J Korean Soc Transplant.
2016 Mar;30(1):6-12. 10.4285/jkstn.2016.30.1.6.
Single Center Experience of Biliary Reconstruction in Living Donor Liver Transplantation: Duct-to-Duct Anastomosis
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. choi5491@yuhs.ac
- KMID: 2202622
- DOI: http://doi.org/10.4285/jkstn.2016.30.1.6
Abstract
- BACKGROUND
Duct-to-duct anastomosis is the most common biliary reconstruction method in living donor liver transplantation. However, biliary complications can frequently occur. The objective of this study was to examine biliary complications and related risk factors of patients with living donor liver transplantation during the last 12 years in our institution.
METHODS
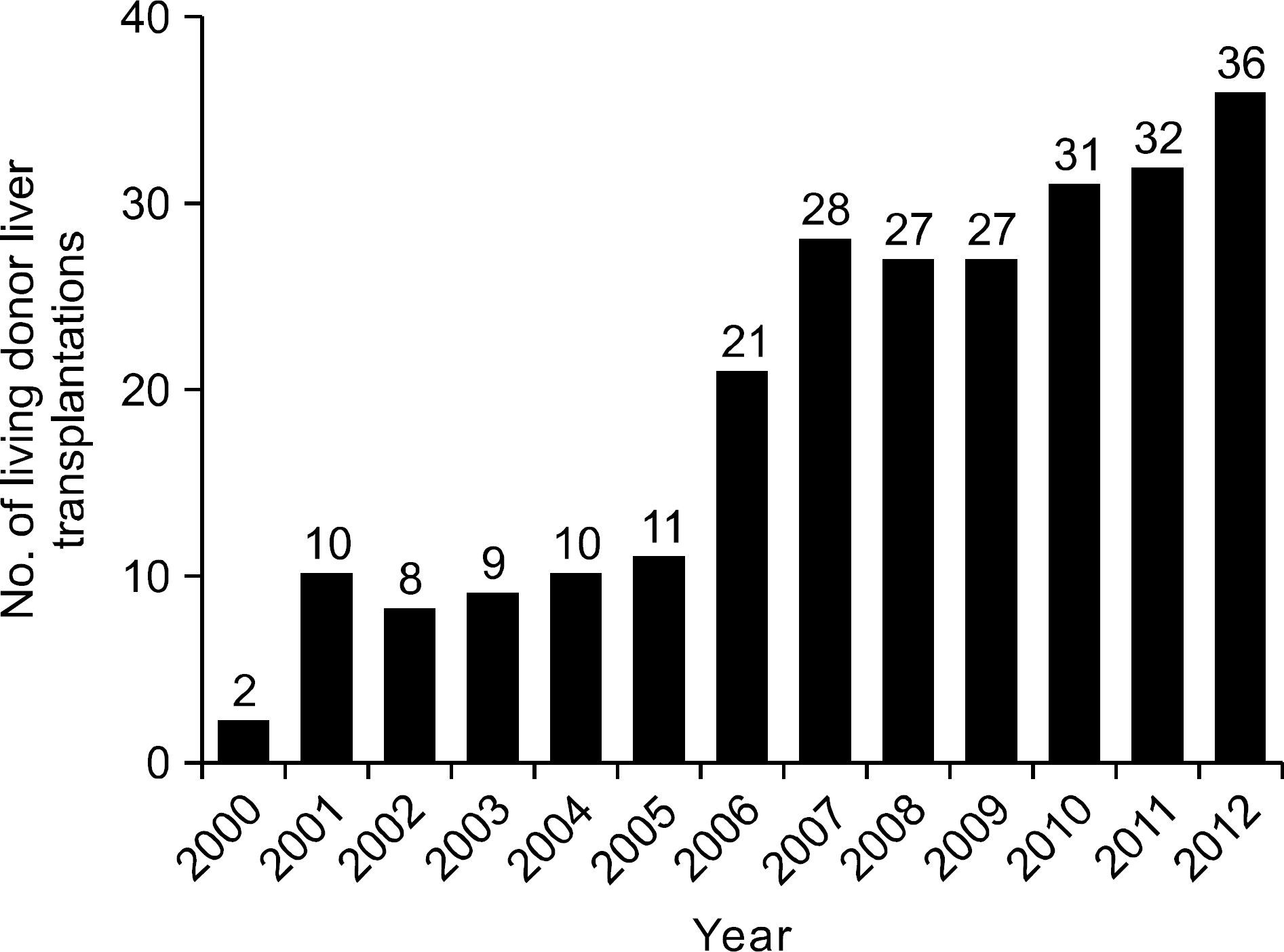
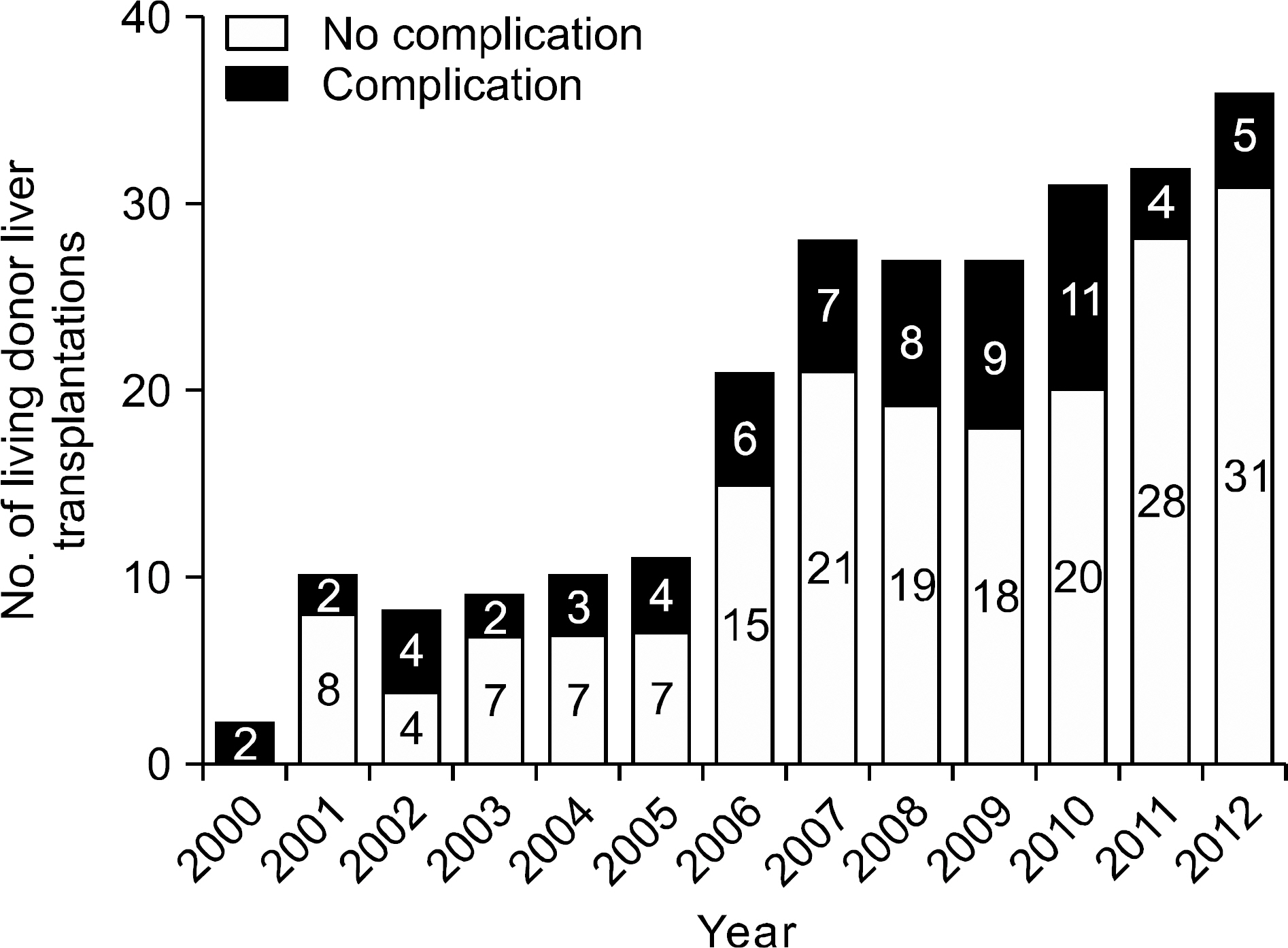
Surgical outcomes of 252 consecutive patients with duct-to-duct anastomosis for biliary reconstruction in living donor liver transplantation between December 2000 and July 2012 were analyzed retrospectively.
RESULTS
Among the 252 patients, there were 65 cases (25.8%) of biliary complications. Before 2010, the incidence of biliary complications was 30.4% (56 of 184 cases). After 2011, the incidence was significantly (P<0.05) decreased to 13.2% (nine out of 68 cases). The complication rate of anastomosis of two separated bile ducts of graft to recipient two separated bile ducts using cystic duct and common bile duct of recipient was 50% (10 out of 20), which was relatively higher compared to that of single to single duct anastomosis (47 out of 191, 24.6%) or multiple duct to single duct anastomosis (eight out of 41, 19.5%).
CONCLUSIONS
Duct to duct anastomosis between two separated bile ducts of a graft to two separated bile ducts of a recipient, the most common biliary reconstruction method, was associated with higher rate of biliary complications. Complications related to biliary reconstruction of living donor liver transplantation was gradually decreased. Standardization of bile duct anastomosis might lead to sequential reduction of biliary complications in living donor liver transplantations.
MeSH Terms
Figure
Reference
-
1). Murray KF., Carithers RL Jr: AASLD. AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology. 2005. 41:1407–32.
Article2). Vitale A., Morales RR., Zanus G., Farinati F., Burra P., Angeli P, et al. Barcelona Clinic Liver Cancer staging and transplant survival benefit for patients with hepatocellular carcinoma: a multicentre, cohort study. Lancet Oncol. 2011. 12:654–62.
Article3). de Villa VH., Lo CM., Chen CL. Ethics and rationale of living-donor liver transplantation in Asia. Transplantation. 2003. 75(3 Suppl):S2–5.
Article4). Kaido T., Uemoto S. Does living donation have advantages over deceased donation in liver transplantation? J Gastroenterol Hepatol. 2010. 25:1598–603.
Article5). Wan P., Yu X., Xia Q. Operative outcomes of adult living donor liver transplantation and deceased donor liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2014. 20:425–36.
Article6). Wachs ME., Bak TE., Karrer FM., Everson GT., Shrestha R., Trouillot TE, et al. Adult living donor liver transplantation using a right hepatic lobe. Transplantation. 1998. 66:1313–6.
Article7). Akamatsu N., Sugawara Y., Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 2011. 24:379–92.
Article8). Duailibi DF., Ribeiro MA Jr. Biliary complications following deceased and living donor liver transplantation: a review. Transplant Proc. 2010. 42:517–20.
Article9). Zimmerman MA., Baker T., Goodrich NP., Freise C., Hong JC., Kumer S, et al. Development, management, and resolution of biliary complications after living and deceased donor liver transplantation: a report from the adult-to-adult living donor liver transplantation cohort study consortium. Liver Transpl. 2013. 19:259–67.
Article10). Wilson BJ., Marsh JW., Makowka L., Stieber AC., Koneru B., Todo S, et al. Biliary tract complications in orthotopic adult liver transplantation. Am J Surg. 1989. 158:68–70.
Article11). Soejima Y., Taketomi A., Yoshizumi T., Uchiyama H., Harada N., Ijichi H, et al. Biliary strictures in living donor liver transplantation: incidence, management, and technical evolution. Liver Transpl. 2006. 12:979–86.
Article12). Rouch DA., Emond JC., Thistlethwaite JR Jr., Mayes JT., Broelsch CE. Choledochocholedochostomy without a T tube or internal stent in transplantation of the liver. Surg Gynecol Obstet. 1990. 170:239–44.13). Ju MK., Choi GH., Joo DJ., Hur KH., Choi J., Kim MS, et al. Use of the hilar plate looping technique for bile duct dissection in living donor liver transplantation significantly reduces recipient biliary complications. Transplant Proc. 2010. 42:4161–3.
Article14). Simoes P., Kesar V., Ahmad J. Spectrum of biliary complications following live donor liver transplantation. World J Hepatol. 2015. 7:1856–65.
Article15). Lee SG. Current status of liver transplantation in Korea. Korean J Gastroenterol. 2005. 46:75–83. (이승규, 국내 간이식 의 현황과 전망. 대한소화기학회지 2005;46: 75-83.).16). Korean Network for Organ Sharing (KONOS). Statistics of organ transplantation [Internet]. Seoul: KONOS;c2014. [cited 2016 Mar 2]. Available from:. http://www.konos.go.kr.17). Yang Y., Yan LN., Zhao JC., Ma YK., Huang B., Li B, et al. Microsurgical reconstruction of hepatic artery in A-A LDLT: 124 consecutive cases without HAT. World J Gastroenterol. 2010. 16:2682–8.
Article18). Seehofer D., Eurich D., Veltzke-Schlieker W., Neuhaus P. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant. 2013. 13:253–65.
Article19). Sugawara Y., Makuuchi M. Living donor liver transplantation: present status and recent advances. Br Med Bull. 2005. 75-76:15–28.
Article20). Yazumi S., Chiba T. Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol. 2005. 40:861–5.
Article21). Hwang S., Lee SG., Sung KB., Park KM., Kim KH., Ahn CS, et al. Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver Transpl. 2006. 12:831–8.
Article22). Ayuso JR., Ayuso C., Bombuy E., De Juan C., Llovet JM., De Caralt TM, et al. Preoperative evaluation of biliary anatomy in adult live liver donors with volumetric mangafodipir trisodium enhanced magnetic resonance cholangiography. Liver Transpl. 2004. 10:1391–7.
Article23). Ju MK., Kim MS., Choi GH., Chang HK., Ahn HJ., Kim YS, et al. The efficacy of pretransplant radiologic evaluation for graft volume and anatomy in living donor liver transplantation. J Korean Soc Transplant. 2007. 21:128–34. (주만기, 김명수, 최기홍, 장혜경, 안형준, 김유선, 등. 생체 간이식 공여자의 수술 전 이식간 용적과 해부학적 구조에 대한 영상학적 검사의 유용성. 대한이식학회지 2007;21: 128-34.).24). Park S., Choi GS., Jung J., Cho G., Shin E., Lim C, et al. Clinical efficacy of pretransplant magnetic resonance cholangiography of donor for living donor liver transplantation. J Korean Soc Transplant. 2010. 24:311–5. (박승완, 김형철, 조규 석, 송옥평, 신응진, 임철완, 등. 생체간이식 수술에서 이식 전 제공자 자기공명담관조영술의 임상적 유용성. 대한이식학회지 2010;24: 311-5.).
Article25). Taketomi A., Morita K., Toshima T., Takeishi K., Kayashima H., Ninomiya M, et al. Living donor hepatectomies with procedures to prevent biliary complications. J Am Coll Surg. 2010. 211:456–64.
Article26). Takatsuki M., Eguchi S., Yamanouchi K., Hidaka M., Soyama A., Kanematsu T. Technical refinements of bile duct division in living donor liver surgery. J Hepatobiliary Pancreat Sci. 2011. 18:170–5.
Article27). Testa G., Malago M., Porubsky M., Marinov M., Sankary H., Oberholzer J, et al. Hilar early division of the hepatic duct in living donor right hepatectomy: the probe-and-clamp technique. Liver Transpl. 2006. 12:1337–41.
Article28). Lee KW., Joh JW., Kim SJ., Choi SH., Heo JS., Lee HH, et al. High hilar dissection: new technique to reduce biliary complication in living donor liver transplantation. Liver Transpl. 2004. 10:1158–62.
Article29). Li C., Mi K., Wen T., Yan L., Li B., Yang J, et al. A learning curve for living donor liver transplantation. Dig Liver Dis. 2012. 44:597–602.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term external biliary drainage in living donor liver transplantation using duct-to-duct anastomosis: a single-center experience
- The Role of Bile Duct Probe for Bile Duct Division during Donor Right Hemihepatectomy
- Magnetic Compression Duct-to-duct Anastomosis for Biliary Obstruction in a Patient with Living Donor Liver Transplantation
- Cystic duct anastomosis can be a viable option for biliary reconstruction in case of multiple ducts in right lobe living-donor liver transplantation
- The impact of the multiple bile ducts on postoperative biliary complications in living donor liver transplantation: a single center experience