J Korean Soc Spine Surg.
2009 Jun;16(2):71-78. 10.4184/jkss.2009.16.2.71.
Efficiency of Anterior Interbody Fusion using Cage and Plate in the Distractive Flexion Injury of Cervical Spine : Cage vs Tricortical Autoiliac Bone
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University, Wonju College of Medicine, Wonju, Korea. par73@yonsei.ac.kr
- KMID: 2209600
- DOI: http://doi.org/10.4184/jkss.2009.16.2.71
Abstract
-
STUDY DESIGN: This is a retrospective study
OBJECTIVES
We wanted to evaluate the effectiveness and safety of anterior interbody fusion (AIF) using cage and plate fixation for treating distractive flexion injury of the cervical spine according to the radiological and clinical outcomes. SUMMARY OF THE LITERATURE REVIEW: AIF of the cervical spine using autoiliac bone and plate fixation is known as an effective method for treating not only degenerative disease, but also trauma as well. However, the problem lies in the complications that occur at the donor site. To avoid these complications, the fusion method using a cage is becoming more frequently used, but there are not many reports on using a cage and plate for treating trauma in the cervical spine.
MATERIALS AND METHODS
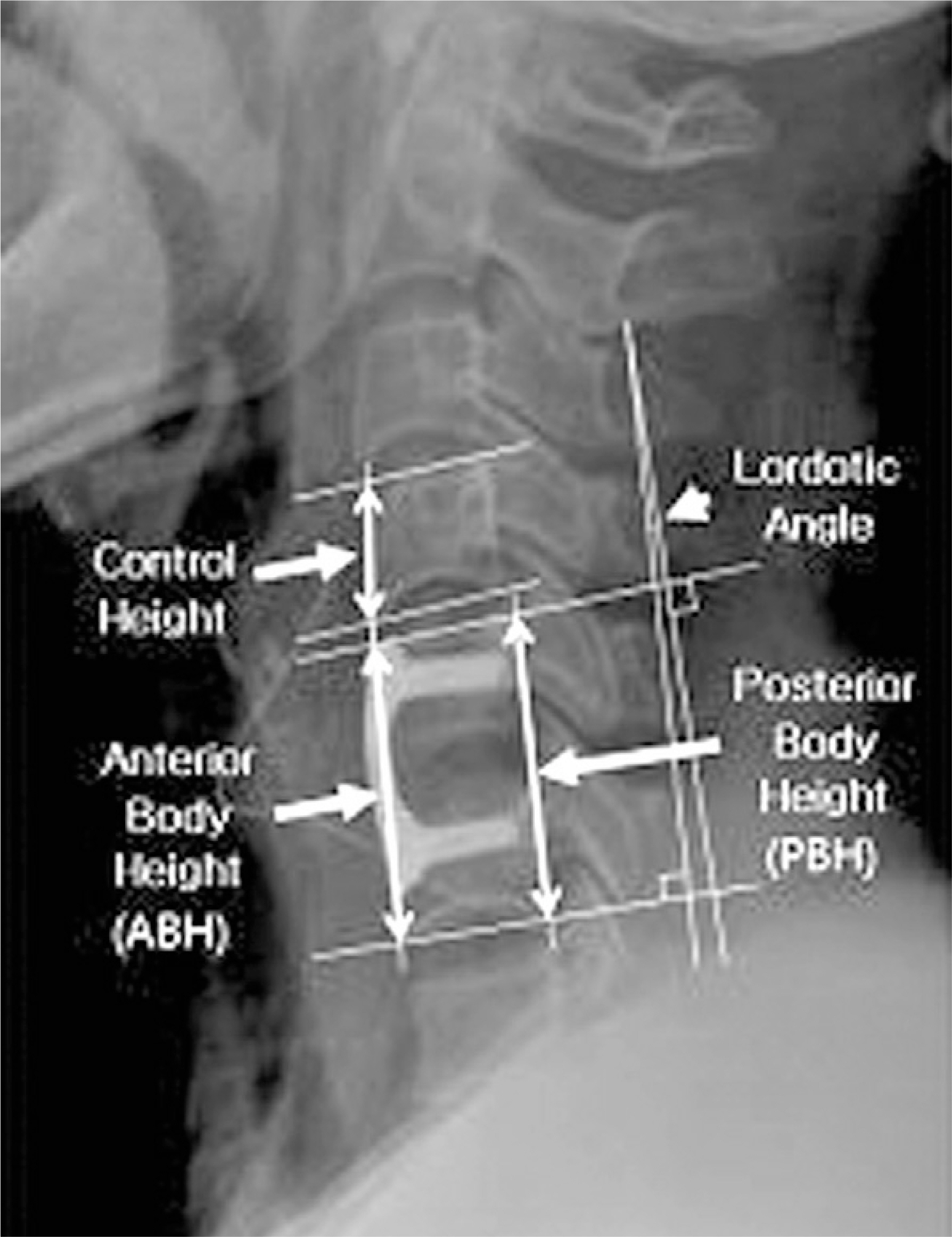
We retrospectively analyzed 47 patients with distractive flexion injury of the cervical spine and who underwent anterior decompression and interbody fusion with a autoiliac bone graft and plate fixation (Group I, 32 patients) or who underwent anterior decompression and interbody fusion with cage and plate fixation (Group II, 15 patients). We statistically analyzed the changes of the segmental lordosis, the fused segmental body height, the fusion rate on plain radiography and the neurologic recovery with using an ASIA scoring system.
RESULTS
All the cases were fused by 12.6+/-2.5weeks after operation. The changes of segmental lordosis shows no statistical difference between the two groups (p=0.69). The anterior and posterior vertebral heights of the fused segments of Group I were more decreased than those of Group II, and there was a statistical difference between the two groups (p=0.03, 0.04). The initial and last follow up neurologic statuses were not statistically difference between the two groups (p=0.11)
CONCLUSIONS
For the treatment of fracture-dislocation injury in the cervical spine, AIF using a PEEK cage filled with autoiliac bone and plate fixation is an effective method with the least possibility of complications at the donor site, and at the same time, this surgical method shows equally satisfactory results, both radiologically and clinically, as fusion with using a tricortical autoiliac bone graft.
MeSH Terms
Figure
Reference
-
1). Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982; 7(1):1–27.
Article2). Song KJ, Lee KB, Kim SR. Availability of anterior cervical plating according to the severity of injury in distractive flexion injury in lower cervical spine. J Korean Orthop Assoc. 2005; 40:195–202.
Article3). Park HJ, Shim YJ. Treatment of distractive flexion injury in lower cervical spine using anterior cervical fusion. J Korean Soc Spine Surg. 2007; 14:221–228.
Article4). Cybulsky GR, Douglas RA, Meyer PR Jr, et al. Complications in three column cervical spine injuries requiring anterior-posterior stabilization. Spine. 1992; 17:253–256.5). Henriques T, Olerud C, Bergman A, Jonsson H Jr. Distractive flexion injuries of the subaxial cervical spine treat with anterior plate alone. J Spinal Disord Tech. 2004; 17:1–7.6). Ulrich C, Worsdorfer O, Claes L, Magerl F. Comparative study of the stability of anterior and posterior cervical spine fixation procedures. Arch Orthp Trauma Surg. 1987; 106:226–231.
Article7). Robinson R, Smith G. Anterlateral cervical disc removal and interbody fusion for cervical disc herniation. Bull Johns Hopkins Hosp. 1955; 96:223–224.8). Cloward R. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958; 15:602–617.9). Wilson DH, Campbell DD. Anterior cervical discectomy without bone graft. Report 71 cases. J Neurosurg. 1977; 47:551–555.10). Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003; 28:134–139.
Article11). Arringon ED, Smith VJ, Chambers HG, et al. Complication of iliac crest bone graft harvesting. Clin Orthop. 1996; 329:300–309.12). Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004; 62:378–385. discussion 385-386.
Article13). Rawlinson JN. Morbidity after anterior cervical decompression and fusion: The influence of the donor site on recovery, and the results of a trial of Surgibone compared to autologous bone. Acta Neurochir. 1994; 131:106–118.
Article14). Summer BN, Eisenstein SM. Donor site pain from the ilium. A complication of lumbar spine fusion. J Bone Joint Surg Br. 1998; 71:677–680.15). Malloy KM, Hilibrand AS. Autograft versus allograft in degenerative cervical disease. Clin Orthop Relat Res. 2002; 394:27–38.
Article16). Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine. 1991; 16:726–729.
Article17). Deutsch H, Haid R, Rodts G Jr, Mummaneni PV. The dicision-making process: allograft versus autograft. Neurosurgery. 2007; 60:98–102.18). Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopaedics. 1988; 11:931–944.
Article19). Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine. 1993; 18:2106–2107.20). Kuslich SD, Ulstrom CL, Griffith SL, Ahern JW, Dow-dle JD. The Bagby and Kuslich method of lumbar interbody fusion. History, techniques, and 2-year followup results of a United States prospective, multicenter trial. Spine. 1998; 23:1267–1279.21). Ray CD. Threaded titanium cages for lumbar interbody fusion. Spine. 1997; 22:667–679.22). Yu-Cheng Chou, Der-Cherng Chen, Wanhua Annie Hsieh, et al. Efficacy of anterior cervical fusion: Comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci. 2008; 15:1240–1245.23). Park HJ, Shim YJ, Yang JH. Anterior decompression and fusion in the treatment of single-level cervical disc herniation: Plate vs Cage. J Korean Soc Spine Surg. 2008; 15:140–148.24). Cho DY, Liau WR, Lee WY, et al. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002; 51:1343–1349. discussion 1349-1350.
Article25). Erich Kast, Sharam Derakhshani, Matthias Bothmann, Joachim Oberle. Subsidence after anterior cervical interbody fusion: A randomized prospective clinical trial. Neurosurg Rev. 2008.26). Kemmesies D, Meier U. Experience with five different intervertebral disc spacers for cervical spondylodesis. Zentralbl Neurochir. 2005; 66:24–33.
Article27). G. Matge. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir. 2002; 144:539–550.28). Kettler A, Wilke HJ, Claes L. Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg. 2001; 94:97–107.
Article29). Demircan MN, Kutlay AM, Colak A, et al. Multilevel cervical fusion without plates, screws or autogenous iliac crest bone graft. J Clin Neurosci. 2007; 14:723–728.
Article30). Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007; 2:205–209.
Article31). Delepine F, Jund S, Schlatterer B, de Peretti F. Experience with poly ether ether ketone (PEEK) cages and locking plate for anterior cervical fusion in the treatment of spine trauma without cord injury. Rev Chir Orthop Reparatrice Appar Mot. 2007; 93:789–797.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficiency of Anterior Interbody Fusion using Cage Packed with DBM in the Distractive Flexion Injury of Cervical Spine: Demineralized Bone Matrix vs Autoiliac Cancellous Bone
- Anterior Decompression and Fusion in the Treatment of Single-level Cervical Disc Herniation: Plate Fixation vs Cage
- Anterior Cervical Interbody Fusion Using a Plate Cage System in Degenerative Cervical Disease
- Functional Outcomes of Subaxial Spine Injuries Managed With 2-Level Anterior Cervical Corpectomy and Fusion: A Prospective Study
- Anterior Cervical Fusion with the PCB Instrumentation (Cervical Plate Cage System) in Degenerative Cervical Disease