graft failure; this results must be considered before surgery.
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Retained Descemet's Membrane after Penetrating Keratoplasty
Chi Shian Feng, Won Seok Choi, Woo Ho Nam, Young Joo Shin
J Korean Ophthalmol Soc. 2013;54(5):813-817. doi: 10.3341/jkos.2013.54.5.813.
Reference
-
References
1. Choi SH, Lee YW, Kim HM, et al. Epidemiologic Studies of Keratoplsty in Korea. J Korean Ophthalmol Soc. 2006; 47:538–47.2. Boisjoly HM, Tourigny R, Bazin R, et al. Risk factors of corneal graft failure. Ophthalmology. 1993; 100:1728–35.
Article3. Kim EC, Kim MS. Graft rejection in penetrating keratoplasty. J Korean Ophthalmol Soc. 2003; 44:289–95.4. Weisbrod DJ, Sit M, Naor J, Slomovic AR. Outcomes of repeat penetrating keratoplasty and risk factors for graft failure. Cornea. 2003; 22:429–34.
Article5. Yildiz EH, Hoskins E, Fram N, et al. Third or greater penetrating keratoplasties: indications, survival, and visual outcomes. Cornea. 2010; 29:254–9.
Article6. Tchah HW, Ha DW, Kim CK, et al. Penetrating keratoplasty results in 275 cases. J Korean Ophthalmol Soc. 2001; 42:20–9.7. Yoon KC, Park YK, Park YG. Surgical results of repeat penetrating keratoplasty and risk factors for graft failure. J Korean Ophthalmol Soc. 2004; 45:1827–32.8. Djalilian AR, Nussenblatt RB, Holland EJ. Immnunosuppressive therapy in ocular surface transplantation. Holland EJ, Mannis MJ, editors. Ocular Surface Disease Medical and Surgical Management. 1st ed.New York: Springer;2002. 1:chap. 22.9. Halberstadt M, Machens M, Gahlenbek KA, et al. The outcome of corneal grafting in patients with stromal keratitis of herpetic and non-herpetic origin. Br J Ophthalmol. 2002; 86:646–52.
Article10. Robinson CH. Indications, complications and prognosis for repeat penetrating keratoplasty. Ophthalmic Surg. 1979; 10:27–34.11. Rapuano CJ, Cohen EJ, Brady SE, et al. Indications for and outcomes of repeat penetrating keratoplasty. Am J Ophthalmol. 1990; 15:689–95.
Article12. Maeno A, Naor J, Lee HM, et al. Three decades of corneal transplantation: indications and patient characteristics. Cornea. 2000; 19:7–11.
Article13. MacEwen CJ, Khan ZU, Anderson E, MacEwen CG. Corneal re-graft: indications and outcome. Ophthalmic Surg. 1988; 19:706–12.
Article14. Patel NP, Kim T, Rapuano CJ, et al. Indications for and outcomes of repeat penetrating keratoplasty, 1989-1995. Ophthalmology. 2000; 107:719–24.
Article15. Vanathi M, Sharma N, Sinha R, et al. Indications and outcome of repeat penetrating keratoplasty in india. BMC Ophthalmol. 2005; 5:26.
Article16. Al-Mezaine H, Wagoner MD, King Khaled Eye Specialist Hospital Cornea Transplant Study Group. Repeat penetrating keratoplasty: indication, graft survival, and visual outcome. Br J Ophthalmol. 2006; 90:324–7.17. Bersudsky V, Blum-Hareuveni T, Rehany U, Rumelt S. The profile of repeated corneal transplantation. Ophthalmology. 2001; 108:461–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in Corneal Transplantation Revealed by KONOS and Health Insurance Review and Assessment Service Annual Reports
- Clinical Results of Corneal Triple Procedure and Risk Factors for Graft Failure
- Risk Factors of Graft Failure in Post-Keratoplasty Ocular Hypertension
- Surgical Results of Repeat Penetrating Keratoplasty and Risk Factors for Graft Failure
- Descemet Stripping Automated Endothelial Keratoplasty for Repeated Penetrating Keratoplasty Graft Failure