J Korean Soc Spine Surg.
2003 Sep;10(3):269-276. 10.4184/jkss.2003.10.3.269.
Changes of Adjacent Segment in Anterior Cervical Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University, Wonju College of Medicine, Wonju, Korea. par73@wonju.yonsei.ac.kr
- KMID: 2209696
- DOI: http://doi.org/10.4184/jkss.2003.10.3.269
Abstract
- STUDY DESIGN: A retrospective radiographic and medical record analysis of 36 patients.
OBJECTIVES
To describe the incidence and consequence of the distribution of sagittal plane motion, across the adjacent cervical motion segment, after cervical fusion. Furthermore, to find the cause of the progression of degenerative changes in intervertebral discs adjacent to the fused segment. SUMMARY OF LITERATURE REVIEW : Anterior cervical fusion has been widely used in the treatment of degenerative cervical spine. An increased incidence of degenerative disease may exist at the levels immediately adjacent to a cervical fusion. However, the frequency of these complications is probably overestimated, and their effect on clinical outcome remains unknown.
MATERIALS AND METHODS
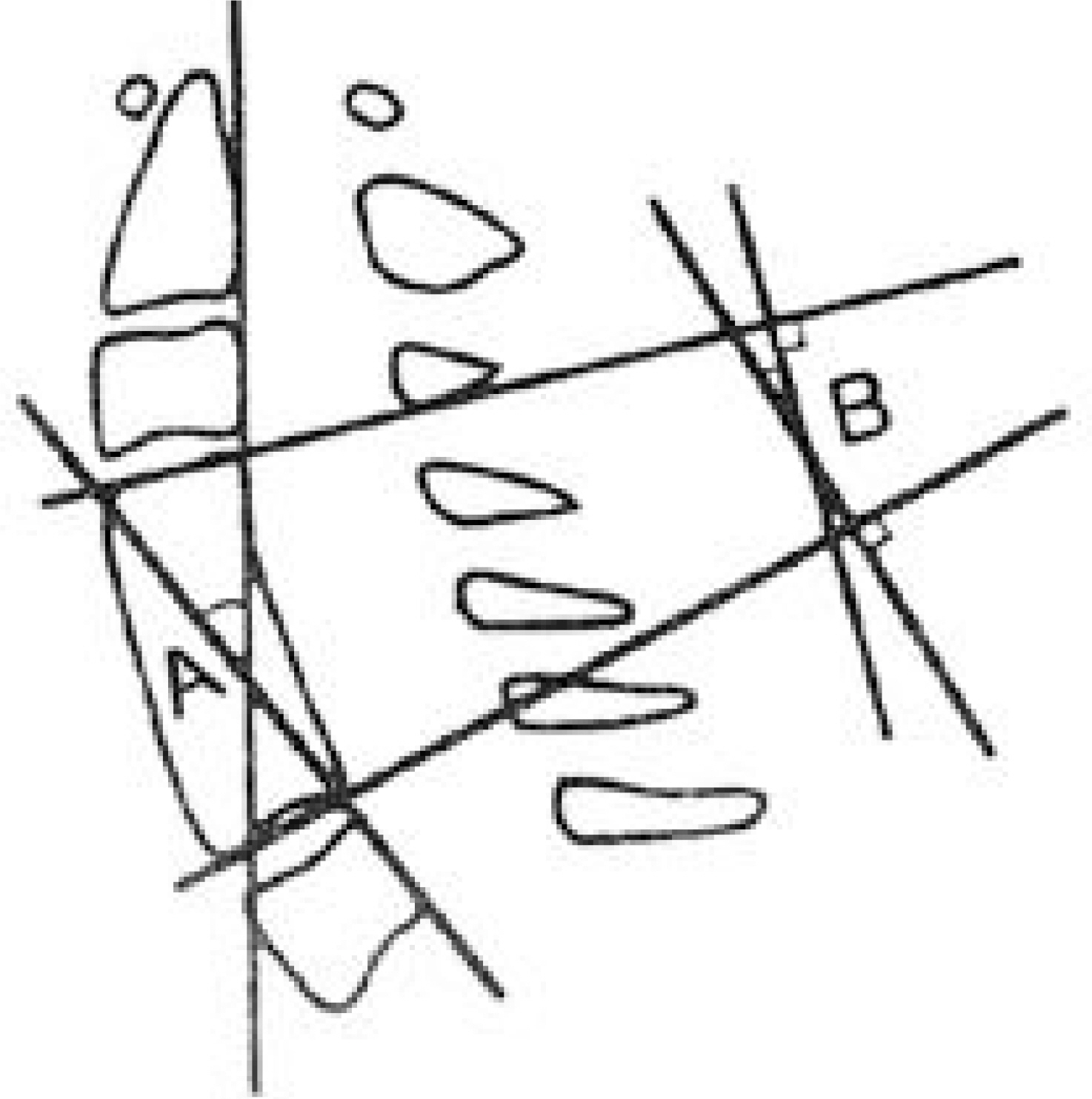
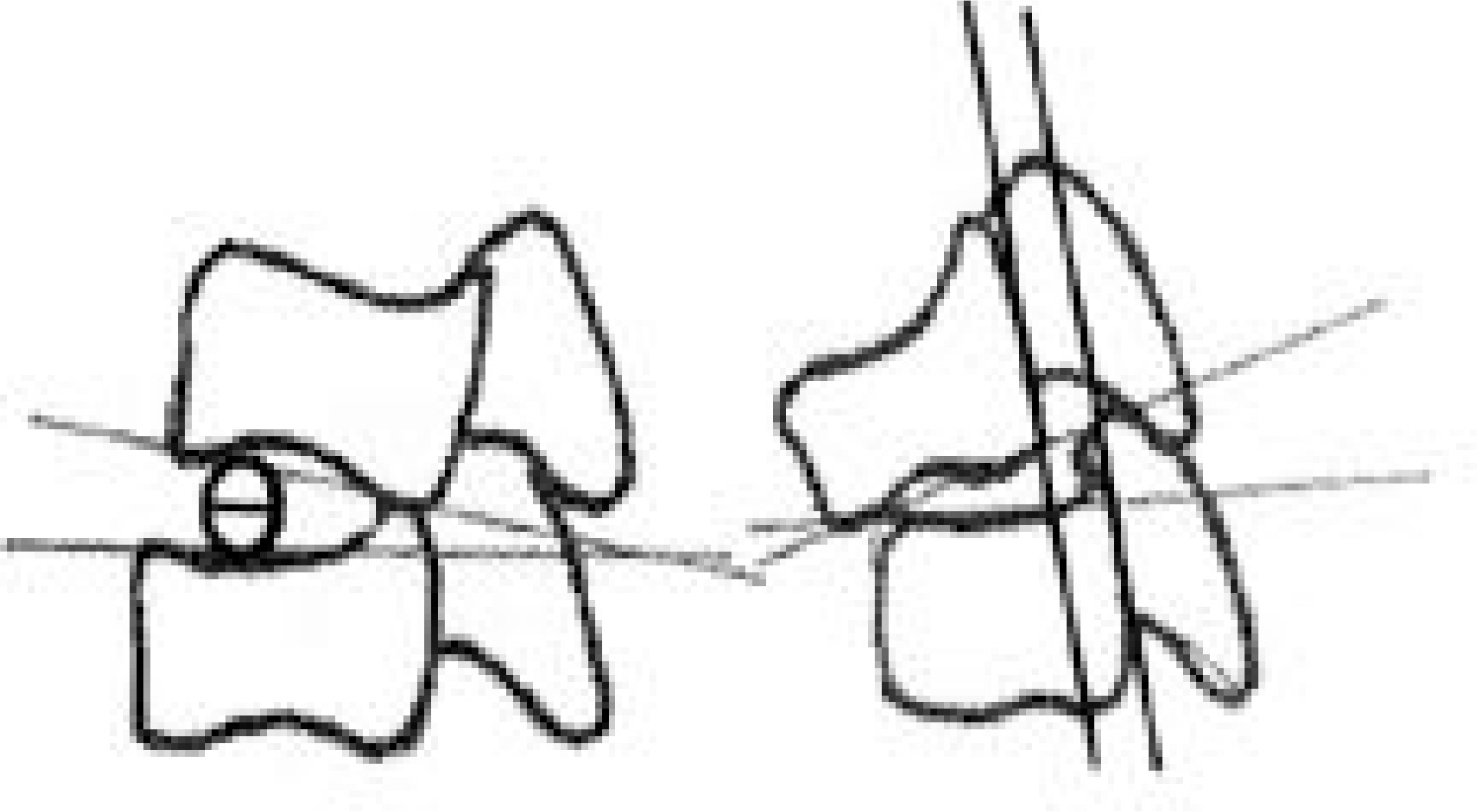
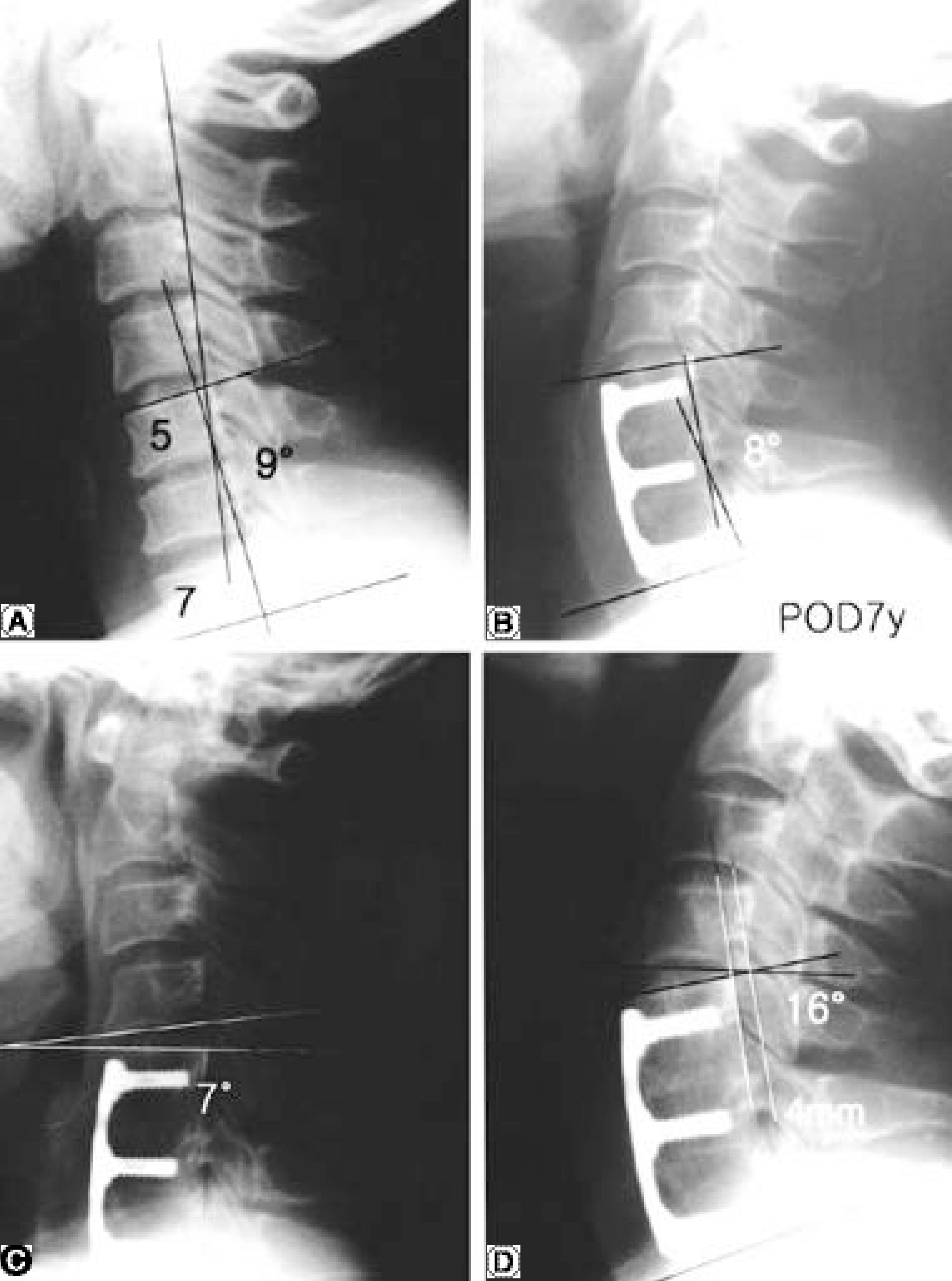
From 1990 to 1996, 36 patients who underwent anterior cervical spine fusion for degenerative disorders were reviewed retrospectively with an average follow up of 6.9 years. Lateral views in neutral position, in flexion, and in extension of the preoperative cervical roentgenograms were analyzed in comparison with the last follow-up films in the range of motion of the neck, and in the intervertebral angular mobility and anteroposterior displacement of the vertebral bodies, and finally to quantify the incidence of the spinal instability.
RESULTS
Degenerative change in adjacent intervertebral level was observed in 16 of the 36 patients (44.4%), above the fusion in 10, below the fusion in 4, and both above and below the fusion in 2 cases. In addition, degenerative change in adjacent intervertebral level was observed in 68% of cases of loss of lordosis of the fused segment, and degenerative change occurred more frequently in younger patients to a statistically significant extent.
CONCLUSIONS
Loss of lordosis of the fused segment and young age are two factors promoting degenerative changes in adjacent intervertebral levels after anterior cervical fusion.
MeSH Terms
Figure
Cited by 3 articles
-
Lower Cervical Spine Injury
Jae-Sung Ahn
J Korean Fract Soc. 2011;24(1):100-113. doi: 10.12671/jkfs.2011.24.1.100.Availability of Anterior Cervical Plating in Distractive Flexion Injury in Lower Cervical Spine - Radiologic Aspects -
Whoan Jeang Kim, Jong Won Kang, Jae Guk Park, Chang Hyun Baik, Kun Young Park, Joon Hyuk Ko, Won Sik Choy
J Korean Soc Spine Surg. 2006;13(3):163-169. doi: 10.7469/JKSS.2006.13.3.163.Prevalence And Risk Factor of Degenerative Disease of Adjacent Segment after Anterior Cervical Arthrodesis
Yung-Tae Kim, Dong-Hoon Baek, Choon-Sung Lee, Dong-Ho Lee, Changju Hwang, Dong-Wook Sohn
J Korean Soc Spine Surg. 2010;17(1):1-6. doi: 10.4184/JKSS.2010.17.1.1.
Reference
-
1). Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy: Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg. 1993; 75:1298–1307.
Article2). Braunstein EM, Hunter LY, Bailey RW. Long term radiographic changes following anterior cervical fusion. Clin Radiol. 1980; 31:201–203.
Article3). Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs: A review of one hundred forty-six patients. Spine. 1984; 9:667–671.4). Gregorius FK, Estrin T, Crandall PH. Cervical spondylotic radiculopathy and myelopathy. A long-term follow-up study. Arch Neurol. 1976; 33:618–625.5). Robinson RA, Walker AE, Ferlic DC, Wiecking DK. The results of anterior interbody fusion of the cervical spine. J Bone Joint Surg. 1962; 44:1569–1587.
Article6). Gore DR, Sepic SB. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine. 1993; 23:2047–2051.7). Shinomiya K, Okamoto A, Kamikozuru M, Furuya K, Yamaur al. An analysis of failures in primary cervical anterior spinal cord decompression and fusion. J Spinal Disord. 1993; 6:277–288.8). Wu W, Thuomas KA, Hedlund R, Leszniewski W, Vavruch L. Degenerative changes following anterior cervical disectomy and fusion evaluated by fast spin-echo MR imaging. Acta Radiol. 1996; 37:611–617.9). Yonenobu K, Okada K, Fuii T, Fujiwara K. Yamashita K, Ono K. Causes of neurologic deterioration following surgical treatment of cervical myelopathy. Spine. 1996; 11:818–823.
Article10). Goto S, Mochizuki M, Kita T, et al. Anterior surgery in four consecutive technical phases for cervical spondylotic myelopathy. Spine. 1993; 18:1986–1973.
Article11). Dvorak J, Froehlich D, Penning L. Baumgarner H, Panabi MM. Functional radiographic diagnosis of the cervical spine: Flexion/Extension. Spine. 1988; 13:1748–1755.
Article12). Cloward RB. The anterior approach for removal of ruptured cervical disc. J Neurosurg. 1958; 15:602–617.13). Dohler JR, Kahn MR, Hughes SP. Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Acta Orthop trauma Surg. 1985; 104:247–250.14). Jackson RP, McMaus AC. Radiogrphic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size: a prospective controled clinical study. Spine. 1994; 19:1611–1618.15). Oda I, Cunningham BW, Buckley RA, et al. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments An in vivo animal model. Spine. 1999; 24:2139–2146.16). Katsuura A, Hukuda S, Saruhashi Y, Mori k. Kyphotic malalignment after anterior cervical fusion in one of the factors promoting the degenrative process in adjacent intervetabral levels. Eur Spine J. 2001; 10:320–324.17). Breig A, Turnbull I, Hassler O. Effects of mechanical stress on the spinal cord in cervical spondylosis. A study on fresh cadaver material. J Neurosurg. 1996; 25:45–563. 1996.18). Ahn JS, Lee JK, Yang JY, Lee HH. Change of the lordosis on cervical spine after anterior interbody fusion with antogenous iliac strut bone graft. J Kor Spine Surg. 2001; 8:468–474.19). Park HJ, Rha JH, Yoon YS. Anterior cervical interbody fusion using cervical locking plate(CSLP). J Kor Orthop Assoc. 1996; 31:52–57.20). Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT. A kinematic study after cervical spine before and after segmental arthrodesis. Spine. 1998; 23:1649–1656.21). Panjabi MM. The stabilizing system of the spine. Part II, Neutral zone and instability hypothesis. J Spinal Disord. 1992; 5:390–7.
Article22). Baba H, Furusawa N, Lmura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopa -thy. Spine. 1993; 18:2167–2173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparing adjacent segment biomechanics between anterior and posterior cervical fusion using patient-specific finite element modeling
- Degenerative Changes of Adjacent Segment Following Cervical Anterior fusion: Correlation with Preoperative MRI Findings of Adjacent Disc
- Comparison of Adjacent Segment Degeneration, Cervical Alignment, and Clinical Outcomes after One- and Multilevel Anterior Cervical Discectomy and Fusion
- Prevalence And Risk Factor of Degenerative Disease of Adjacent Segment after Anterior Cervical Arthrodesis
- Recycling of Cervical Artificial Disc for the Symptomatic Adjacent Segment Disorder Combined with Instability on Total Disc Replacement Area: A Case Report