J Korean Soc Spine Surg.
2002 Dec;9(4):305-312. 10.4184/jkss.2002.9.4.305.
The Changes of Adjacent Segments after Fusions (above 3-levels to L5) in Degenerative Lumbar Spinal Disorders
- Affiliations
-
- 1Department of Orthopaedic Surgery, Eulji University, Daejeon, Korea. ortho@hananet.net
- 2Cheongju St. Mary's Hospital, Korea.
- 3Kon-Kuk University Hospital, Chungju, Korea.
- KMID: 2209712
- DOI: http://doi.org/10.4184/jkss.2002.9.4.305
Abstract
-
STUDY DESIGN: A retrospective study.
OBJECTIVE
To evaluate the usefulness of MRI grading of disc degeneration in determining whether L5-S1 fusion is necessary in degenerative lumbar spinal disorders. SUMMARY OF LITERATURE REVIEW: Changes in adjacent segments are not well understood, after floating fusion has been performed.
MATERIALS AND METHODS
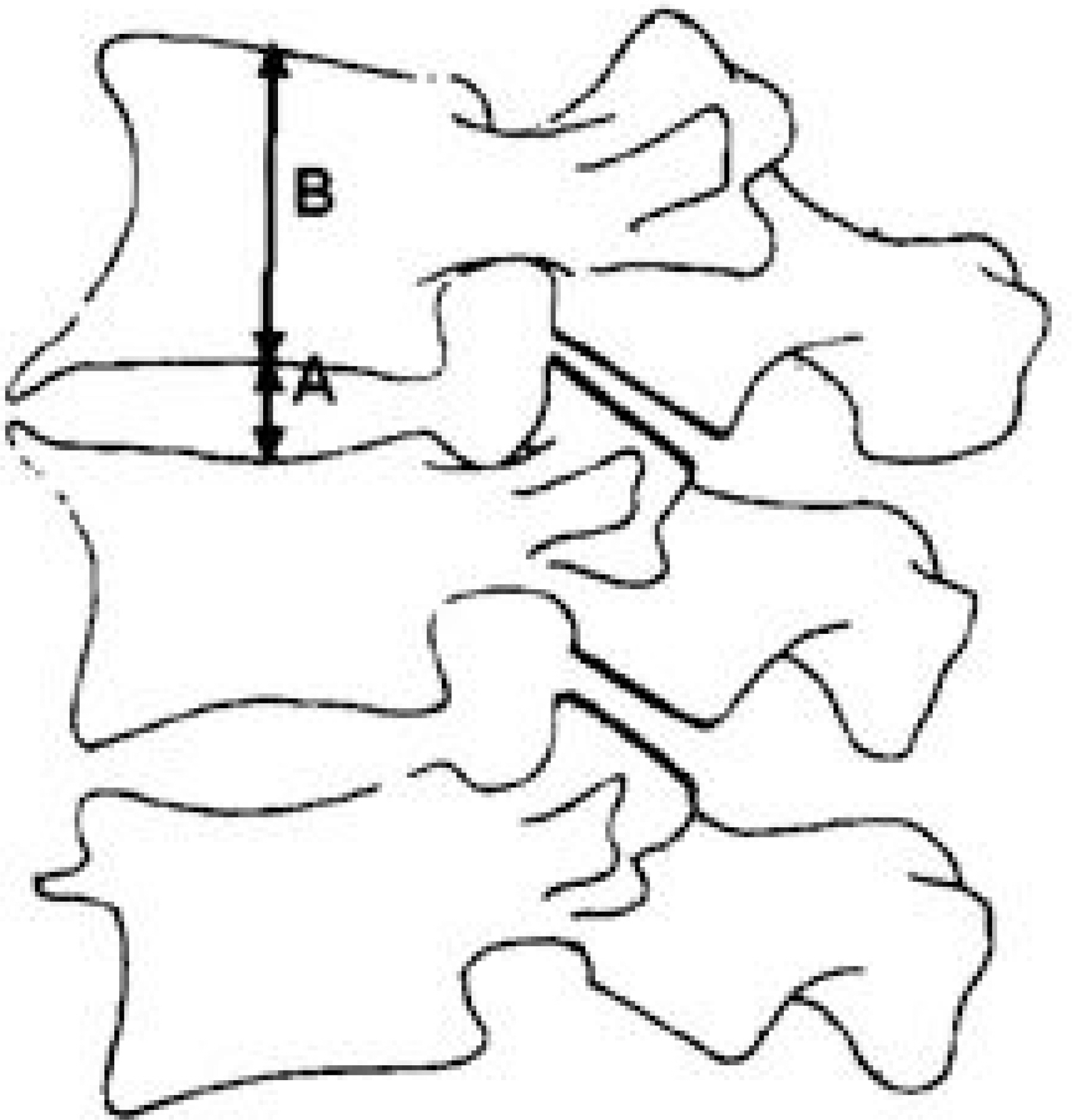
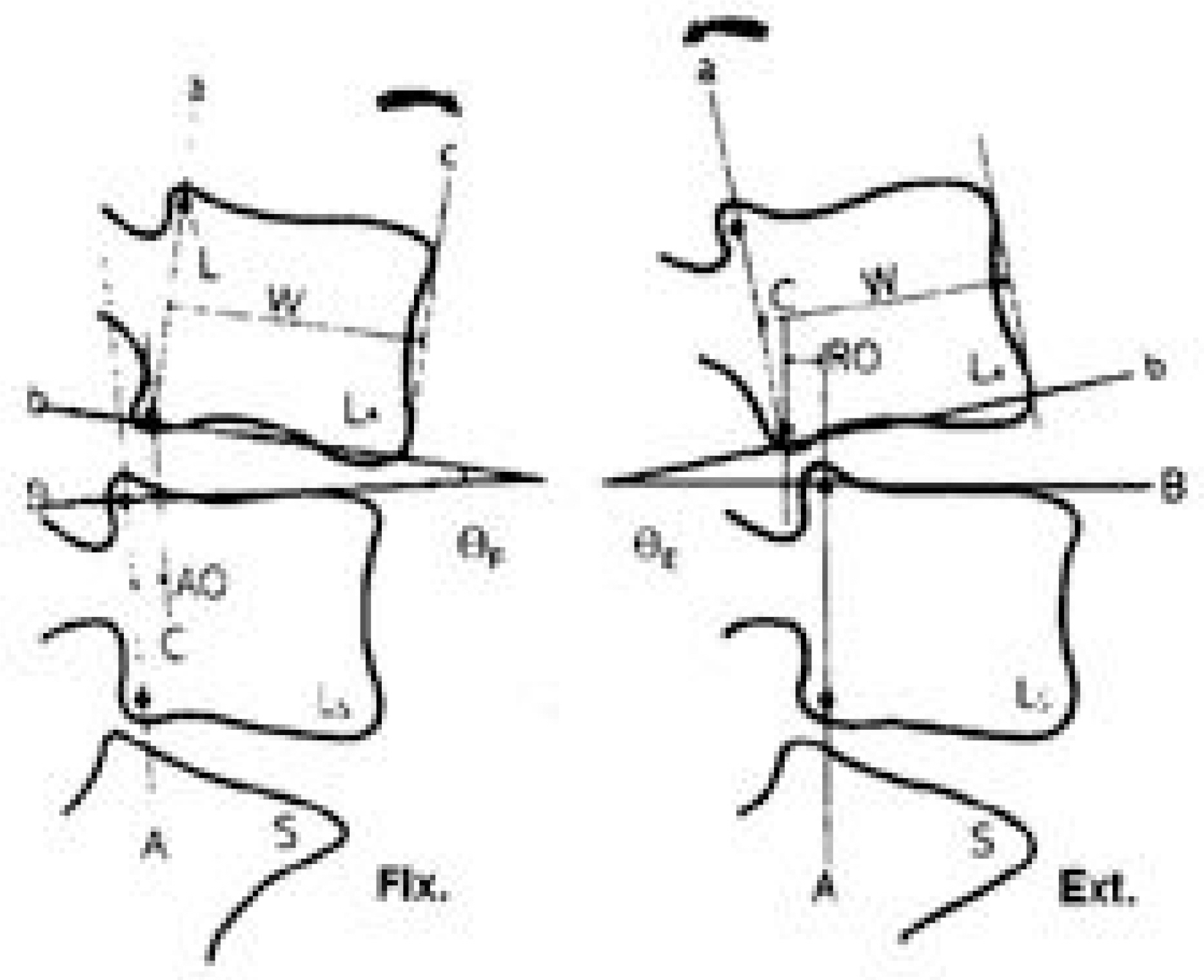
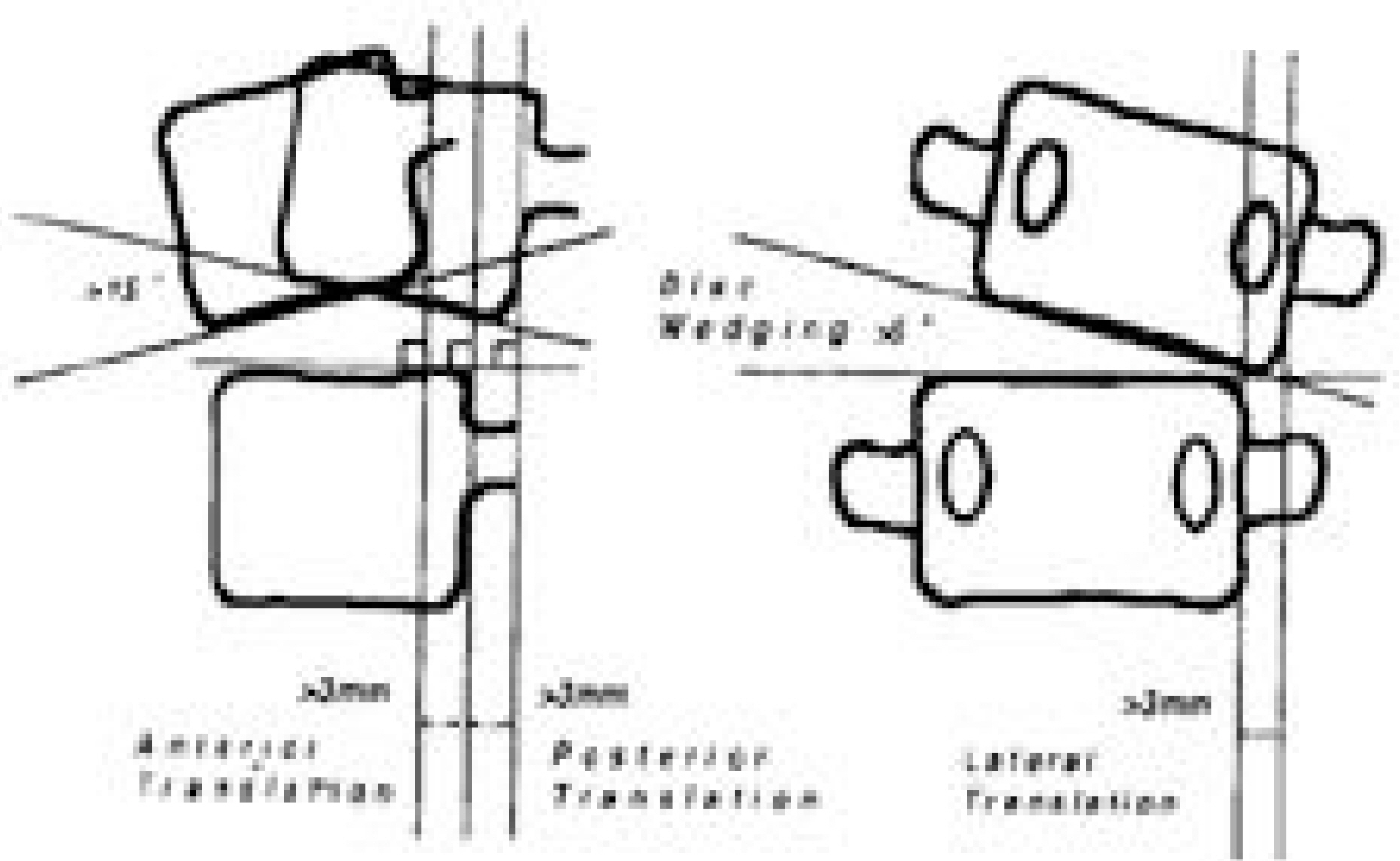
We reviewed 16 surgical cases of degenerative lumbar spinal disorders from July 1996 to February 2000 with an average follow-up of 41 months. Fusion was done in patients without instability, pathology and narrowing of L5-S1. We measured the disc degeneration of adjacent segments in preoperative MRIs using the Modified Pearce classification. In spine AP, lateral and flexion-extension radiographs, we measured disc height, angular motion and instability changes and correlated these with disc degeneration.
RESULTS
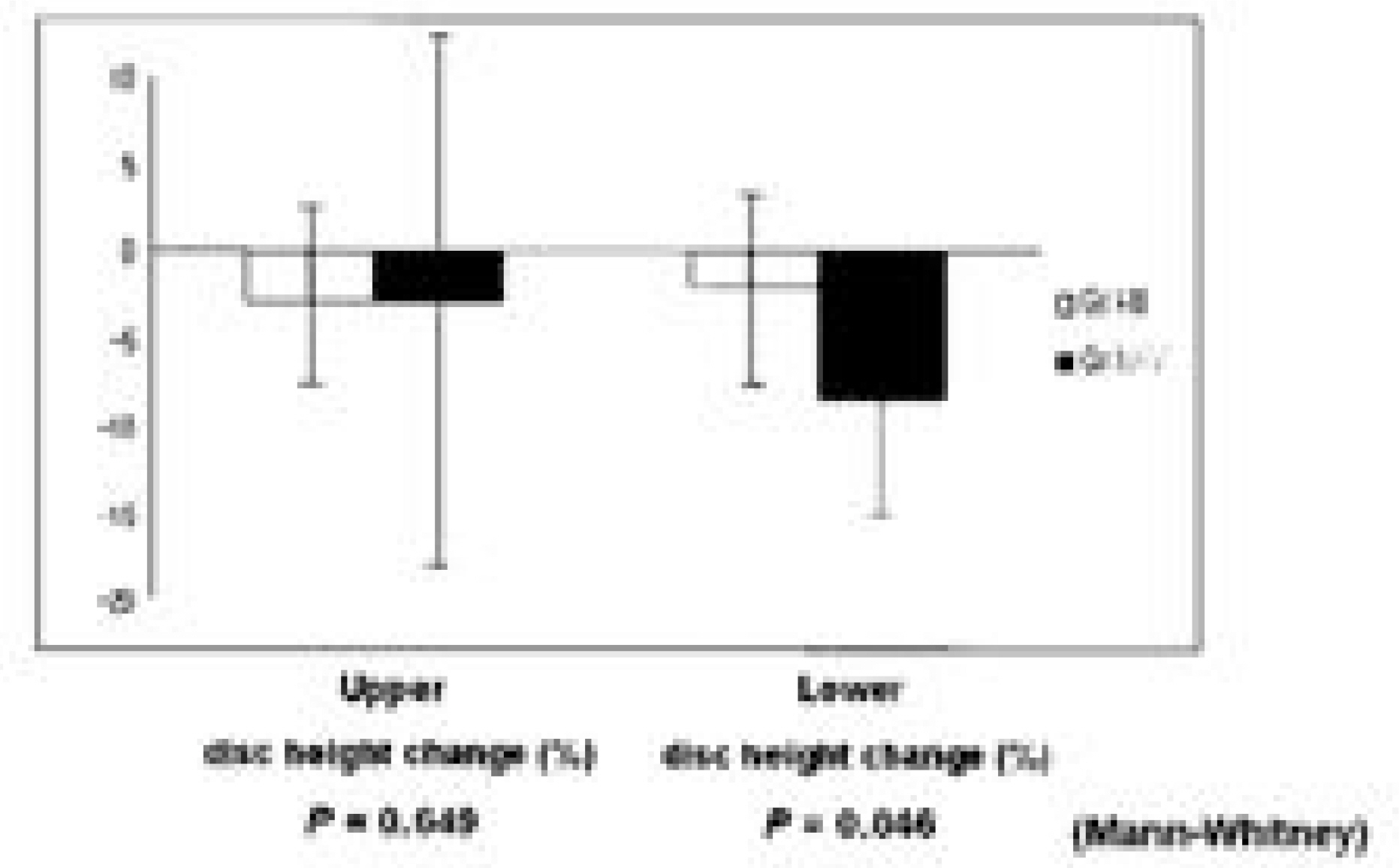
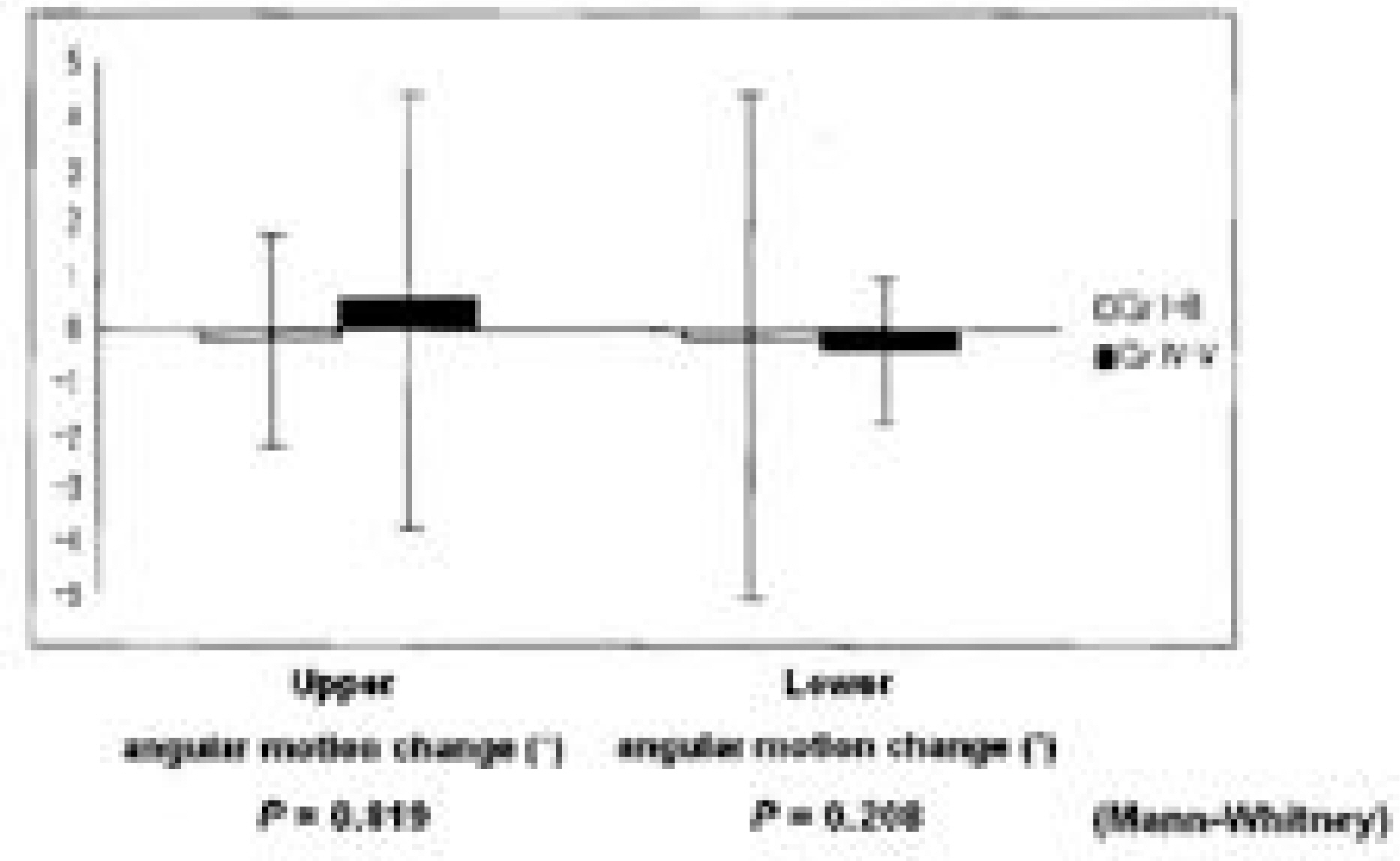
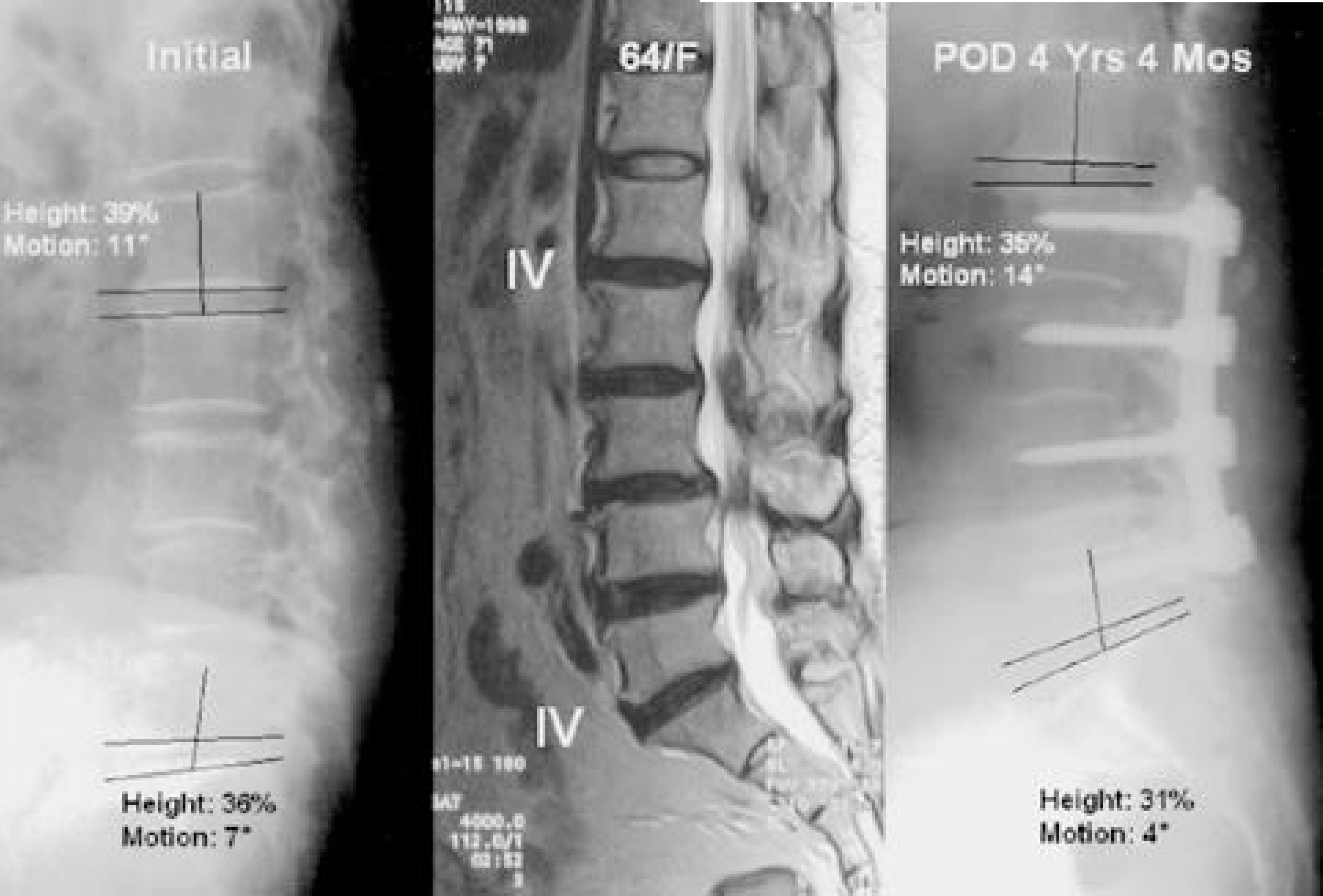
Disc height changes decreased in the upper and lower adjacent segments and preoperative disc degeneration above grade IV, decreased more in lower adjacent segment. A statistical correlation was found between disc degeneration and disc height changes in the lower segment (P=0.046), but not in the upper segment (P=0.649). The angular-motion was unchanged in the upper and lower adjacent segments, and no statistical correlation was found between disc degeneration and angular-motion changes (P=0.819, 0.208). Postoperative instability was found in the upper adjacent segment in 2 patients, but no statistical cor-relation was found between disc degeneration and instability (P=0.083, P=1.000).
CONCLUSION
L5-S1 might be saved when free of pathology, and when disc degeneration is below grade III and balanced sagit-tally. However, further study is needed because of the short-term follow up and low number of cases in this study.
MeSH Terms
Figure
Cited by 1 articles
-
Surgical Treatment of Osteoporotic Compression Fracture
Whoan Jeang Kim
J Korean Fract Soc. 2009;22(4):314-318. doi: 10.12671/jkfs.2009.22.4.314.
Reference
-
1). Aota Y, Kumano K and Hirabayashi S. P ostfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. Journal of spinal disorders. 8:464–473. 1995.2). Brodsky AE, Hendricks RL, Khalil MA, Darden BV and Brotzman TT. Segmental(“ Floating”) lumbar spine fusions. Spine. 14:447–450. 1989.
Article3). Cho KJ, Lee JY and Oh IS, et al. Change of segmental motion after lumbar posterolateral fusion. J of Korean Orthop Assoc. 34:281–287. 1999.
Article4). Cochran T, Irstam L and Nachemson A. Lon g-term anatomic and functional changes in patients with adoles - cent idiopathic scoliosis treated by Harrington rod fusion. Spine. 8:576–583. 1983.5). Dupuis PR, Yong-hing K, Cassidy JD and Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine. 10(3):262–276. 1985.
Article6). Friberg S and Hirsch C. Anatomical and clinical studies on lumbar disc degeneration. Acta Orthop Acand. 19:222–242. 1949.7). Frymoyer JW, Hanley EN, Howe J, Kuhlmann D and Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine. 4:435–440. 1979.
Article8). Horton WC, Holt RT and Muldowny DS. Controversy fusion of L5-S1 in adult scoliosis. Spine. 21:2520–2522. 1996.9). Kim HT, Park BH, Cheon DW, An HS and Lee HS. A comparative study of the floating(L4-5) vs lumbosacral (L4-S1) spinal fusions. J of Korean Orthop Assoc. 29:1151–1159. 1994.10). Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine. 12:97–104. 1987.
Article11). Moskowitz A, Moe JH, Winter RB, et al. Long-term follow-up of scoliosis fusion. J Bone Joint Surg. 62-A:364–376. 1980.
Article12). Pfirrmann CWA, Metzdorf A, Zanetti M, Hodler J and Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 26:1873–1878. 2001.
Article13). Quinnell RC and Stockdale HR. Some experimenatal observations of the influence of a single lumbar floating fusion on the remaining lumbar spine. Spine. 6:263–267. 1981.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accelerated L5-S1 Segment Degeneration after Spinal Fusion on and above L4-5 : Minimum 4-Year Follow-Up Results
- Surgical treatment of Degenerative Lumbar Spinal Disorders Using the Graf System: over three year results
- Survival Rates and Risk Factors for Cephalad and L5-S1 Adjacent Segment Degeneration after L5 Floating Lumbar Fusion : A Minimum 2-Year Follow-Up
- Adjacent Disc Stress Following Floating Lumbar Spine Fusion: A Finite Element Study
- Combined Instrumentation with the Soft and Rigid Stabilizer in Degenerative Lumbar Disorders