J Korean Neurosurg Soc.
2015 Aug;58(2):163-166. 10.3340/jkns.2015.58.2.163.
Phenytoin Induced Erythema Multiforme after Cranial Radiation Therapy
- Affiliations
-
- 1Department of Neurosurgery, Ankara Ataturk Education and Research Hospital, Ankara, Turkey. atillakazanci@gmail.com
- 2Department of Neurosurgery, Ankara Bayindir Hospital, Ankara, Turkey.
- KMID: 2191329
- DOI: http://doi.org/10.3340/jkns.2015.58.2.163
Abstract
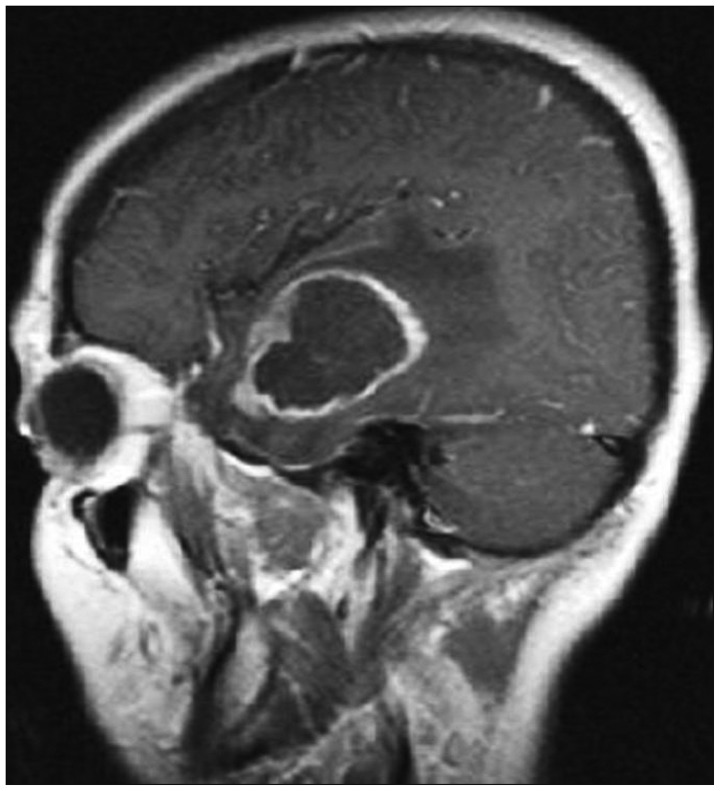
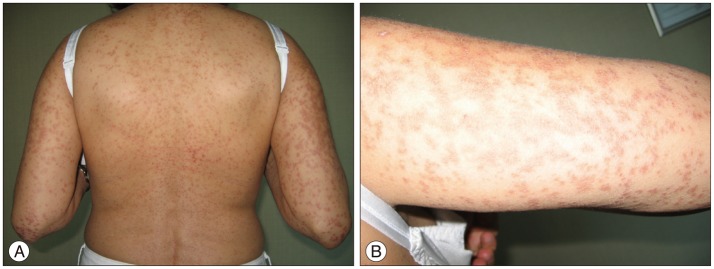
- The prophylactic use of phenytoin during and after brain surgery and cranial irradiation is a common measure in brain tumor therapy. Phenytoin has been associated with variety of adverse skin reactions including urticaria, erythroderma, erythema multiforme (EM), Stevens-Johnson syndrome, and toxic epidermal necrolysis. EM associated with phenytoin and cranial radiation therapy (EMPACT) is a rare specific entity among patients with brain tumors receiving radiation therapy while on prophylactic anti-convulsive therapy. Herein we report a 41-year-old female patient with left temporal glial tumor who underwent surgery and then received whole brain radiation therapy and chemotherapy. After 24 days of continous prophylactic phenytoin therapy the patient developed minor skin reactions and 2 days later the patient returned with generalized erythamatous and itchy maculopapuler rash involving neck, chest, face, trunk, extremities. There was significant periorbital and perioral edema. Painful mucosal lesions consisting of oral and platal erosions also occurred and prevented oral intake significantly. Phenytoin was discontinued gradually. Systemic admistration of corticosteroids combined with topical usage of steroids for oral lesions resulted in complete resolution of eruptions in 3 weeks. All cutaneous lesions in patients with phenytoin usage with the radiotherapy must be evoluated with suspicion for EM.
Keyword
MeSH Terms
Figure
Reference
-
1. Ahmed I, Reichenberg J, Lucas A, Shehan JM. Erythema multiforme associated with phenytoin and cranial radiation therapy : a report of three patients and review of the literature. Int J Dermatol. 2004; 43:67–73. PMID: 14693027.
Article2. Arif H, Buchsbaum R, Weintraub D, Koyfman S, Salas-Humara C, Bazil CW, et al. Comparison and predictors of rash associated with 15 antiepileptic drugs. Neurology. 2007; 68:1701–1709.
Article3. Baba M, Karakaş M, Aksungur VL, Homan S, Yücel A, Acar MA, et al. The anticonvulsant hypersensitivity syndrome. J Eur Acad Dermatol Venereol. 2003; 17:399–401. PMID: 12834448.
Article4. Barbosa LA, Teixeira CR. Erythema multiforme associated with prophylactic use of phenytoin during cranial radiation therapy. Am J Health Syst Pharm. 2008; 65:1048–1050. PMID: 18499877.
Article5. Lin MS, Dai YS, Pwu RF, Chen YH, Chang NC. Risk estimates for drugs suspected of being associated with Stevens-Johnson syndrome and toxic epidermal necrolysis : a case-control study. Intern Med J. 2005; 35:188–190. PMID: 15737140.
Article6. Mamon HJ, Wen PY, Burns AC, Loeffler JS. Allergic skin reactions to anticonvulsant medications in patients receiving cranial radiation therapy. Epilepsia. 1999; 40:341–344.
Article7. Man CB, Kwan P, Baum L, Yu E, Lau KM, Cheng AS, et al. Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese. Epilepsia. 2007; 48:1015–1018. PMID: 17509004.
Article8. Micali G, Linthicum K, Han N, West DP. Increased risk of erythema multiforme major with combination anticonvulsant and radiation therapies. Pharmacotherapy. 1999; 19:223–227. PMID: 10030773.
Article9. Mockenhaupt M, Messenheimer J, Tennis P, Schlingmann J. Risk of Stevens-Johnson syndrome and toxic epidermal necrolysis in new users of antiepileptics. Neurology. 2005; 64:1134–1138. PMID: 15824335.
Article10. Oner Dincbas F, Yörük S, Demirkesen C, Uzel O, Koca S. Toxic epidermal necrolysis after cranial radiotherapy and phenytoin treatment. Onkologie. 2004; 27:389–392. PMID: 15347896.
Article11. Pelekanos J, Camfield P, Camfield C, Gordon K. Allergic rash due to antiepileptic drugs : clinical features and management. Epilepsia. 1991; 32:554–559. PMID: 1831121.
Article12. Roujeau JC, Kelly JP, Naldi L, Rzany B, Stern RS, Anderson T, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995; 333:1600–1607. PMID: 7477195.
Article13. Rzany B, Correia O, Kelly JP, Naldi L, Auquier A, Stern R. Study Group of the International Case Control Study on Severe Cutaneous Adverse Reactions. Risk of Stevens-Johnson syndrome and toxic epidermal necrolysis during first weeks of antiepileptic therapy : a case-control study. Lancet. 1999; 353:2190–2194. PMID: 10392983.
Article14. Welykyj S, Gradini R, Nakao J, Massa M. Carbamazepine-induced eruption histologically mimicking mycosis fungoides. J Cutan Pathol. 1990; 17:111–116. PMID: 2140116.
Article15. Wöhrl S, Loewe R, Pickl WF, Stingl G, Wagner SN. EMPACT syndrome. J Dtsch Dermatol Ges. 2005; 3:39–43. PMID: 16353748.