J Korean Ophthalmol Soc.
2011 Mar;52(3):293-298. 10.3341/jkos.2011.52.3.293.
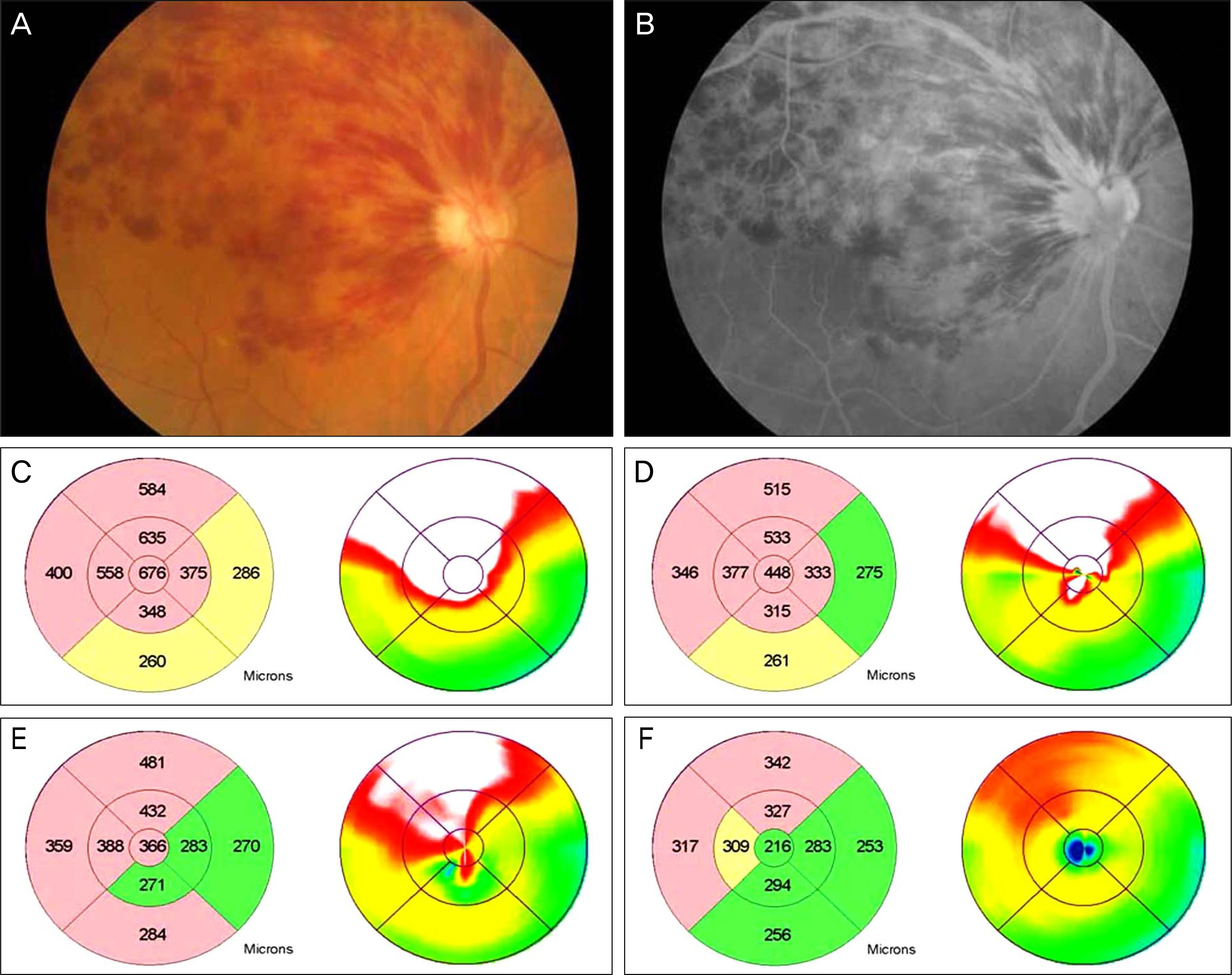
Intravitreal Bevacizumab for Treatment of Macular Edema Secondary to Hemicentral Retinal Venous Occlusion and Concentrations of Cytokine in Aqueous Humor
- Affiliations
-
- 1Department of Ophthalmology, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea. jiwoneye@hallym.or.kr
- KMID: 2214293
- DOI: http://doi.org/10.3341/jkos.2011.52.3.293
Abstract
- PURPOSE
To evaluate the effects of intravitreal bevacizumab and to investigate the concentrations of cytokine in the aqueous humors of patients with macular edema secondary to hemicentral retinal venous occlusion.
METHODS
Fifteen eyes of 15 patients with macular edema secondary to hemicentral retinal venous occlusion received intravitreal bevacizumab injections and completed 12 months of follow-up. Cytokine levels were measured in the aqueous humors of these patients using a multiplex bead assay and the levels were compared with those of the controls.
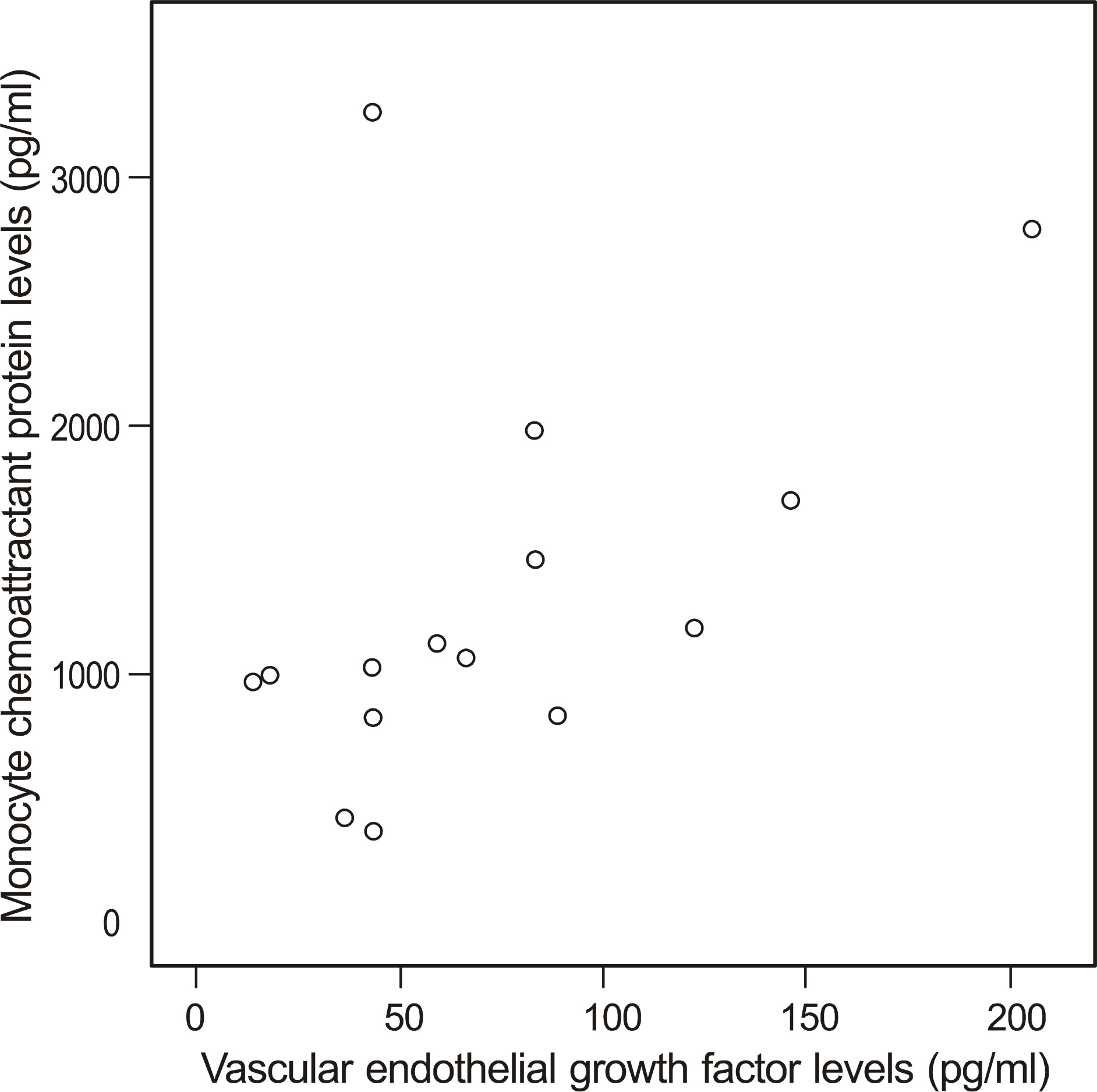
RESULTS
During 12 months of follow-up, a mean of 4.5 intravitreal bevacizumab injections were performed. The visual acuity and the central macular thickness improved significantly (p = 0.028, p = 0.000) after treatment. The levels of interleukin-6, vascular endothelial growth factor, and monocyte chemoattractant protein-1 were increased in the aqueous humor compared with the levels in the control group (p = 0.010, p = 0.045, p < 0.001).
CONCLUSIONS
Elevated cytokine levels were identified in the aqueous humor after hemicentral retinal venous occlusion. Intravitreal bevacizumab injections were effective for improvements in visual acuity and macular edema due to hemicentral retinal venous occlusion.
MeSH Terms
Figure
Reference
-
References
1. Hayreh SS, Hayreh MS. Hemicentral retinal vein occulsion. Pathogenesis, clinical features, and natural history. Arch Ophthalmol. 1980; 98:1600–9.2. Chopdar A. Hemicentral retinal vein occlusion. Pathogenesis, clinical features, natural history and incidence of dual trunk central retinal vein. Trans Ophthalmol Soc U K. 1982; 102:241–8.3. Rosenfeld PJ, Fung AE, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg Lasers Imaging. 2005; 36:336–9.
Article4. Ferrara DC, Koizumi H, Spaide RF. Early bevacizumab treatment of central retinal vein occlusion. Am J Ophthalmol. 2007; 144:864–71.
Article5. Lee HK, Kim HW, Yun IH. Intravitreal bevacizumab injection for macular edema secondary to branch retinal vein occlusion. J Korean Ophthalmol Soc. 2009; 50:1800–8.
Article6. Hoeh AE, Ach T, Schaal KB, et al. Long-term followup of OCT-guided bevacizumab treatment of macular edema due to retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2009; 247:1635–41.
Article7. Nghiem-Buffet S, Cohen SY. Retinal vein occlusion: anti-VEGF treatments. J Fr Ophtalmol. 2009; 32:679–86.8. Fish GE. Intravitreous bevacizumab in the treatment of macular edema from branch retinal vein occlusion and hemisphere retinal vein occlusion (an AOS thesis). Trans Am Ophthalmol Soc. 2008; 106:276–300.9. Hayashi A, Ueta Y, Yunoki T, et al. Short-term effects of intravitreal injection of bevacizumab on macular edema due to central retinal vein occlusion. Nippon Ganka Gakkai Zasshi. 2010; 114:347–55.10. Noma H, Funatsu H, Yamasaki M, et al. Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye. 2008; 22:42–8.
Article11. Funatsu H, Yamashita H, Noma H, et al. Aqueous humor levels of cytokines are related to vitreous levels and progression of diabetic retinopathy in diabetic patients. Graefes Arch Clin Exp Ophthalmol. 2005; 243:3–8.
Article12. Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology. 2007; 114:855–9.
Article13. Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994; 331:1480–7.
Article14. Boyd SR, Zachary I, Chakravarthy U, et al. Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion. Arch Ophthalmol. 2002; 120:1644–50.
Article15. Cohen T, Nahari D, Cerem LW, et al. Interleukin 6 induces the expression of vascular endothelial growth factor. J Biol Chem. 1996; 271:736–41.
Article16. Funk M, Kriechbaum K, Prager F, et al. Intraocular concentrations of growth factors and cytokines in retinal vein occlusion and the effect of therapy with bevacizumab. Invest Ophthalmol Vis Sci. 2009; 50:1025–32.
Article17. Noma H, Funatsu H, Yamasaki M, et al. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. Am J Ophthalmol. 2005; 140:256–61.
Article18. Noma H, Funatsu H, Mimura T, et al. Vitreous levels of inter-leukin-6 and vascular endothelial growth factor in macular edema with central retinal vein occlusion. Ophthalmology. 2009; 116:87–93.
Article19. Schober A, Zernecke A. Chemokines in vascular remodeling. Thromb Haemost. 2007; 97:730–7.
Article20. Hoshino M, Takahashi M, Aoike N. Expression of vascular endothelial growth factor, basic fibroblast growth factor, and angioge-nin immunoreactivity in asthmatic airways and its relationship to angiogenesis. J Allergy Clin Immunol. 2001; 107:295–301.
Article21. Krohne TU, Eter N, Holz FG, Meyer CH. Intraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humans. Am J Ophthalmol. 2008; 146:508–12.
Article22. Choi SW, Kim HW, Yun IH. Intravitreal bevacizumab treatment of macular edema in central retinal vein occlusion. J Korean Ophthalmol Soc. 2010; 51:707–15.
Article23. Wu L, Arevalo JF, Berrocal MH, et al. Comparison of two doses of intravitreal bevacizumab as primary treatment for macular edema secondary to central retinal vein occlusion: results of the pan American collaborative retina study group at 24 months. Retina. 2010; 30:1002–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Intravitreal Bevacizumab Injection in 3 Types of Macular Edema Secondary to Branch Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion: Long-Term Results
- A Case of Retinal Hemorrhage Following a Dexamethasone Intravitreal Implant
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion