J Korean Neurosurg Soc.
2013 Jun;53(6):364-367. 10.3340/jkns.2013.53.6.364.
Delayed Unilateral Soft Palate Palsy without Vocal Cord Involvement after Microvascular Decompression for Hemifacial Spasm
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kwanpark@skku.edu
- KMID: 2190825
- DOI: http://doi.org/10.3340/jkns.2013.53.6.364
Abstract
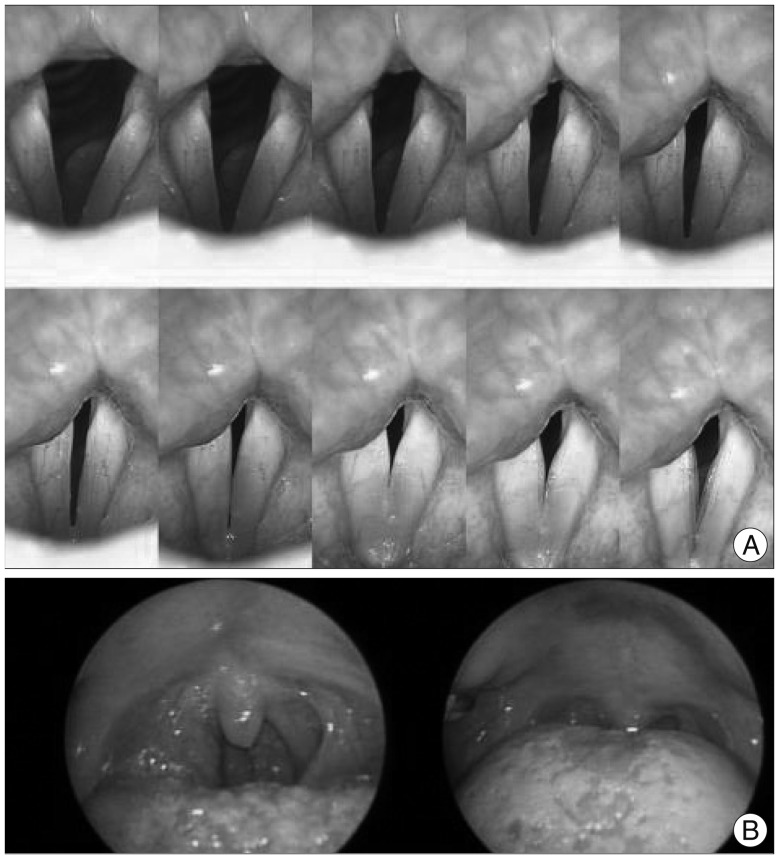
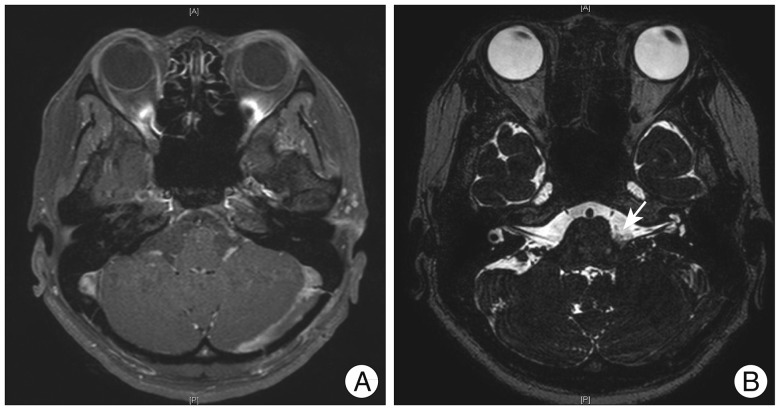
- Microvascular decompression is a very effective and relatively safe surgical modality in the treatment of hemifacial spasm. But rare debilitating complications have been reported such as cranial nerve dysfunctions. We have experienced a very rare case of unilateral soft palate palsy without the involvement of vocal cord following microvascular decompression. A 33-year-old female presented to our out-patient clinic with a history of left hemifacial spasm for 5 years. On postoperative 5th day, patient started to exhibit hoarsness with swallowing difficulty. Symptoms persisted despite rehabilitation. Various laboratory work up with magnetic resonance image showed no abnormal lesions. Two years after surgery patient showed complete recovery of unitaleral soft palate palsy. Various etiologies of unilateral soft palate palsy are reviewed as the treatment and prognosis differs greatly on the cause. Although rare, it is important to keep in mind that such complication could occur after microvascular decompression.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Significance of Arachnoid Dissection to Obtain Optimal Exposure of Lower Cranial Nerves and the Facial Nerve Root Exit Zone during Microvascular Decompression Surgery
Bum-Tae Kim
J Korean Neurosurg Soc. 2014;55(1):64-65. doi: 10.3340/jkns.2014.55.1.64.
Reference
-
1. Cohen-Gadol AA. Microvascular decompression surgery for trigeminal neuralgia and hemifacial spasm: naunces of the technique based on experiences with 100 patients and review of the literature. Clin Neurol Neurosurg. 2011; 113:844–853. PMID: 21752534.
Article2. Erman AB, Kejner AE, Hogikyan ND, Feldman EL. Disorders of cranial nerves IX and X. Semin Neurol. 2009; 29:85–92. PMID: 19214937.
Article3. Fang TJ, Tam YY, Courey MS, Li HY, Chiang HC. Unilateral high vagal paralysis: relationship of the severity of swallowing disturbance and types of injuries. Laryngoscope. 2011; 121:245–249. PMID: 21271569.
Article4. Gillig PM, Sanders RD. Cranial Nerves IX, X, XI, and XII. Psychiatry (Edgmont). 2010; 7:37–41. PMID: 20532157.5. Jeon CJ, Kong DS, Lee JA, Park K. The efficacy and safety of microvascular decompression for hemifacial spasm in elderly patients. J Korean Neurosurg Soc. 2010; 47:442–445. PMID: 20617090.
Article6. Lapresle J, Faux N. [Unilateral involvement of IX, X, Xi and XII in cervical zoster. Cranial nerve contribution to vascular pathology]. J Neurol Sci. 1981; 52:351–357. PMID: 7310438.7. Lapresle J, Lasjaunias P, Thévenier D. [Transitory paralysis of cranial nerves IX, X and XII as well as the left VII after angiography. Contribution to the ischemic pathology of the cranial nerves]. Rev Neurol (Paris). 1980; 136:787–791. PMID: 7209243.8. Nusbaum AO, Som PM, Dubois P, Silvers AR. Isolated vagal nerve palsy associated with a dissection of the extracranial internal carotid artery. AJNR Am J Neuroradiol. 1998; 19:1845–1847. PMID: 9874534.9. Paniello RC, Edgar JD, Kallogjeri D, Piccirillo JF. Medialization versus reinnervation for unilateral vocal fold paralysis: a multicenter randomized clinical trial. Laryngoscope. 2011; 121:2172–2179. PMID: 21898419.
Article10. Resnick DK, Jannetta PJ. Hyperactive rhizopathy of the vagus nerve and microvascular decompression. Case report. J Neurosurg. 1999; 90:580–582. PMID: 10067935.
Article11. Rhee DJ, Kong DS, Park K, Lee JA. Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien). 2006; 148:839–843. discussion 843. PMID: 16804640.
Article12. Tang SC, Jeng JS, Liu HM, Yip PK. Isolated vagus nerve palsy probably associated with herpes simplex virus infection. Acta Neurol Scand. 2001; 104:174–177. PMID: 11551239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Generalized Convulsion and Delayed Emergence following Microvascular Decompression Surgery under General Anesthesia: A case report
- Delayed Cranial Nerve Palsy after Microvascular Decompression for Hemifacial Spasm
- Intraoperative monitoring of microvascular decompression in hemifacial spasm
- Severe Hemifacial Spasm is a Predictor of Severe Indentation and Facial Palsy after Microdecompression Surgery
- Microvascular triple decompression for combined simultaneous trigeminal neuralgia, hemifacial spasm, and pulsatile tinnitus due to separate offending vessels