J Korean Soc Spine Surg.
2003 Mar;10(1):46-54. 10.4184/jkss.2003.10.1.46.
Osteoid Osteoma and Osteoblastoma of the Spine
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. bschang@medicine.snu.ac.kr
- KMID: 2209704
- DOI: http://doi.org/10.4184/jkss.2003.10.1.46
Abstract
- STUDY DESIGN: A retrospective study
OBJECTIVE
To analyze the clinical and radiological findings, and the results of the surgical treatment of osteoid osteomas and osteoblastomas of the spine. SUMMARY OF LITERATURE REVIEW: With the development of new imaging techniques, earlier diagnoses have been reported. However, a few reports of unexpected misdiagnosis, and postoperative results, have also been published.
MATERIALS AND METHODS
Between January 1980 and September 2002, twelve patients were diagnosed with an osteoid osteoma or osteoblastoma of the spine, and were surgically treated. The average preoperative symptom-duration and follow-up period were 20 and 33 months, with ranges from 6weeks to 96 months, and 4 to 120 months, respectively. All the patients were younger than 30 years old, with the majority being of growing age, and underwent at least a bone scan, CT or MRI, as part of the diagnostic procedures.
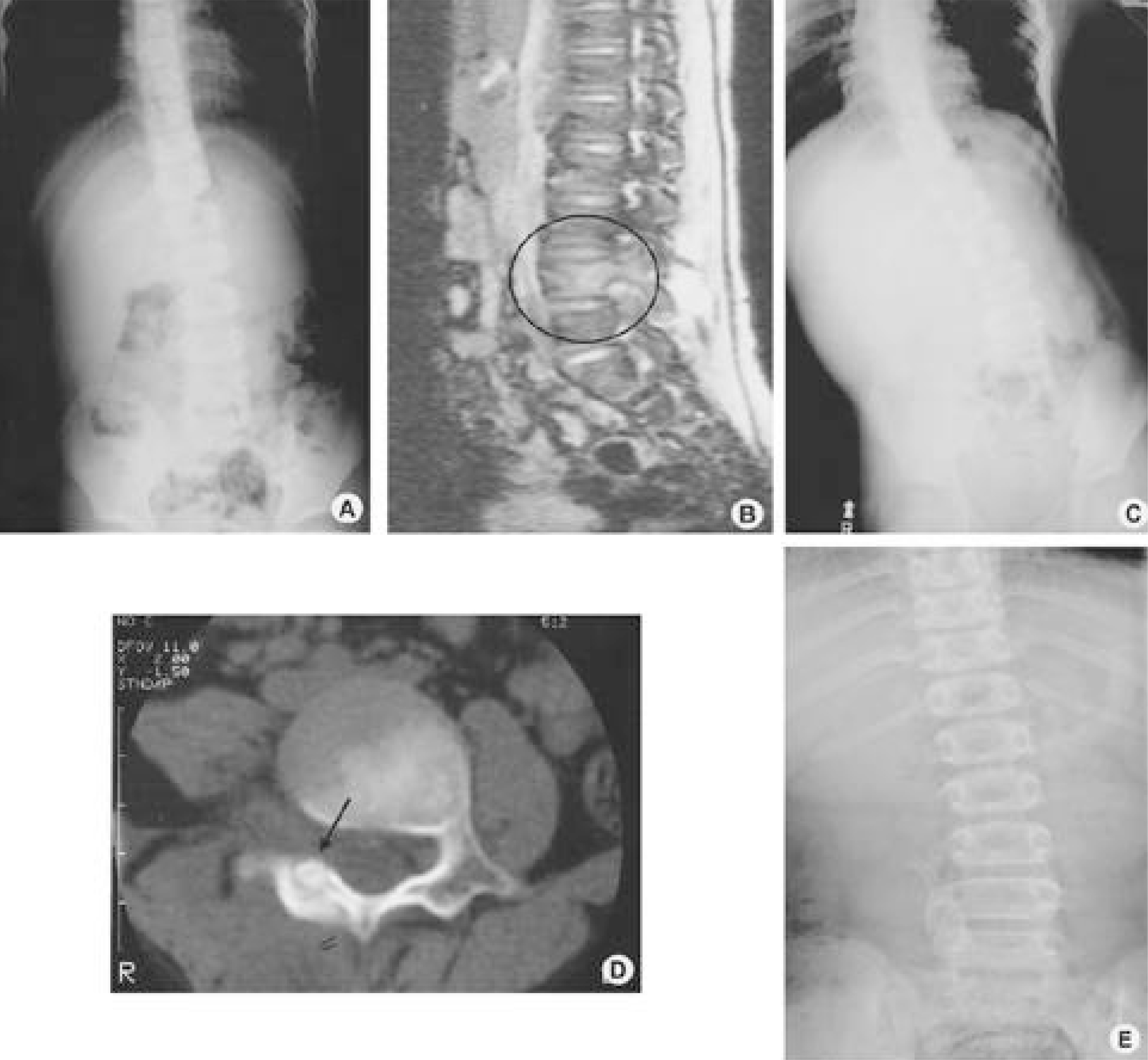
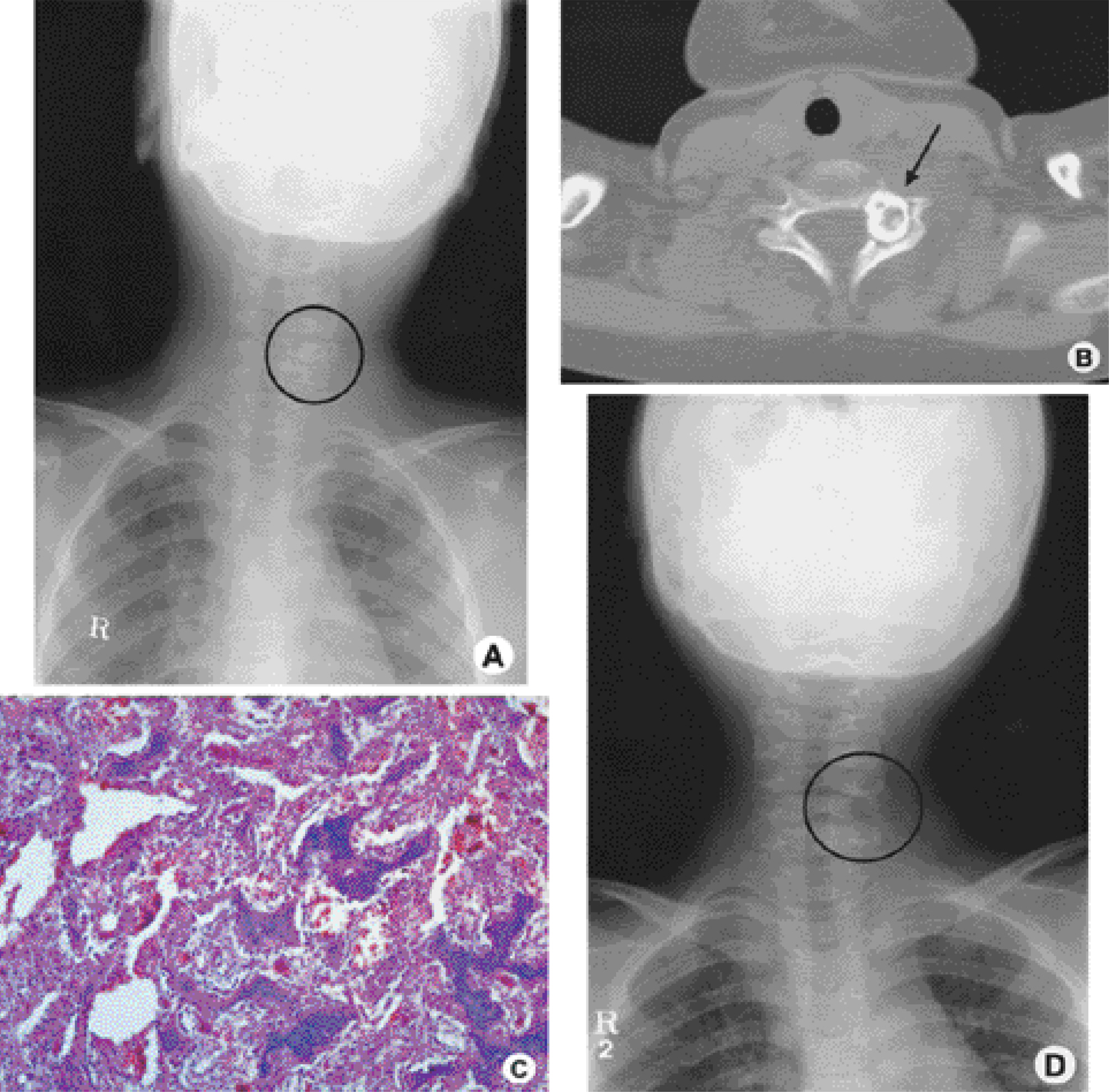
RESULTS
The most common symptom was pain at the lesion, with 2 torticollis and 4 scoliosis observed as combined spine deformities, respectively. Neurological abnormalities were seen more often in the osteoblastomas (80%) than in the osteoid osteomas (43%). From the radiological findings, a CT scan was a more effective procedure than any of the other diagnostic modalities in differentiating an osteosclerotic bony lesion and a nidus. In three out of the five MRI, 2 cases were misdiagnosed as infections and the other as a malignant tumor, with no significant abnormal findings in the simple roentgenogram. A wide excision was performed in all patients, and a fusion, with a bone graft, was also performed in 8. There were no postoperative spinal instabilities or complications.
CONCLUSION
In a differential diagnosis, careful history taking for pain, and a physical examination for spine deformity, are required. Without any clinical information, these tumors can be misdiagnosed as malignant tumors, or other infectious diseases, in a MRI. With regard to the surgical treatment, there were no cases of recurrence reported due to the wide excision, but a fusion, both with or without instrumentation, can be considered to prevent postoperative spine instability.
Keyword
MeSH Terms
Figure
Reference
-
1). Boriani S., Capanna R., Donati D, et al. Osteoblastoma of the spine. Clin Orthop,. 278:37–45. 1992.
Article2). Green R., Saifuddin A., Cannon S. Pictorial review: Imaging of primary osteosarcoma of the spine. Clin Radi -ol,. 51:325–329. 1996.
Article3). Jackson RP., Reckling FW., Mants FA. Osteoi d osteoma and osteoblastoma: Similar histologic lesions with different natural histories. Clin Orthop,. 128:303–313. 1997.4). Janin Y., Epstein JA., Carras R., Khan A. Osteoi d osteomas and osteoblastomas of the spine. Neurosurgery,. 8:31–38. 1981.5). Kawaguchi Y., Hasegawa T., Oka S., Sato C., Arima N., Norimatsu H. Mechanism of intramedullary high instensity area on T2-weighted magnetic resonance imaging in osteoid osteoma: a possible role of COX-2 expression. Pathol Int, Dec;. 51:933–937. 2001.6). Lefton DR., Torrisi JM., Haller JO. Vertebral osteoid osteoma masquerading as a malignant bone of soft-tissue tumor on MRI. Pediatr Radiol, Feb;. 31:72–75. 2001.7). Marsh BW., Bonfiglio M., Brady LP., Enneking WF. Benign osteoblastoma: Range of manifestations. J Bone Joint Surg,. 57A:1–9. 1995.8). McLeod RA., Dahlin DC., Beabout JW. The spec -trum of osteoblastoma. AM J Roentgenol,. 126:321–325. 1976.9). Nemoto O., Moser RP Jr., Van Dam BE., Aoki J., Gilkey FW. Osteoblastoma of the spine: A review of 75 cases. Spine,. 15:1272–1280. 1990.10). Ozaki T., Liljenqvist U., Hillmann A, et al. Os t eo i d Osteoma and Osteoblastoma of the Spine: Experiences with 22 Patients. Clin Orthop,. 397:394–402. 2002.11). Pettine KA., Klassen RA. Osteiod-osteoma and osteoblastoma of the spine. J Bone Joint Surg,. 68A:354–361. 1986.12). Ransford AO., Pozo JL., Hutton PA., Kirwan EO. The behaviour pattern of the scoliosis associated with osteoid osteoma or osteoblastoma of the spine. J Bone Joint Surg,. 66B:16–20. 1984.
Article13). Rosenthal DI., Hornicek FJ., Wolfe MW, et al. Percuta -neous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg,. 80A:815–821. 1998.14). Saifuddin A., Sherazi Z., Shaikh MI, et al. S p i n a l osteoblastoma: Relationship between paravertebral mus -cle abnormalities and scoliosis. Skeletal Radiol,. 25:531–535. 1996.15). Saifuddin A., White J., Sherazi Z, et al. Osteoid osteoma and osteoblastoma of the spine: Factors associated with the presence of scoliosis. Spine,. 23:47–53. 1998.16). Schlman L., Dorfman HD. Nerve Fibers in Osteoid Osteoma. J Bone and Joint Surg,. 52-A:1351–1356. 1970.17). Unni KK. Dahlin's Bone Tumors. General Aspects and Data on 11,087 Cases. Benign Osteoblastoma. Ed5. Philadelphia Lippincott-Raven: p. 131–142. 1996.18). Wold LE., Pritchard DJ., Bergert J, et al. Prostaglandin synthesis by Osteoid Osteoma and Osteoblastoma. Mod Pathol,. 1:129–131. 1998.19). Zanetti M., Eberhard SM., Exner GU., von Hochstetter A., Hodler J. Magnetic Resonance Tomography in osteoid osteoma: More confusion than benefit? Schweiz Rundsch Med Prax;Mar11: 86:p. 432–436. 1997.