J Korean Ophthalmol Soc.
2008 May;49(5):701-705. 10.3341/jkos.2008.49.5.701.
Minimal Stitch Canalicular Repair of Canalicular Lacerations
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Dongguk University, Gyeongju, Korea. 9pqwer@hanmail.net
- KMID: 2211697
- DOI: http://doi.org/10.3341/jkos.2008.49.5.701
Abstract
-
PURPOSE: To examine the results of minimal stitch on the restoration of tissue after canalicular laceration.
METHODS
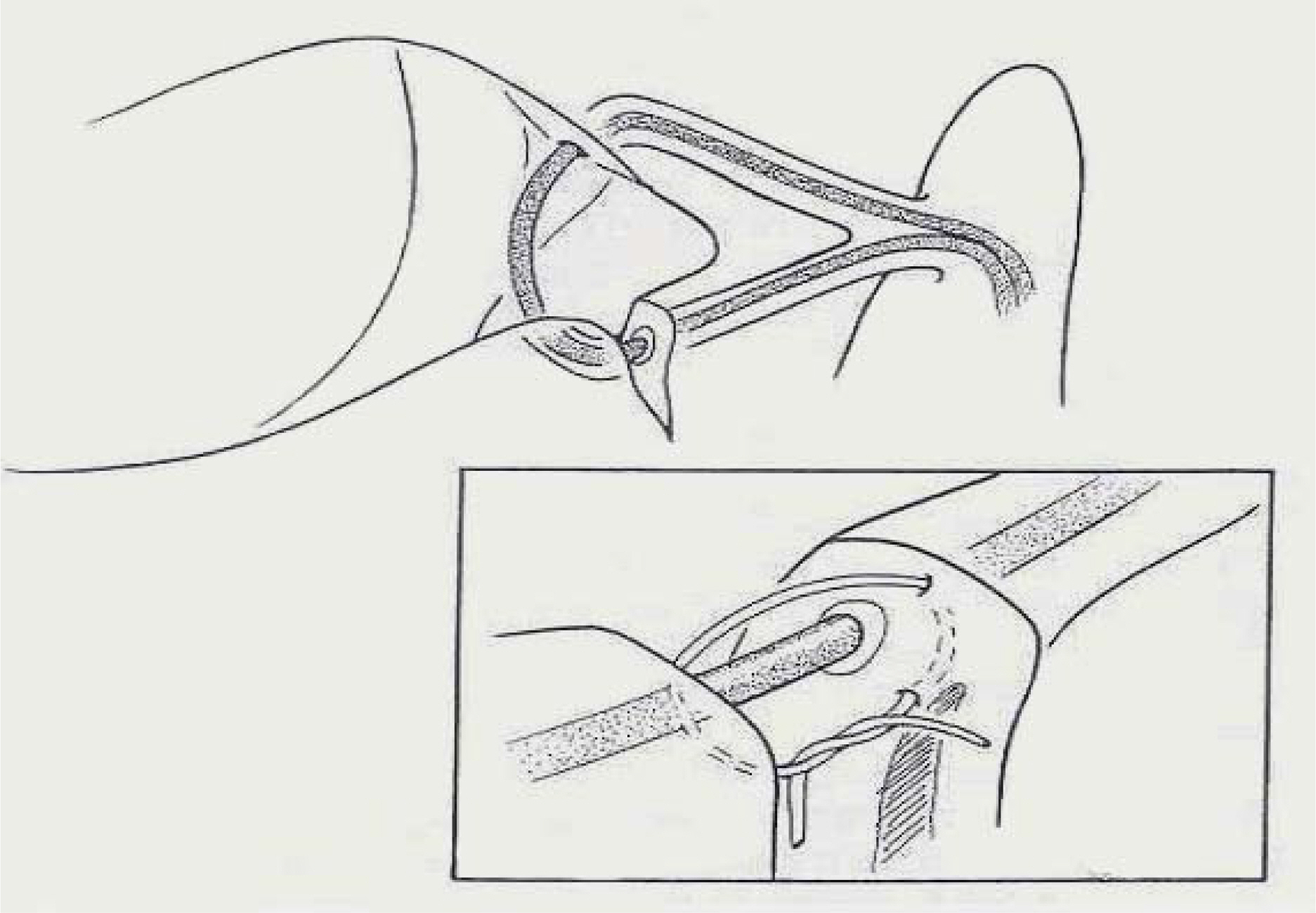
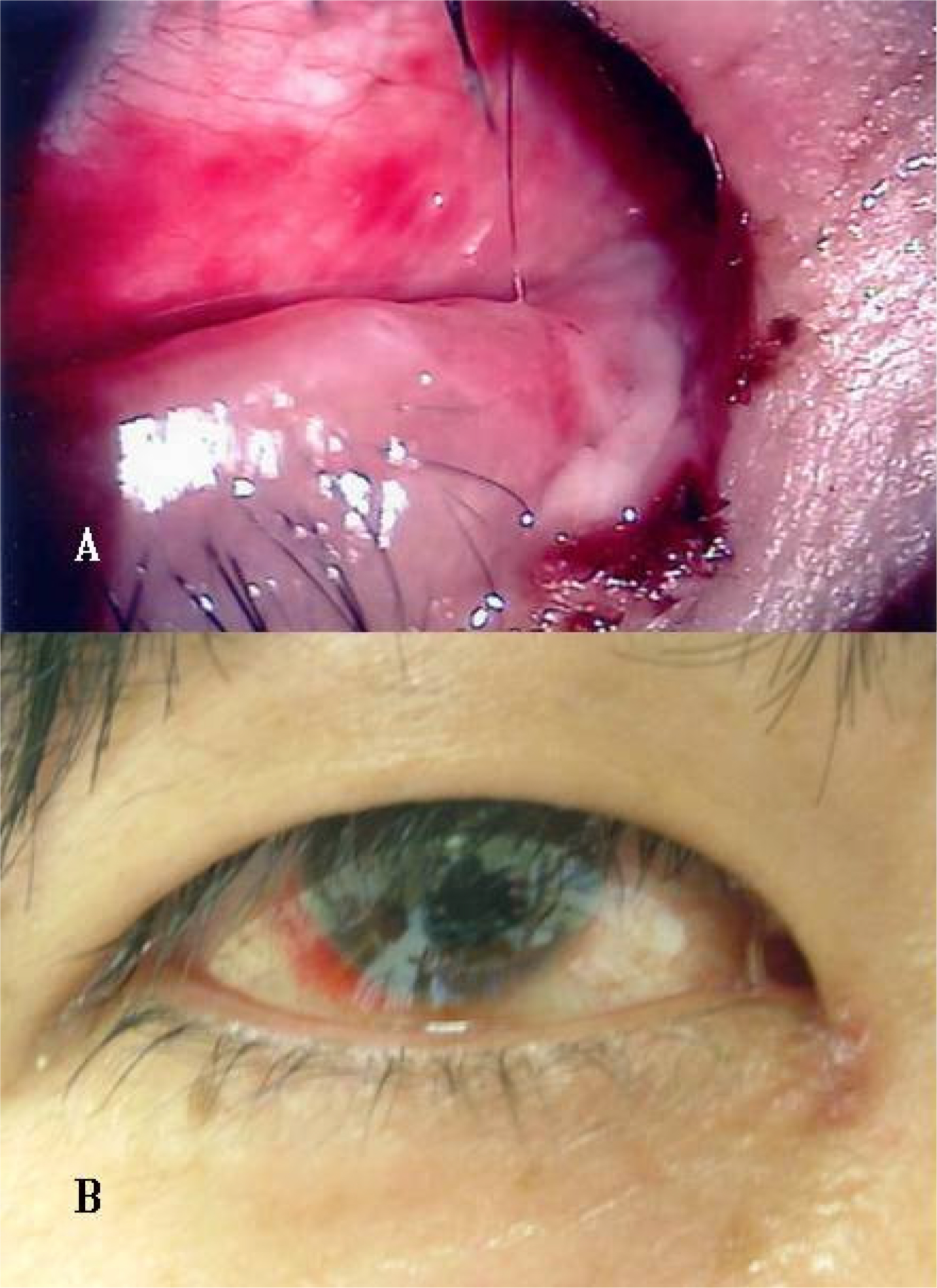
We have operated using sutures of tissues around canalicular laceration by inserting bicanalicular silicone stents and minimal horizontal mattress sutures with 8-0 Vicryl in cases of canalicular laceration instead of the existing method for the past 6 years. The ages of patients ranged from 2 to 76 years (average age 39.8+/-17.4 years), with most patients in their thirties (12 patients, 40%), 30 cases underwent canalicular repair with minimal stitch and bicanalicular silicone stent insertion within 24 hours after trauma. The silicone stent was removed 3 months after the operation if the patient did not complain of epiphroa while the canalicular remained open.
RESULTS
Twenty-five eyes (83.3%) showed symptom improvement and good passage in lacrimal syringing test in 4~12 months (average: 6.8+/-2.2 months) of follow-up study. Complications included one case each of fistula formation, stent prolapse, and wound infection, and two cases of canalicular stenosis.
CONCLUSIONS
We recommend this method because of its satisfying success ratio.
MeSH Terms
Figure
Cited by 1 articles
-
A Clinical Study Associated with Anatomical and Functional Outcomes in the Repair of Canalicular Laceration
Woo Jin Kim, Min Ahn
J Korean Ophthalmol Soc. 2011;52(3):261-265. doi: 10.3341/jkos.2011.52.3.261.
Reference
-
References
1. Hawes MJ, Dorzbach RK, Segrest DR. Lacrimal canalicular trauma. Ophthalmic plastic surgery. 1st ed.1. New York: Raven Press;1994. p. 225–35.2. Kennedy RH, May J, Dailey J, Flanagan JC. Canalicular Laceration. Ophthalmic Plastic Reconstr Surg. 1990; 6:46–53.
Article3. Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi. Ophthalmic Surg. 1985; 16:639–42.
Article4. Wulc AE, Arterberry JF. The pathogenesis of canalicular laceration. Ophthalmology. 1991; 98:1243–9.
Article5. Mark RL. Repair of canalicular lacerations with silicone intubation. Manual of oculoplastic surgery. 2nd ed.1. Washinton: Butterworths;1996. p. 33–6.6. Zoli CL. Microsurgical repair of lacrimal canaliculus in medial canthal trauma. Oculoplastic, Orbital, and Reconstructive Surgery. 1. Baltimore: Wiliams & Wilkins;1988. p. 426–32.7. Kim SY, Kim DC. The Effect of Delayed canaliculoplasty to Canalicular Laceration after Primary Lid Repair. J Korean Ophthalmol Soc. 1999; 40:2651–6.8. Kim MH, Kong SM, Kim HS. Bicnalicular Silicone Intubation of Canalicular Laceration. J Korean Ophthalmol Soc. 1990; 31:533–41.9. Lee KH, Chung WS. Canaliculoplasty using Mini-Monoka® in Monocanalicular Injury. J Korean Ophthalmol Soc. 1995; 36:765–9.10. Seo SH, Chang HK. The Results of Pigtail Probe Canalicular Reconstruction Surgery with Silicone Tube and Methylcellulose. J Korean Ophthalmol Soc. 1993; 34:1178–82.11. Chung JH, Na KS, Choi GJ. The Effectiveness of Canaliculoplasty Using Mini-Monoka® or Bicanalicular Stent for Repair of Upper and Lower Canalicular Laceration. J Korean Ophthalmol Soc. 2000; 41:2138–43.12. Lee CS, Jeong SK, Park YG. Canaliculoplasty Using Mini-Monoka® or Bicanalicular Stent for Repair of Canalicular Laceration. J Korean Ophthalmol Soc. 1999; 40:895–901.13. Hawes MJ, Segrest DR. Effectiveness of bicanalicular silicone intubation in the repair of canailcular lacerations. Ophthal Plast Reconstr Surg. 1985; 51:185–90.14. Pashby RC, Rathbun JE. Silicone tube intubation of the lacrimal drainage system. Arch Ophthalmol. 1979; 7:1318–22.
Article15. Byon DS, Kim YJ, Shyn KH. Clinical Experience of Monocanaliculonasal Stent in Canalicular Laceration. J Korean Ophthalmol Soc. 1995; 36:1079–83.16. Baek SH, Hur H, Park MS. Canaliculoplasty Using Mini-Monoka® (monocanalicular stent) for Repair of Canalicular Laceration. J Korean Ophthalmol Soc. 2001; 42:955–9.17. Kersten RC, Kulwin DR. “One-stitch” Canalicular Repair. A simplified approach for repair of canalicular laceration. Ophthalmology. 1996; 103:785–9.18. Conlon MC, Smith KD, Cadera W, et al. An Animal Model Studying Reconstruction Techniques and Histopathological Changes in Repair of Canalicular Lacerations. Can J Ophthalmol. 1994; 29:3–8.19. Wulc AE, Arterberry JF. The pathogenesis of canalicular laceration. Ophthalmology. 1991; 98:1243–9.
Article20. Katowitz JA. Silicone Tubing in Canalicular Obstructions. Arch Ophthalmol. 1974; 91:456–62.
Article21. Long JA. A method of monocanalicular silicone intubation. Ophthalmic Surg. 1988; 19:204–5.
Article22. Migliori ME, Putterman AM. Silicone intubation for the treatment of congenital lacrimal duct obstruction: successful results removing the tubes after six weeks. Ophthalmology. 1988; 95:792–5.
Article23. Welsh MG, Katowittz JM. Timing of silastic tubing removal after intubation for congenital nasolacrimal duct obstruction. Ophthal Plast Reconst Surg. 1989; 5:43–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Simple New Method for Identifying the Proximal Cut End in Lower Canalicular Laceration
- The Effect of Delayed Canaliculoplasty to Canalicular
- Bicanalicular Silicone Intubation of Canalicular Laceration
- Canaliculodacryocystorhinostomy in Canalicular Obstruction
- Clinical Features Associated With Outcomes of Canalicular Laceration Repair