J Korean Ophthalmol Soc.
2011 Oct;52(10):1215-1221. 10.3341/jkos.2011.52.10.1215.
Effect of Mitomycin C, Dexamethasone, and Cyclosporine A 0.05% on the Proliferation of Human Corneal Keratocytes
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University College of Medicine, Busan, Korea. jongsool@pusan.ac.kr
- 2Department of Ophthalmology, Pusan National University Yangsan Hospital, Busan, Korea.
- KMID: 2215005
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1215
Abstract
- PURPOSE
To investigate the biologic effect of mitomycin C, dexamethasone and cyclosporine A 0.05% on cultured human keratocytes in vitro.
METHODS
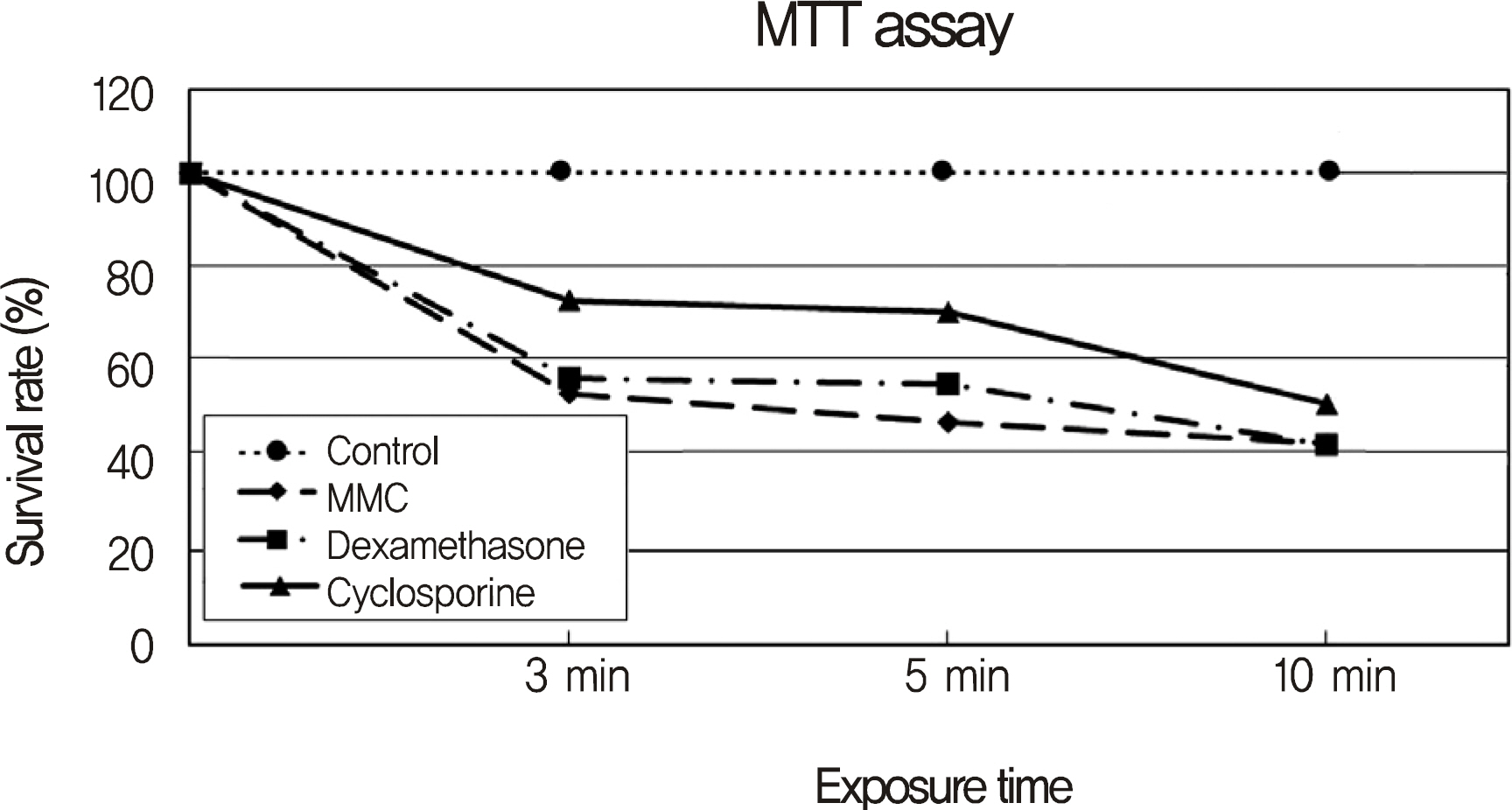
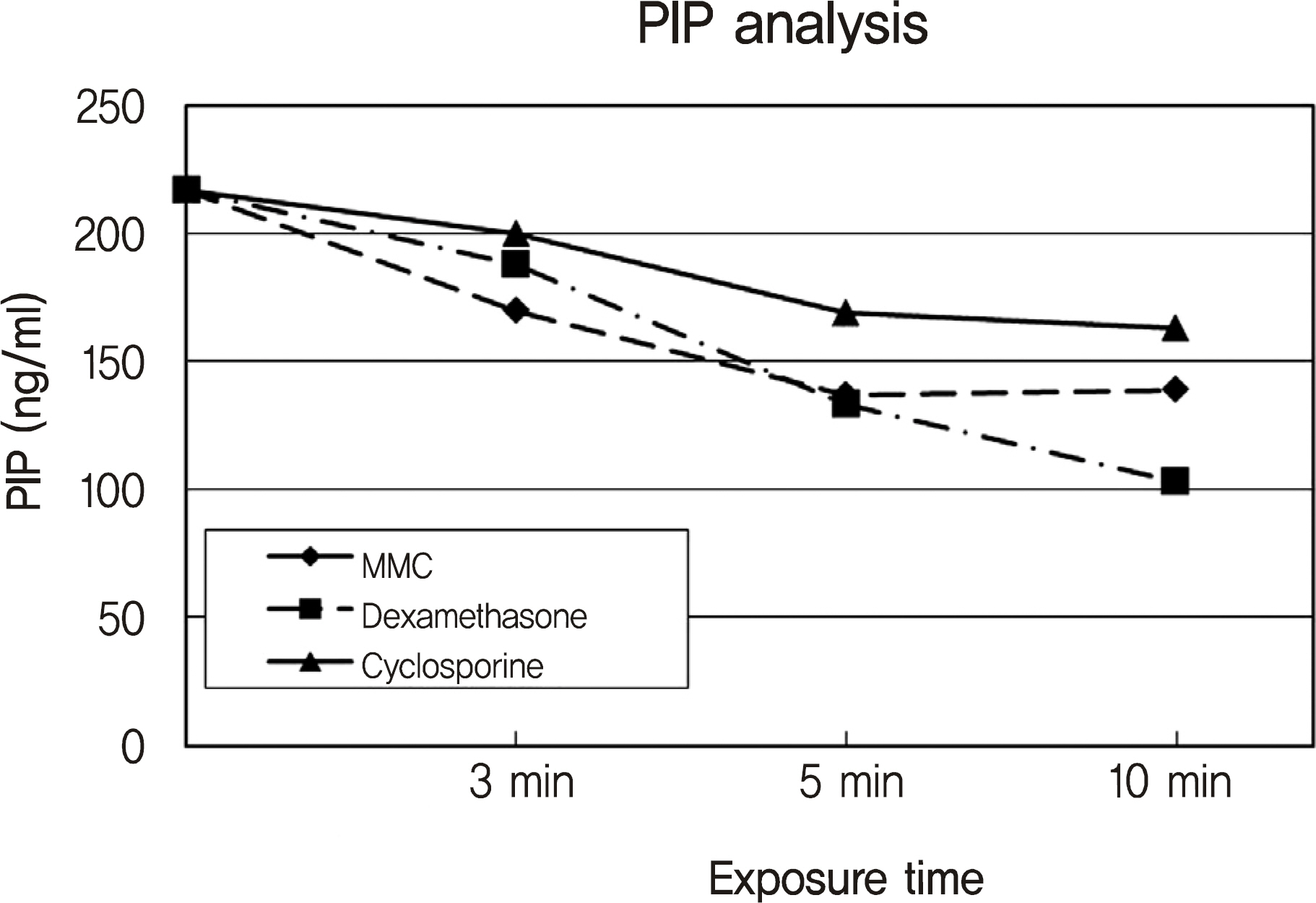
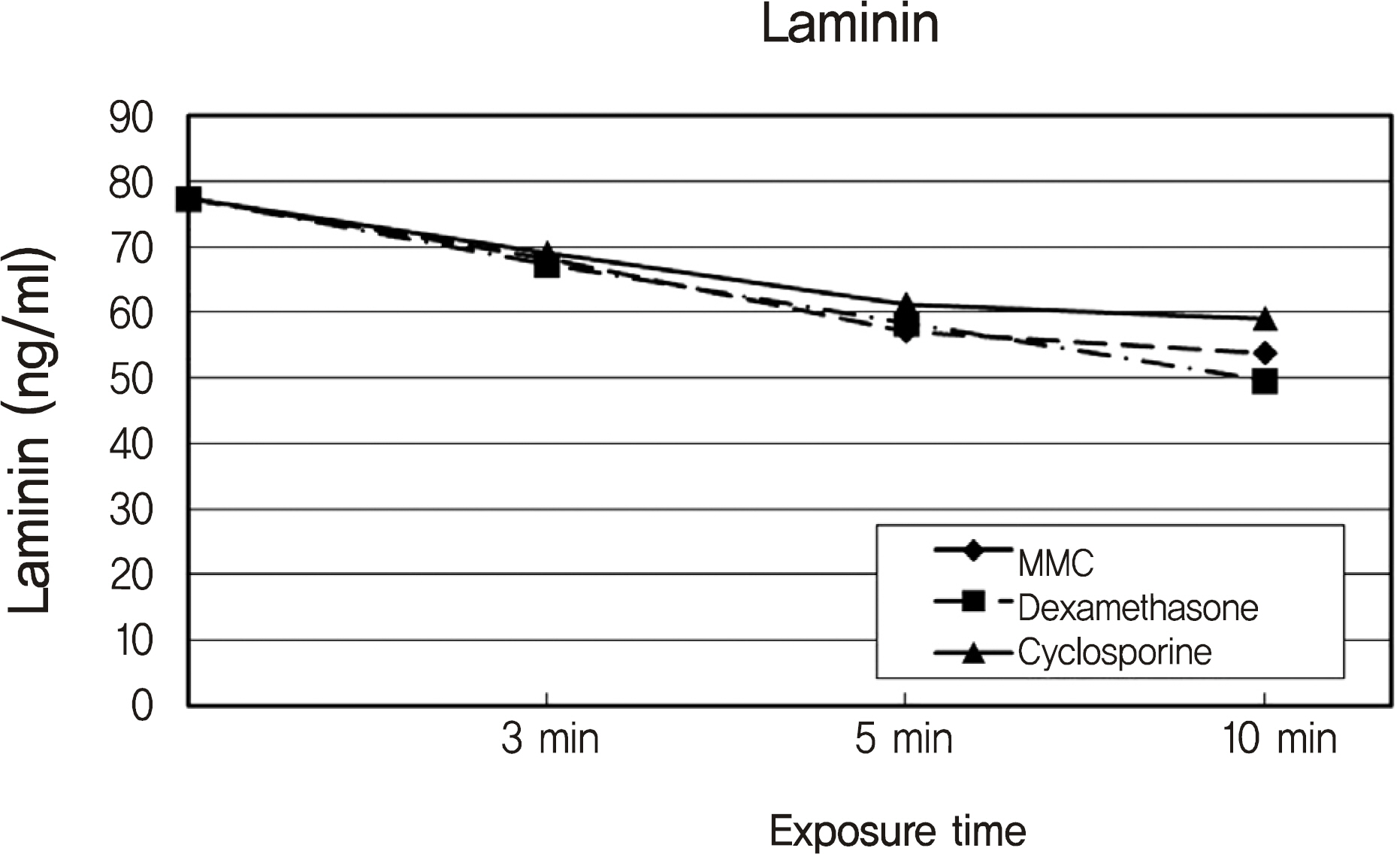
Human corneal keratocytes were exposed to a concentration of mitomycin C (0.05%), dexamethasone (0.05%) and cyclosporine A (0.05%) for a period of 3, 5, and 10 minutes. MTT-based colorimetric assay was performed to assess the metabolic activity of cellular proliferation and the concentration of type I procollagen COOH-terminal peptide (PIP) and laminin were measured. Cell damage was determined by using the lactate dehydrogenase (LDH) assay. Apoptotic response was evaluated utilizing flow cytometric analysis with Annexin V and propiodium iodide.
RESULTS
The inhibitory effect of cellular proliferation and cytotoxicity in cultured human keratocytes showed a time-dependent response in all drugs. The production of PIP and laminin showed a time-dependent response in cultured cells. Apoptosis was observed in flow cytometry after being treated with mitomycin C, dexamethasone and cyclosporine A. Cyclosporin A resulted in less apoptosis of keratocytes than mitomycin C and dexamethasone.
CONCLUSIONS
The apoptotic response of mitomycin C, dexamethasone and cyclosporine A is associated with the inhibitory effect of human corneal keratocyte proliferation. To decrease corneal opacity, mitomycin C and dexamethasone were more effective than cyclosporine A in the present study. Additionally, a high concentration of cyclosporine A greater than 0.05% is necessary to lower corneal opacity.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Salomao MQ, Wilson SE. Corneal molecular and cellular biology update for the refractive surgeon. J Refract Surg. 2009; 25:459–66.
Article2. Nishida T, Yasumoto K, Otori T, Desaki J. The network structure of corneal fibroblasts in the rat as revealed by scanning electron microscopy. Invest Ophthalmol Vis Sci. 1988; 29:1887–90.3. Bergman RH, Spigelman AV. The role of fibroblast inhibitors on corneal healing following photorefractive keratectomy with 193-nanometer excimer laser in rabbits. Ophthalmic Surg. 1994; 25:170–4.
Article4. Gartry DS, Muir MG, Lohmann CP, Marshall J. The effect of topical corticosteroids on refractive outcome and corneal haze after photorefractive keratectomy: A prospective, randomized, double blind trial. Arch Ophthalmol. 1992; 110:944–52.5. de Benito-Llopis L, Teus MA, Sánchez-Pina JM. Comparison between LASEK with mitomycin C and LASIK for the correction of myopia of −7.00 to −13.75 D. J Refract Surg. 2008; 24:516–23.6. Carones F, Vigo L, Scandola E, Vacchini L. Evaluation of the prophylactic use of mitomycin-C to inhibit haze formation after photorefractive keratectomy. J Cataract Refract Surg. 2002; 28:2088–95.
Article7. Ursea R, Purcell TL, Tan BU, et al. The effect of cyclosporine A (Restasis) on recovery of visual acuity following LASIK. J Refract Surg. 2008; 24:473–6.
Article8. Tani E, Katakami C, Negi A. Effects of various eye drops on corneal wound healing after superficial keratectomy in rabbits. Jpn J Ophthalmol. 2002; 46:488–95.
Article9. Sher NA, Chen V, Bowers RA, et al. The use of the 193 nm excimer laser for myopic photorefractive keratectomy in sighted eyes. A multicenter study. Arch Ophthalmol. 1991; 109:1525–30.10. Carones F, Brancato R, Venturi E, et al. Efficacy of corticosteroids in reversing regression after myopic photorefractive keratectomy. Refract Corneal Surg. 1993; 9:S52–6.
Article11. Obrart DP, Lohmann CP, Klonos G, et al. The effects of topical corticosteroids and plasmin inhibitors on refractive outcome, haze and visual performance after photorefractive keratectomy; A prospective, randomized observer-masked study. Ophthalmology. 1994; 101:1565–74.12. Stevenson D, Tauber J, Reis BL. Efficacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-severe dry eye disease: a dose-ranging, randomized trial. The Cyclosporin A Phase 2 Study Group. Ophthalmology. 2000; 107:967–74.13. BenEzra D, Maftzir G. Ocular penetration of cyclosporin A: the rabbit eye. Invest Ophthalmol Vis Sci. 1990; 31:1362–6.14. Lee JE, Shin WB, Lee JS. Effect of cyclosporine A 0.05% on human corneal epithelial cells. J Korean Ophthalmol Soc. 2007; 48:1399–409.
Article15. Hingorani M, Calder VL, Buckley RJ, Lightman S. The immunomodulatory effect of topical cyclosporine A in atopic keratoconjunctivitis. Invest Ophthalmol Vis Sci. 1999; 40:392–9.16. Soya K, Obata H, Amano S, et al. Effects of topical corticosteroids on subepithelial haze after excimer laser corneal surgery-objective and quantitative method for evaluationg haze. Nippon Ganka Gakkai Zasshi. 1997; 101:152–7.17. Furukawa H, Nakayasu K, Gotoh T, et al. Effect of topical tranilast and corticosteroids on subepithelial haze after photorefractive keratectomy in rabbits. J Refract Surg. 1997; 13:s457–8.
Article18. Argento C, Cosentino MJ, Ganly M. Comparison of laser epithelial keratomileusis with and without the use of mitomycin C. J Refract Surg. 2006; 22:782–6.
Article19. Okamoto S, Sakai T, Iwaki Y, et al. Effects of tranilast on cultured rabbit corneal keratocytes and corneal haze after photorefractive keratectomy. Jpn J Ophthalmol. 1999; 43:355–62.
Article20. Lai YH, Wang HZ, Lin CP, Chang SJ. Mitomycin C alters corneal stromal wound healing and corneal haze in rabbits after argon-flu-oride excimer laser photorefractive keratectomy. J Ocul Pharmacol Ther. 2004; 20:129–38.
Article21. Lee JE, Lee JS. Inhibitory effect of mitomycin C(MMC) on the proliferation of human corneal keratocyte. J Korean Ophthalmol Soc. 2002; 43:2519–26.22. Netto MV, Mohan RR, Sinha S, et al. Effect of prophylactic and therapeutic mitomycin C on corneal apoptosis, cellular proliferation, haze, and long-term keratocyte density in rabbits. J Refract Surg. 2006; 22:562–74.
Article23. Lee JE, Lee SU, Kim JH, Lee JS. Effect of dexamethasone and diclofenac on the proliferation of human corneal keratocytes. J Korean Ophthalmol Soc. 2005; 46:133–43.24. Berman B, Duncan MR. Pentoxifylline inhibits normal human dermal fibroblast in vitro proliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity. J Invest Dermatol. 1989; 92:605–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Dexamethasone and Diclofenac on the Proliferation of Human Corneal Keratocytes
- The Effect of Candida albicans and Dexamethasone on the Secretion of Tumor Necrosis Factor-alpha from Cultured Human Keratocytes
- Effect of Anti-inflammatory Mediator on the Proliferation of Human Corneal Keratocyte
- Inhibitory Effect of Mitomycin C (MMC) on the Proliferation of Human Corneal Keratocyte
- Effect of Tranilast on the Proliferation of Human Corneal Keratocytes in Vitro