J Korean Ophthalmol Soc.
2009 Dec;50(12):1800-1808. 10.3341/jkos.2009.50.12.1800.
Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Pusan Paik Hospital, Inje University College of Medicine, Busan, Korea. maekbak@hanmail.net
- KMID: 2212991
- DOI: http://doi.org/10.3341/jkos.2009.50.12.1800
Abstract
- PURPOSE
To examine the clinical effects of intravitreal bevacizumab injections for patients with macular edema secondary to branched retinal vein occlusion (BRVO).
METHODS
Nineteen patients (19 eyes) diagnosed with BRVO within the three month study window, having visual acuities under 0.5 and significant macular edema within two-disc diameters of the fovea were included in the present study. The author evaluated the patients' responses to bevacizumab (1.25 mg/0.05 mL) treatment using visual acuity and central macular edema measurements.
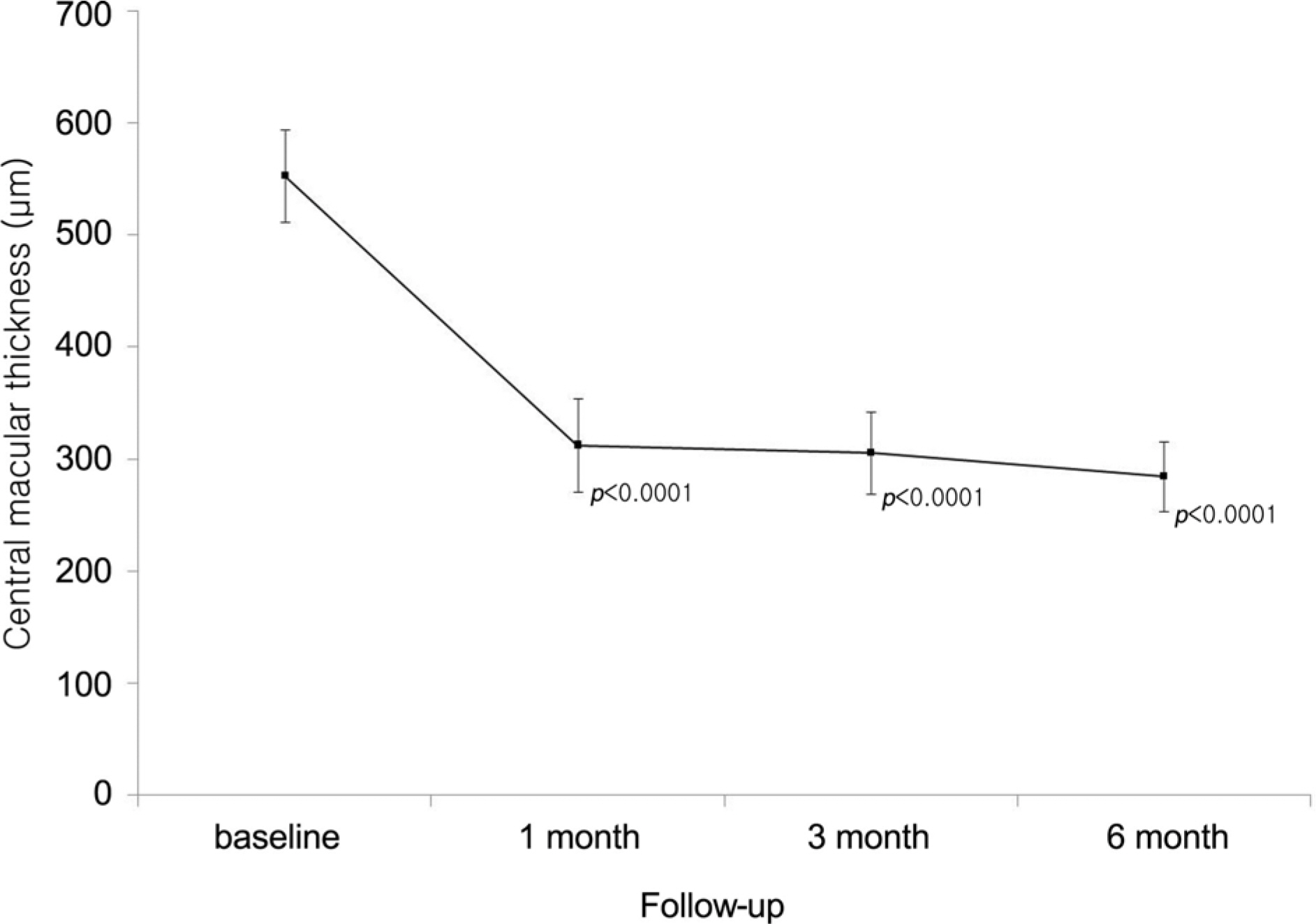
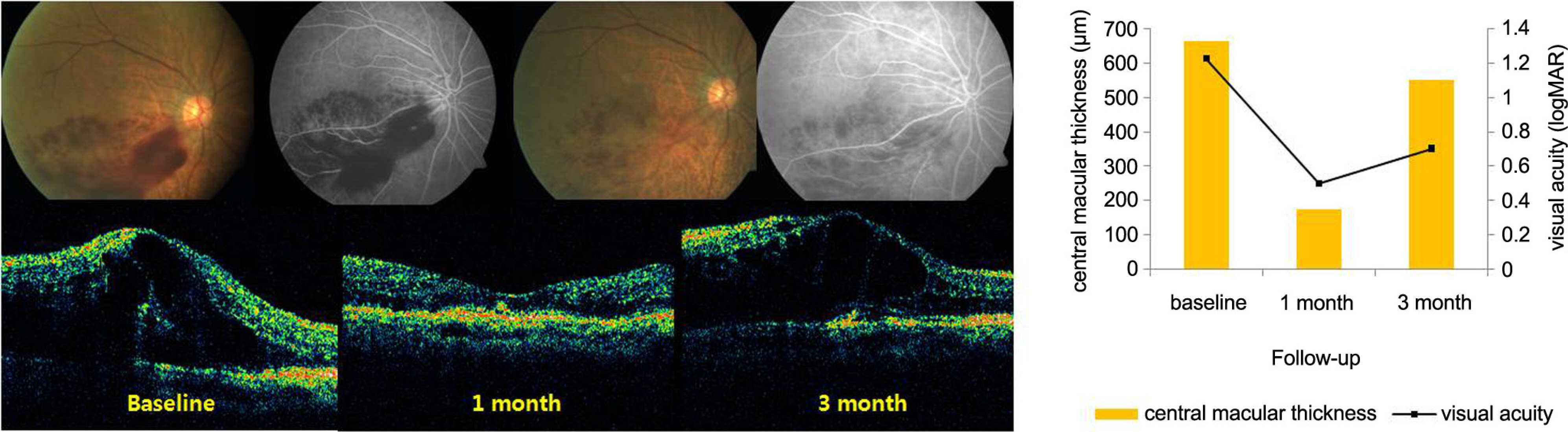
RESULTS
The mean visual acuity improved from 1.06 (+/-0.10 logMAR unit) at baseline to 0.68 (+/-0.09 logMAR unit), 0.279 (+/-0.049) at one month, 0.67 (+/-0.9 logMAR unit) at two months, 0.61 (+/-0.09 logMAR unit) at three months and 0.54 (+/-0.10 logMAR unit) at six months. The mean central macular thickness decreased from 552.9 micrometer (+/-41.0) at baseline to 290.0 micrometer (+/-36.7) at one month, 290.0 micrometer (+/-36.7) at three months and 281.3 micrometer (+/-30.1) at six months. No adverse side effects were observed following injections.
CONCLUSIONS
The observed macular edema and visual acuity improvements, as well as lack of serious adverse side effects after intravitreal bevacizumab injection, demonstrated that intravitreal bevacizumab injection may be useful for treating patients with macular edema secondary to BRVO.
MeSH Terms
Figure
Cited by 2 articles
-
Intravitreal Bevacizumab for Treatment of Macular Edema Secondary to Hemicentral Retinal Venous Occlusion and Concentrations of Cytokine in Aqueous Humor
Su Jeong Ryu, Ji Won Lim
J Korean Ophthalmol Soc. 2011;52(3):293-298. doi: 10.3341/jkos.2011.52.3.293.Two Cases of Macular Edema Associated with Extramacular Branch Retinal Vein Occlusion
Dong Min Cha, Sun Ho Lee, Hye Jin Lee, Jin Ho Jeong
J Korean Ophthalmol Soc. 2016;57(2):330-333. doi: 10.3341/jkos.2016.57.2.330.
Reference
-
References
1. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol. 1996; 114:1243–7.2. Rehak J, Rehak M. Branch retinal vein occlusion: pathogenesis, visual prognosis, and treatment modalities. Curr Eye Res. 2008; 33:111–31.
Article3. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–82.4. Cekic O, Chang S, Tseng JJ, et al. Intravitreal triamcinolone injection for treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2005; 25:851–5.
Article5. Chen SD, Sundaram V, Lochhead J, Patel CK. Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006; 141:876–83.
Article6. Ozkiris A, Evereklioglu C, Erkilic K, Dogan H. Intravitreal triamcinolone acetonide for treatment of persistent macular oedema in branch retinal vein occlusion. Eye. 2006; 20:13–7.
Article7. Avitabile T, Longo A, Reibaldi A. Intravitreal triamcinolone compared with macular laser grid photocoagulation for the treatment of cystoid macular edema. Am J Ophthalmol. 2005; 140:695–702.
Article8. Jaissle GB, Szurman P, Bartz-Schmidt KU. Ocular side effects and complications of intravitreal triamcinolone acetonide injection. Ophthalmologe. 2004; 101:121–8.9. Ferrara N, Hillan KJ, Gerber HP, Novotny W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov. 2004; 3:391–400.
Article10. Astam N, Batioglu F, Ozmert E. Short-term efficacy of intravitreal bevacizumab for the treatment of macular edema due to diabetic retinopathy and retinal vein occlusion. Int Ophthalmol. 2009; 29:543–8.
Article11. Avery RL, Pearlman J, Pieramici DJ, et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology. 2006; 113:1695.
Article12. Mandal S, Venkatesh P, Sampangi R, Garg S. Intravitreal bevacizumab (Avastin) as primary treatment for myopic choroidal neovascularization. Eur J Ophthalmol. 2007; 17:620–6.
Article13. Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994; 331:1480–7.
Article14. Iturralde D, Spaide RF, Meyerle CB, et al. Intravitreal bevacizumab (Avastin) treatment of macular edema in central retinal vein occlusion: a short-term study. Retina. 2006; 26:279–84.15. Jaissle GB, Ziemssen F, Petermeier K, et al. Bevacizumab for treatment of macular edema secondary to retinal vein occlusion. Ophthalmologe. 2006; 103:471–5.16. Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000; 98:133–41.17. Noma H, Minamoto A, Funatsu H, et al. Intravitreal levels of vascular endothelial growth factor and interleukin-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2006; 244:309–15.
Article18. Arnarsson A, Stefansson E. Laser treatment and the mechanism of edema reduction in branch retinal vein occlusion. Invest Ophthalmol Vis Sci. 2000; 41:877–9.19. Silva RM, Faria de Abreu JR, Cunha-Vaz JG. Blood-retina barrier in acute retinal branch vein occlusion. Graefes Arch Clin Exp Ophthalmol. 1995; 233:721–6.
Article20. Stefansson E. The therapeutic effects of retinal laser treatment and vitrectomy. A theory based on oxygen and vascular physiology. Acta Ophthalmol Scand. 2001; 79:435–40.21. Kalogeropoulos C, Donati G, Pizzolato GP, Pournaras CJ. Morphology of early retinal lesions after experimental venous occlusion. Klin Monatsbl Augenheilkd. 1996; 208:375–6.22. Larsson J, Bauer B, Andreasson S. The 30-Hz flicker cone ERG for monitoring the early course of central retinal vein occlusion. Acta Ophthalmol Scand. 2000; 78:187–90.
Article23. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Arch Ophthalmol. 1986; 104:34–41.24. Battaglia Parodi M, Saviano S, Bergamini L, Ravalico G. Grid laser treatment of macular edema in macular branch retinal vein occlusion. Doc Ophthalmol. 1999; 97:427–31.
Article25. Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992; 110:1155–9.
Article26. Bhavsar AR, Ip MS, Glassman AR. The risk of endophthalmitis following intravitreal triamcinolone injection in the DRCRnet and SCORE clinical trials. Am J Ophthalmol. 2007; 144:454–6.
Article27. Jonas JB, Degenring R, Kreissig I, Akkoyun I. Safety of intravitreal high-dose reinjections of triamcinolone acetonide. Am J Ophthalmol. 2004; 138:1054–5.
Article28. Jonas JB, Degenring RF, Kreissig I, et al. Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Ophthalmology. 2005; 112:593–8.
Article29. Rosenfeld PJ, Fung AE, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg Lasers Imaging. 2005; 36:336–9.
Article30. Rabena MD, Pieramici DJ, Castellarin AA, et al. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2007; 27:419–25.
Article31. Wetzig PC. The treatment of acute branch vein occlusion by photocoagulation. Am J Ophthalmol. 1979; 87:65–73.
Article32. Gutman FA, Zegarra H. The natural course of temporal retinal branch vein occlusion. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:OP178–92.33. Schaal KB, Hoh AE, Scheuerle A, et al. Bevacizumab for the treatment of macular edema secondary to retinal vein occlusion. Ophthalmologe. 2007; 104:285–9.34. Stahl A, Agostini H, Hansen LL, Feltgen N. Bevacizumab in retinal vein occlusion-results of a prospective case series. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1429–36.
Article35. Chung EJ, Hong YT, Lee SC, et al. Prognostic factors for visual outcome after intravitreal bevacizumab for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2008; 246:1241–7.
Article36. Krohne TU, Eter N, Holz FG, Meyer CH. Intraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humans. Am J Ophthalmol. 2008; 146:508–12.
Article37. Stewart MW. Predicted biologic activity of intravitreal bevacizumab. Retina. 2007; 27:1196–200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Intravitreal Bevacizumab Injection in 3 Types of Macular Edema Secondary to Branch Retinal Vein Occlusion
- The Efficacy of Intravitreal Bevacizumab in the Treatment of Macular Edema
- Intravitreal Bevacizumab Injection for Macular Edema Secondary to Branch Retinal Vein Occlusion: Long-Term Results
- Macular Vessel Density Analysis Using Optical Coherence Tomography Angiography before and after Intravitreal Bevacizumab Injection in Branch Retinal Vein Occlusion
- Combined Low Dose Bevacizumab-triamcinolone versus Bevacizumab Single Intravitreal Injection for Branch Retinal Vein Occlusion