J Korean Neurosurg Soc.
2013 Sep;54(3):261-264. 10.3340/jkns.2013.54.3.261.
A Long-Term Survival Case of a Primary Malignant Intracerebral Nerve Sheath Tumor
- Affiliations
-
- 1Department of Neurosurgery, Chungbuk National University School of Medicine & Medical Research Institute, Cheongju, Korea. mslee@chungbuk.ac.kr
- KMID: 2190911
- DOI: http://doi.org/10.3340/jkns.2013.54.3.261
Abstract
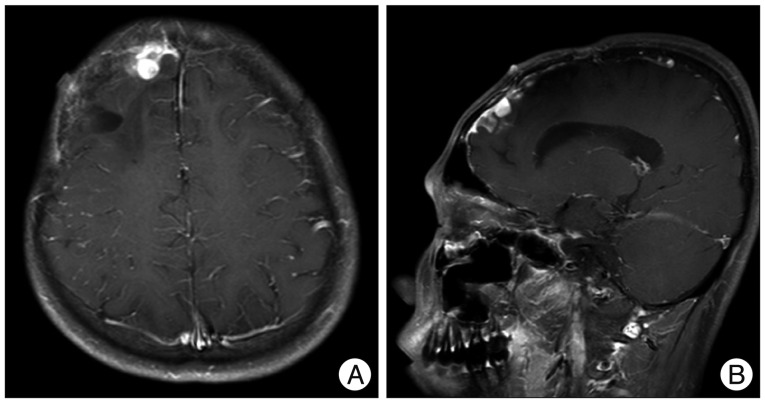
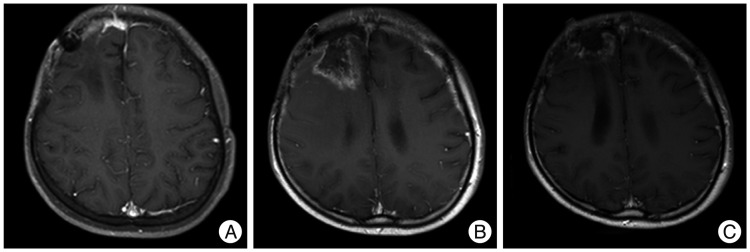
- We report a long-term survival case of a primary malignant intracerebral nerve sheath tumor (MINST) occurring in the right frontal lobe of a 13-year old boy. After the gross total resection (GTR), we have performed radiation therapy but it recurred 50 months after the surgery, so the second GTR was performed. Later, second tumor recurrence was found 4 months after the second surgery. Subsequently the third GTR, radiotherapy, and chemotherapy were carried out. At present, the patient has been remaining alive for 77 months without evidence of tumor recurrence. According to the previous reports, the primary MINST is very rare : there are only 8 cases reported. It is also a fast-growing, invasive tumor with poor outcome. This is the first case that had no recurrence for 50 months after the surgery among the reported cases that had been followed up for more than 5 years. It is supposed that a period of recurrence free survival after GTR and low mitotic activity are associated with the patient's prognosis. A GTR followed by adjuvant radiation therapy and chemotherapy will be recommended to patients of MINST.
Keyword
Figure
Reference
-
1. Barnard ZR, Agarwalla PK, Jeyaretna DS, Farrell CJ, Gerstner ER, Tian D. Sporadic primary malignant intracerebral nerve sheath tumor : case report and literature review. J Neurooncol. 2011; 104:605–610. PMID: 21327709.
Article2. Beauchesne P, Mosnier JF, Schmitt T, Brunon J. Malignant nerve sheath tumor of the right cerebral peduncle : case report. Neurosurgery. 2004; 54:500–503. PMID: 14744297.3. Bhattacharyya AK, Perrin R, Guha A. Peripheral nerve tumors : management strategies and molecular insights. J Neurooncol. 2004; 69:335–349. PMID: 15527099.
Article4. Bruner JM, Humphreys JH, Armstrong DL. Immunocytochemistry of recurring intracerebral nerve sheath tumor. J Neuropathol Exp Neurol. 1984; 43:1. PMID: 6319616.5. Carli M, Ferrari A, Mattke A, Zanetti I, Casanova M, Bisogno G, et al. Pediatric Malignant Peripheral Nerve Sheath Tumor : The Italian and German Soft Tissue Sarcoma Cooperative Group. J Clin Oncol. 2005; 23:8422–8430. PMID: 16293873.
Article6. Chen L, Mao Y, Chen H, Zhou LF. Diagnosis and management of intracranial malignant peripheral nerve sheath tumors. Neurosurgery. 2008; 62:825–832. PMID: 18496188.
Article7. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopatholgic study of 120 cases. Cancer. 1986; 57:2006–2021. PMID: 3082508.
Article8. Enzinger FM, Weiss SW. Malignant tumor of the peripheral nerves. In : Enzinger FM, Weiss SW, editors. Soft Tissue Tumors. ed 3. St Louis, MO: CV Mosby;1995. p. 889–928.9. Kim ET, Namgung H, Shin HD, Lee SI, Kwon JE, Chang MC, et al. Oncologic manifestations of neurofibromatosis type 1 in Korea. J Korean Surg Soc. 2012; 82:205–210. PMID: 22493760.
Article10. Kozić D, Nagulic M, Samardzic M, Ostojic J, Rasulic L, Cvetkovic-Dozic D. Intrapontine malignant nerve sheath tumor : MRI and MRS features. Acta Neurol Belg. 2008; 108:67–71. PMID: 18795600.11. Rees J. Advances in magnetic resonance imaging of brain tumors. Curr Opin Neurol. 2003; 16:643–650. PMID: 14624071.12. Sharma S, Abbott RI, Zagzag D. Malignant intracerebral nerve sheath tumor : A case report and review of the literature. Cancer. 1998; 82:545–552. PMID: 9452273.13. Shin HY. Korean society for pediatric neuro-oncology (KSPNO). Korean J Pediatr Hematol Oncol. 2005; 12:188–200.14. Singh RV, Suys S, Campbell DA, Broome JC. Malignant schwannoma of the cerebellum: case report. Surg Neurol. 1993; 39:128–132. PMID: 8351625.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Peripheral Nerve Sheath Tumor of the Larynx
- Primary Paraspinal Malignant Peripheral Nerve Sheath Tumor
- Epithelioid Malignant Intracerebral Nerve Sheath Tumor: A Case Report and a Comparison with Conventional Type
- Malignant Peripheral Nerve Sheath Tumor of Abdomen
- Malignant Peripheral Nerve Sheath Tumor of the Cauda Equina in Type I Neurofibromatosis: Case Report