Ann Hepatobiliary Pancreat Surg.
2021 Aug;25(3):328-335. 10.14701/ahbps.2021.25.3.328.
Cystic duct anastomosis can be a viable option for biliary reconstruction in case of multiple ducts in right lobe living-donor liver transplantation
- Affiliations
-
- 1Centre for Liver and Biliary Sciences, Max Super Speciality Hospital, New Delhi, India
- KMID: 2519288
- DOI: http://doi.org/10.14701/ahbps.2021.25.3.328
Abstract
- Backgrounds/Aims
Multiple ducts in right lobe living-donor liver transplant (LDLT) pose a technical challenge in biliary reconstruction. In the absence of separate recipient hepatic ducts for duct-to-duct anastomoses and certain demerits of hepaticojejunostomy, duct to duct anastomoses with the recipient cystic duct might be a possible solution.
Methods
A total of 329 recipients of LDLT who underwent two or more separate biliary anastomoses at our centre between January 2014 and November 2019 were studied retrospectively. Records of demographic data, donor and graft characteristics, operative details, postoperative biochemical parameters, and biliary complications were analysed.
Results
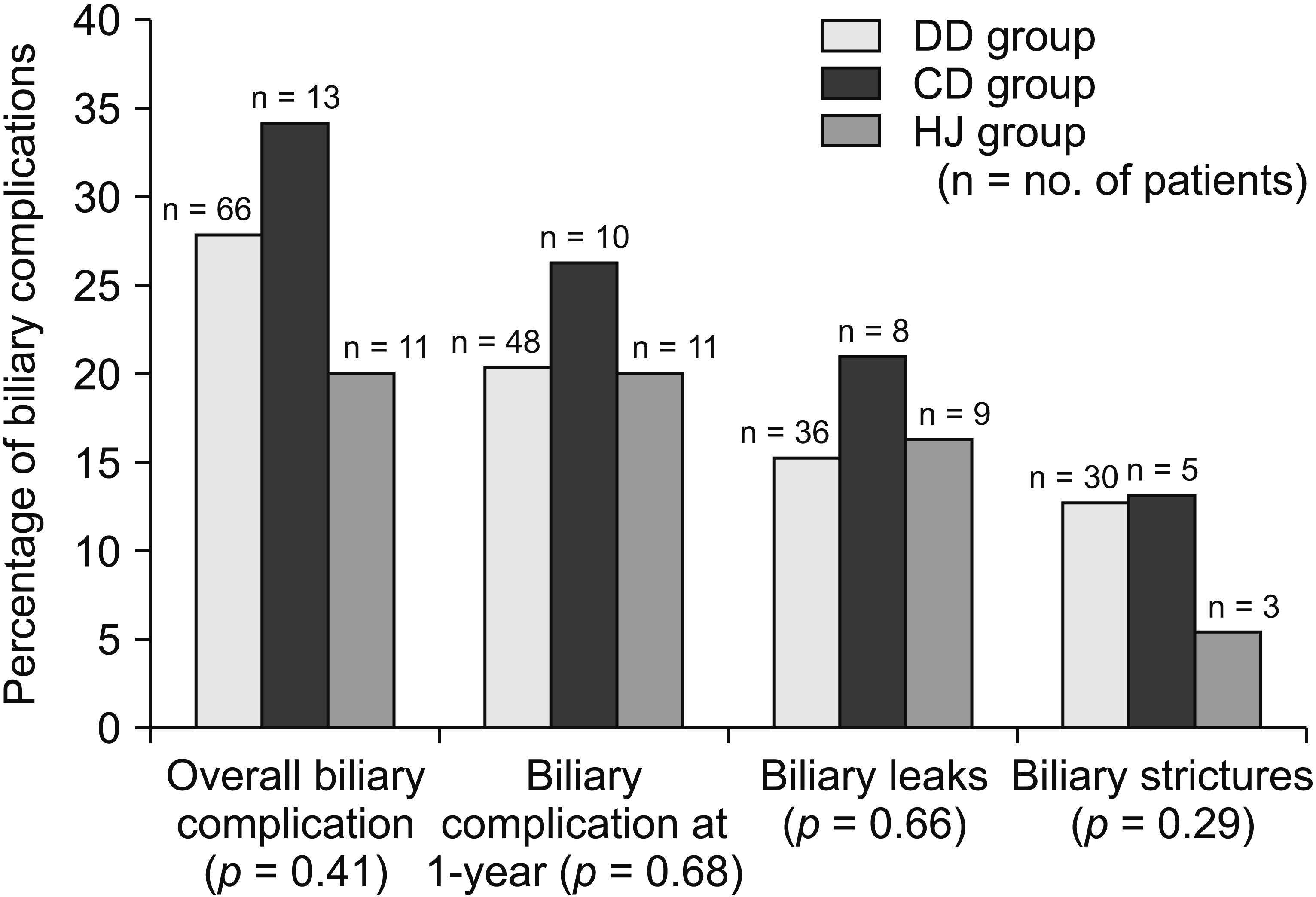
Of 329 recipients, 236 patients (71.7%) underwent purely duct-to-duct (DD group) anastomoses, 38 patients (11.5%) underwent at least one anastomosis with the cystic duct (CD group), and 55 patients (16.7%) underwent at least one hepaticojejunostomy (HJ group). At one year, biliary complication rates of these three groups were 20.3%, 26.3%, and 20.0%, respectively (p = 0.68). Postoperative intensive care unit and overall hospital stay were similar among the three groups. Grades IIIa, IIIb, IV, and V Clavien-Dindo complications were identical. One-year patient survival and graft survival were also similar among the three groups.
Conclusions
Biliary outcomes using the cystic duct may have acceptable outcomes. Similar postoperative results as other means of biliary reconstruction could be anticipated with the cystic duct anastomoses in case of multiple ducts in the graft.
Keyword
Figure
Reference
-
1. Vohra S, Goyal N, Gupta S. 2014; Preoperative CT evaluation of potential donors in living donor liver transplantation. Indian J Radiol Imaging. 24:350–359. DOI: 10.4103/0971-3026.143897. PMID: 25489128. PMCID: PMC4247504.
Article2. Rather SA, Nayeem MA, Agarwal S, Goyal N, Gupta S. 2017; Vascular complications in living donor liver transplantation at a high-volume center: evolving protocols and trends observed over 10 years. Liver Transpl. 23:457–464. DOI: 10.1002/lt.24682. PMID: 27880991.
Article3. Muhammad ZM, Farah Z, Bushra Z, Tsan-S L, Chao-long C. 2016; Results of multiple biliary ducts anastomosis in living donor liver transplantation. Adv Res Gastroentero Hepatol. 2:555581. DOI: 10.19080/argh.2016.02.555581.
Article4. Nguyen NTT, Harring TR, Goss JA, O'Mahony CA. 2015; Biliary reconstruction in pediatric liver transplantation: a case report of biliary complications and review of the literature. J Liver. 4:179. DOI: 10.4172/2167-0889.1000179.
Article5. Tanaka K, Uemoto S, Tokunaga Y, Fujita S, Sano K, Nishizawa T, et al. 1993; Surgical techniques and innovations in living related liver transplantation. Ann Surg. 217:82–91. DOI: 10.1097/00000658-199301000-00014. PMID: 8424706. PMCID: PMC1242738.
Article6. Kawachi S, Shimazu M, Wakabayashi G, Hoshino K, Tanabe M, Yoshida M, et al. 2002; Biliary complications in adult living donor liver transplantation with duct-to-duct hepaticocholedochostomy or Roux-en-Y hepaticojejunostomy biliary reconstruction. Surgery. 132:48–56. DOI: 10.1067/msy.2002.125314. PMID: 12110795.
Article7. Rouch DA, Emond JC, Thistlethwaite JR Jr, Mayes JT, Broelsch CE. 1990; Choledochocholedochostomy without a T tube or internal stent in transplantation of the liver. Surg Gynecol Obstet. 170:239–244. PMID: 2406979.8. Liu CL, Lo CM, Chan SC, Fan ST. 2004; Safety of duct-to-duct biliary reconstruction in right-lobe live-donor liver transplantation without biliary drainage. Transplantation. 77:726–732. DOI: 10.1097/01.TP.0000116604.89083.2F. PMID: 15021836.9. Kadry Z, Cintorino D, Foglieni CS, Fung J. 2004; The pitfall of the cystic duct biliary anastomosis in right lobe living donor liver transplantation. Liver Transpl. 10:1549–1550. DOI: 10.1002/lt.20249. PMID: 15558582.
Article10. Suh KS, Choi SH, Yi NJ, Kwon CH, Lee KU. 2004; Biliary reconstruction using the cystic duct in right lobe living donor liver transplantation. J Am Coll Surg. 199:661–664. DOI: 10.1016/j.jamcollsurg.2004.05.278. PMID: 15454156.
Article11. Asonuma K, Okajima H, Ueno M, Takeichi T, Zeledon Ramirez ME, Inomata Y. 2005; Feasibility of using the cystic duct for biliary reconstruction in right-lobe living donor liver transplantation. Liver Transpl. 11:1431–1434. DOI: 10.1002/lt.20496. PMID: 16237710.
Article12. Turner MA, Fulcher AS. 2001; The cystic duct: normal anatomy and disease processes. Radiographics. 21:3–22. DOI: 10.1148/radiographics.21.1.g01ja093. PMID: 11158640.
Article13. Pina LN, Samoilovich F, Urrutia S, Rodríguez A, Alle L, Ferreres AR. 2015; Surgical considerations of the cystic duct and Heister valves. Surg J (N Y). 1:e23–e27. DOI: 10.1055/s-0035-1567879. PMID: 28824966. PMCID: PMC5530626.14. Chan SC, Fan ST. 2008; Biliary complications in liver transplantation. Hepatol Int. 2:399–404. DOI: 10.1007/s12072-008-9092-z. PMID: 19669315. PMCID: PMC2716905.
Article15. Gondolesi GE, Varotti G, Florman SS, Muñoz L, Fishbein TM, Emre SH, et al. 2004; Biliary complications in 96 consecutive right lobe living donor transplant recipients. Transplantation. 77:1842–1848. DOI: 10.1097/01.TP.0000123077.78702.0C. PMID: 15223901.
Article16. Malagó M, Testa G, Hertl M, Lang H, Paul A, Frilling A, et al. 2002; Biliary reconstruction following right adult living donor liver transplantation end-to-end or end-to-side duct-to-duct anastomosis. Langenbecks Arch Surg. 387:37–44. DOI: 10.1007/s00423-002-0282-1. PMID: 11981683.
Article17. Salvalaggio PR, Whitington PF, Alonso EM, Superina RA. 2005; Presence of multiple bile ducts in the liver graft increases the incidence of biliary complications in pediatric liver transplantation. Liver Transpl. 11:161–166. DOI: 10.1002/lt.20288. PMID: 15666393.
Article18. Pamecha V, Sasturkar SV, Sinha PK, Mohapatra N, Patil N. 2021; Biliary reconstruction in adult living donor liver transplantation: the all-knots-outside technique. Liver Transpl. 27:525–535. DOI: 10.1002/lt.25862. PMID: 32767818.
Article19. Kollmann D, Goldaracena N, Sapisochin G, Linares I, Selzner N, Hansen BE, et al. 2018; Living donor liver transplantation using selected grafts with 2 bile ducts compared with 1 bile duct does not impact patient outcome. Liver Transpl. 24:1512–1522. DOI: 10.1002/lt.25197.
Article20. Arikan T, Emek E, Bozkurt B, Mammadov E, Ceyhan O, Sahin T, et al. 2019; Does multiple bile duct anastomosis in living donor liver transplantation affect the postoperative biliary complications? Transplant Proc. 51:2473–2477. DOI: 10.1016/j.transproceed.2019.01.160. PMID: 31405743.
Article21. Kim EJ, Lim S, Chu CW, Ryu JH, Yang K, Park YM, et al. 2017; Clinical impacts of donor types of living vs. deceased donors: predictors of one-year mortality in patients with liver transplantation. J Korean Med Sci. 32:1258–1262. DOI: 10.3346/jkms.2017.32.8.1258. PMID: 28665060. PMCID: PMC5494323.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single Center Experience of Biliary Reconstruction in Living Donor Liver Transplantation: Duct-to-Duct Anastomosis
- The Role of Bile Duct Probe for Bile Duct Division during Donor Right Hemihepatectomy
- The impact of the multiple bile ducts on postoperative biliary complications in living donor liver transplantation: a single center experience
- Biliary Complications after Living Donor Liver Transplanstation
- Magnetic Compression Duct-to-duct Anastomosis for Biliary Obstruction in a Patient with Living Donor Liver Transplantation