J Korean Soc Transplant.
2015 Sep;29(3):148-159. 10.4285/jkstn.2015.29.3.148.
The Feasibility of Right Posterior Sector Graft in the Adult Living Donor Liver Transplantation
- Affiliations
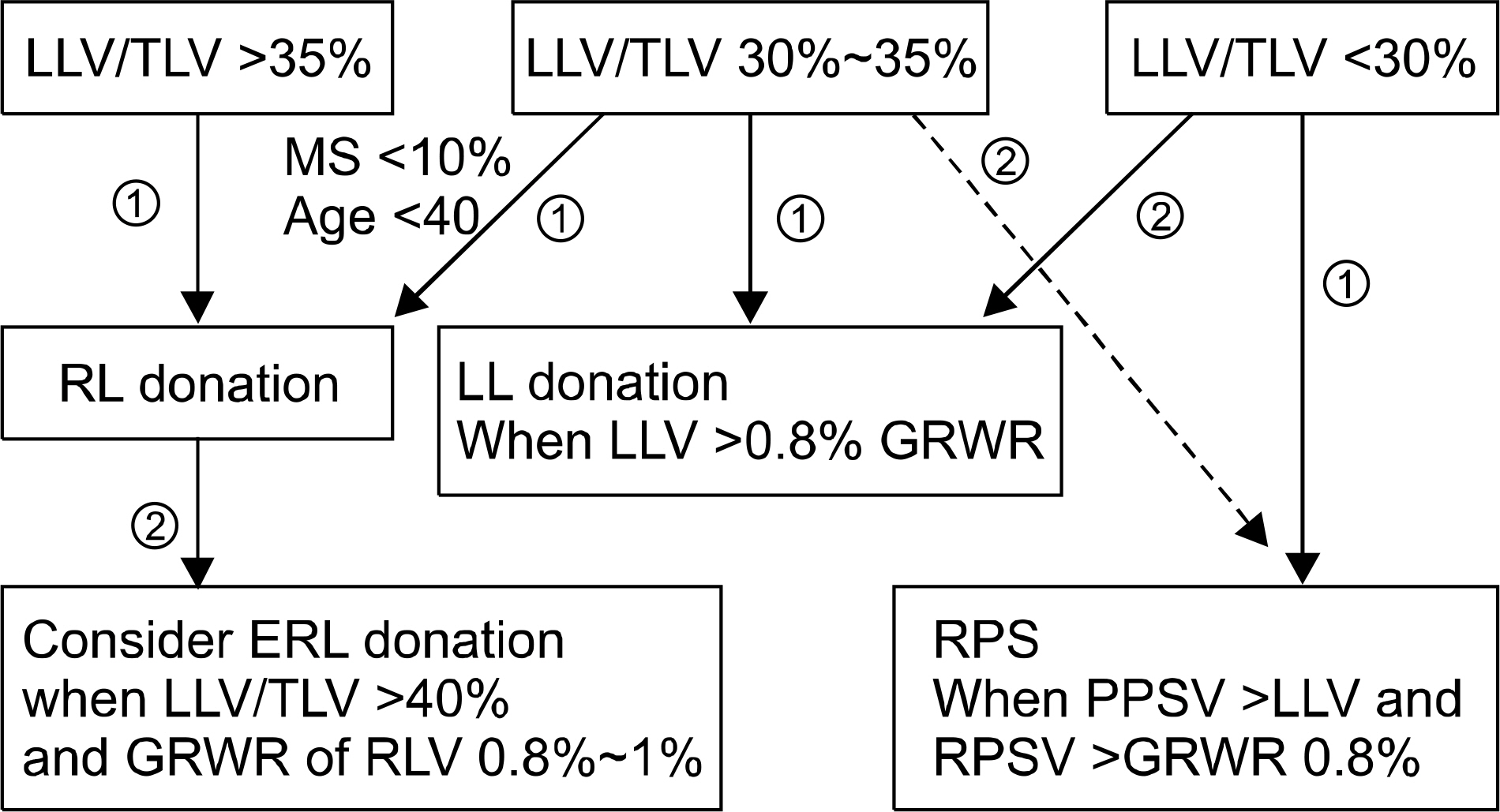
-
- 1Department of Liver Transplantation and Hepatobiliary Surgery, Ajou University School of Medicine, Suwon, Korea. drbwkim@ajou.ac.kr
- KMID: 2202587
- DOI: http://doi.org/10.4285/jkstn.2015.29.3.148
Abstract
- BACKGROUND
The aim of this study is to evaluate the feasibility of living donor liver transplantation (LDLT) using an right posterior sector (RPS) graft selected by liver volumetry of living donors.
METHODS
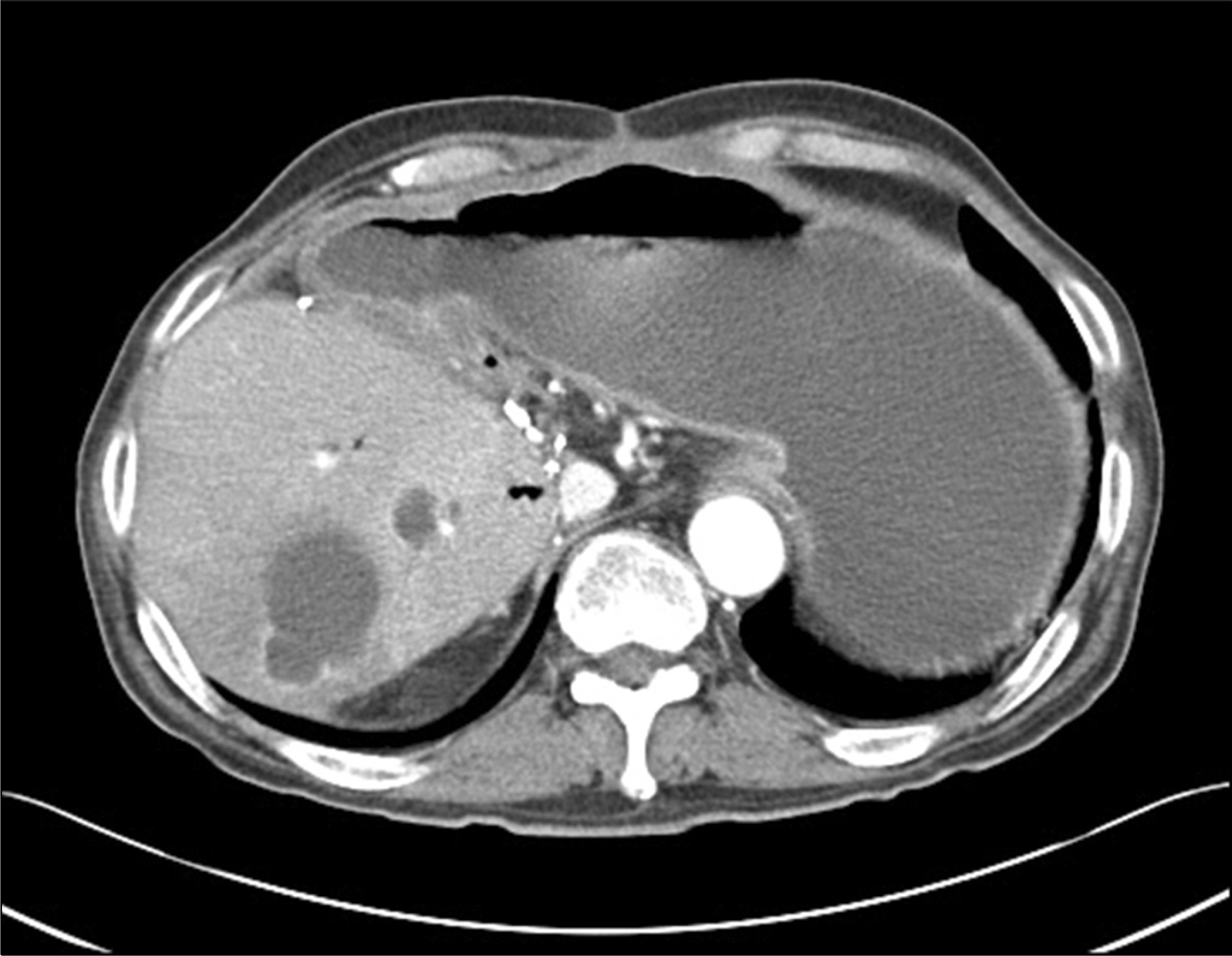
From April 2008 to August 2014, 132 LDLTs were performed in our hospital. Of these, 20 recipients (15.1%) received an RPS graft. Perioperative data of LDLTs using an RPS graft were analyzed retrospectively.
RESULTS
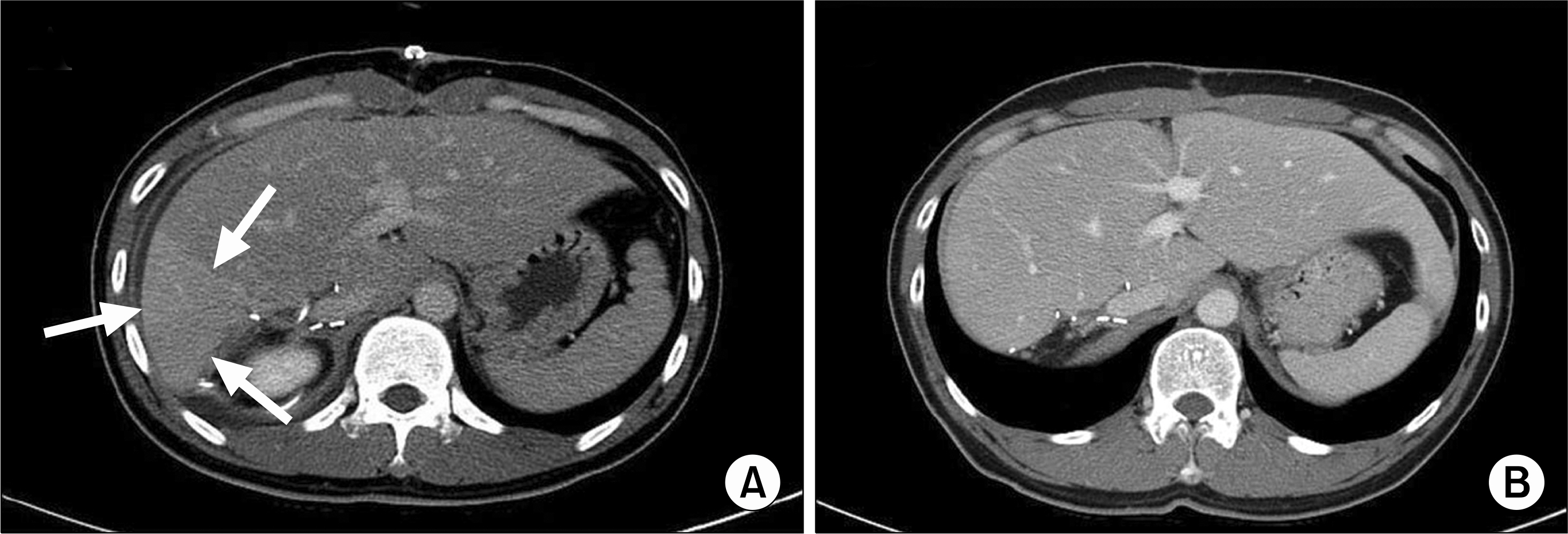
Mean of the Model for End-stage Liver Disease score of the 20 recipients was 12.1+/-6.2. The mean right liver volume was 72.4%+/-3.1% of total liver volume (TLV) and the mean volume of RPS was 38.2%+/-5.3% of TLV. Anatomical anomalies were found in the portal vein (PV) of 14 donors (70%), in the hepatic artery of one donor (5%), and bile duct of seven donors (35%). All donors were discharged with normal liver function. Two donors (10%) developed bile leakage after RPS donation. None of the recipients experienced complication associated with hepatic artery and PV anastomosis. One recipient had in-hospital mortality due to pneumonia. The remaining 19 recipients were discharged with good graft function. Four recipients (20%) developed biliary stricture and one (5%) had a liver abscess during follow-up.
CONCLUSIONS
The RPS donor had a high incidence of abnormal anatomy of PV. LDLT using an RPS graft might have high incidence of biliary complications. We think that selection of an RPS graft from a donor with an inappropriately large right lobe volume could expand the donor pool and be a feasible option in LDLT.
MeSH Terms
Figure
Reference
-
References
1). Gali B, Rosen CB, Plevak DJ. Living donor liver transplantation: selection, perioperative care, and outcome. J Intensive Care Med. 2012; 27:71–8.2). Campos BD, Botha JF. Strategies to optimize donor safety with smaller grafts for adult-to-adult living donor liver transplantation. Curr Opin Organ Transplant. 2012; 17:230–4.
Article3). Barr ML, Belghiti J, Villamil FG, Pomfret EA, Sutherland DS, Gruessner RW, et al. A report of the Vancouver Forum on the care of the live organ donor: lung, liver, pancreas, and intestine data and medical guidelines. Transplantation. 2006; 81:1373–85.
Article4). Kim BW, Xu W, Wang HJ, Park YK, Lee K, Kim MW. Volumetry-based selection of right posterior sector grafts for adult living donor liver transplantation. Liver Transpl. 2011; 17:1046–58.
Article5). Yoshizumi T, Ikegami T, Kimura K, Uchiyama H, Ikeda T, Shirabe K, et al. Selection of a right posterior sector graft for living donor liver transplantation. Liver Transpl. 2014; 20:1089–96.
Article6). Hori T, Kirino I, Uemoto S. Right posterior segment graft in living donor liver transplantation. Hepatol Res. Epub. 2015 Jan 6. DOI:. http://dx.doi.org/10.1111/hepr.12469.7). Hwang S, Lee SG, Lee YJ, Park KM, Kim KH, Ahn CS, et al. Donor selection for procurement of right posterior segment graft in living donor liver transplantation. Liver Transpl. 2004; 10:1150–5.
Article8). Sugawara Y, Makuuchi M, Takayama T, Mizuta K, Kawarasaki H, Imamura H, et al. Liver transplantation using a right lateral sector graft from a living donor to her granddaughter. Hepatogastroenterology. 2001; 48:261–3.9). Kyoden Y, Tamura S, Sugawara Y, Akamatsu N, Matsui Y, Togashi J, et al. Biliary complications in right lateral sector graft live donor liver transplantation. Transpl Int. 2008; 21:332–9.
Article10). Marubashi S, Dono K, Nagano H, Kobayashi S, Takeda Y, Umeshita K, et al. Biliary reconstruction in living donor liver transplantation: technical invention and risk factor analysis for anastomotic stricture. Transplantation. 2009; 88:1123–30.
Article11). Leelaudomlipi S, Sugawara Y, Kaneko J, Matsui Y, Ohkubo T, Makuuchi M. Volumetric analysis of liver segments in 155 living donors. Liver Transpl. 2002; 8:612–4.
Article12). Sugawara Y, Makuuchi M, Takayama T, Imamura H, Kaneko J. Right lateral sector graft in adult living-related liver transplantation. Transplantation. 2002; 73:111–4.13). Stange BJ, Glanemann M, Nuessler NC, Settmacher U, Steinmuller T, Neuhaus P. Hepatic artery thrombosis after adult liver transplantation. Liver Transpl. 2003; 9:612–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Liver retransplantation for adult recipients
- Revolution and Refinement of Surgical Techniques for Living Donor Partial Liver Transplantation
- Anatomical limits in living donor liver transplantation
- "Small-for-size Graft" and "Small-for-size Syndrome" in Living Donor Liver Transplantation