J Korean Assoc Oral Maxillofac Surg.
2011 Jun;37(3):237-240. 10.5125/jkaoms.2011.37.3.237.
Iatrogenic epidermoid cyst in the parotid gland: A case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Yonsei University (Gangnam Severance Hospital), Seoul, Korea. omshuh@yuhs.ac
- 2Department of Oral and Maxillofacial Radiology, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 2189785
- DOI: http://doi.org/10.5125/jkaoms.2011.37.3.237
Abstract
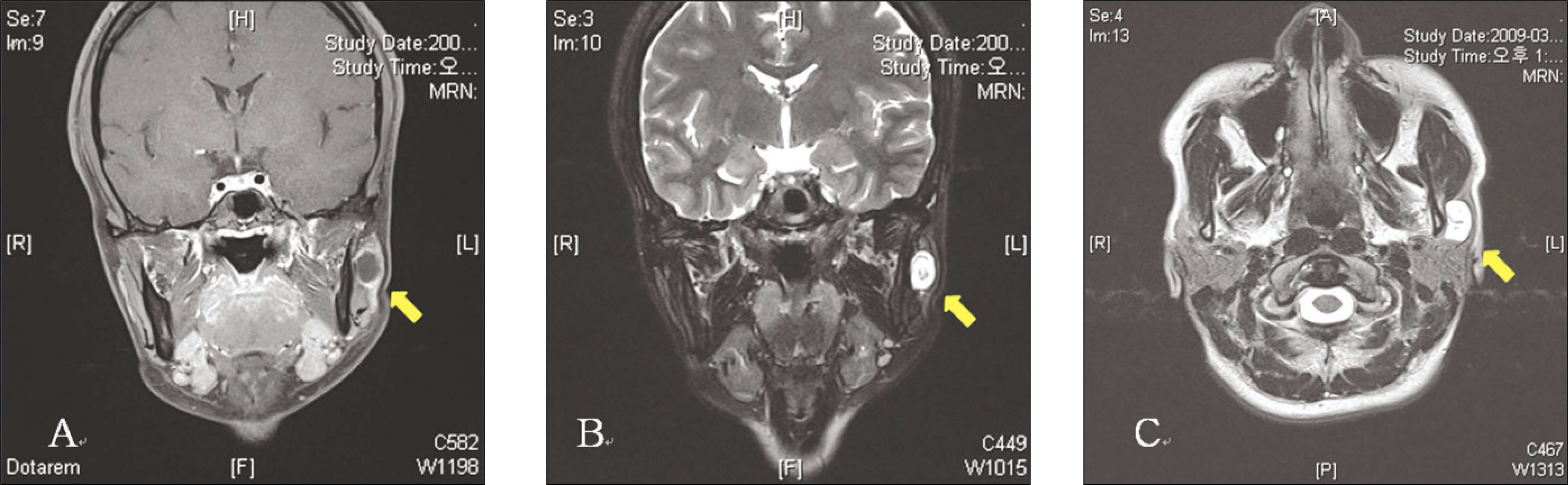
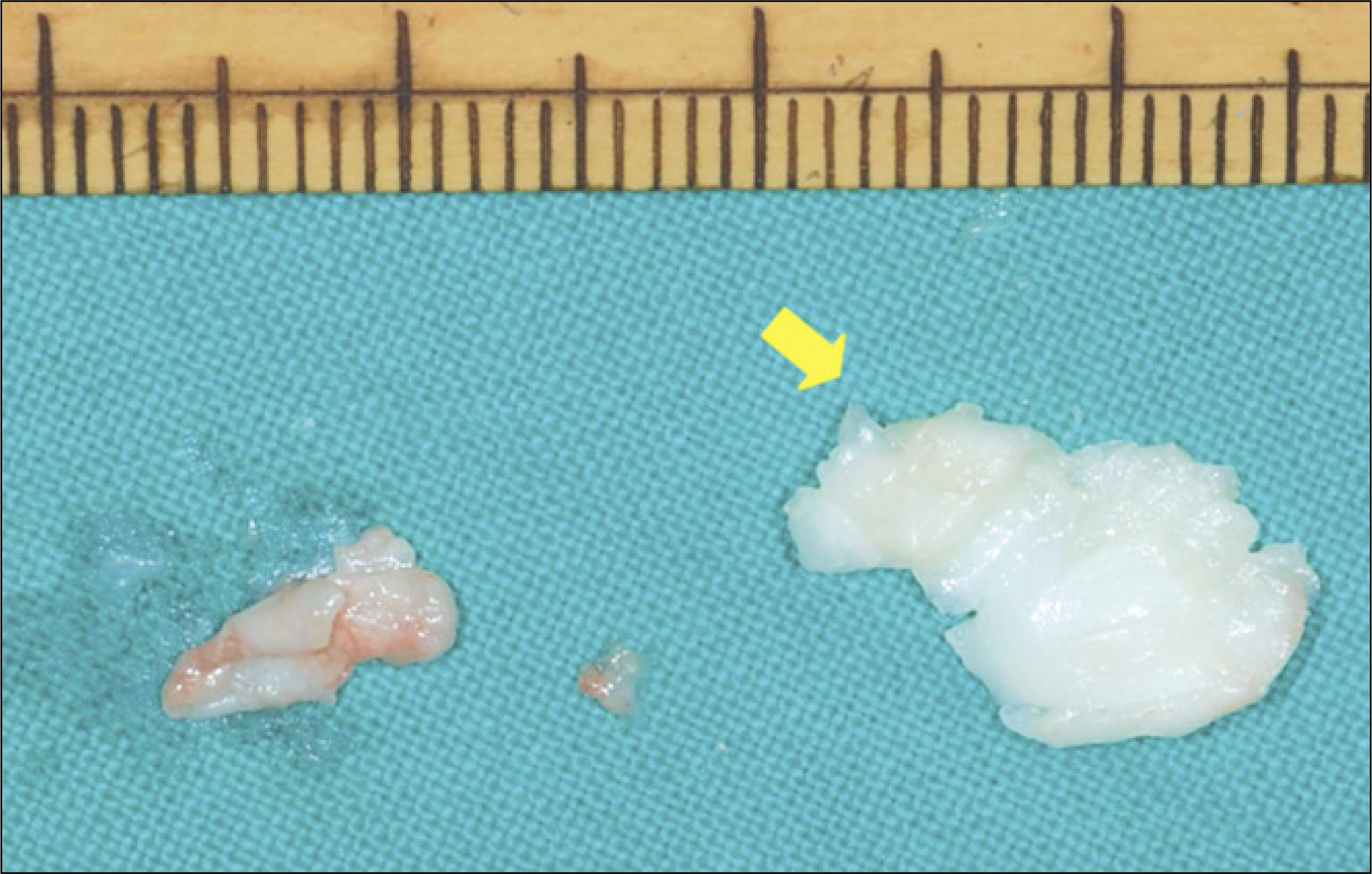
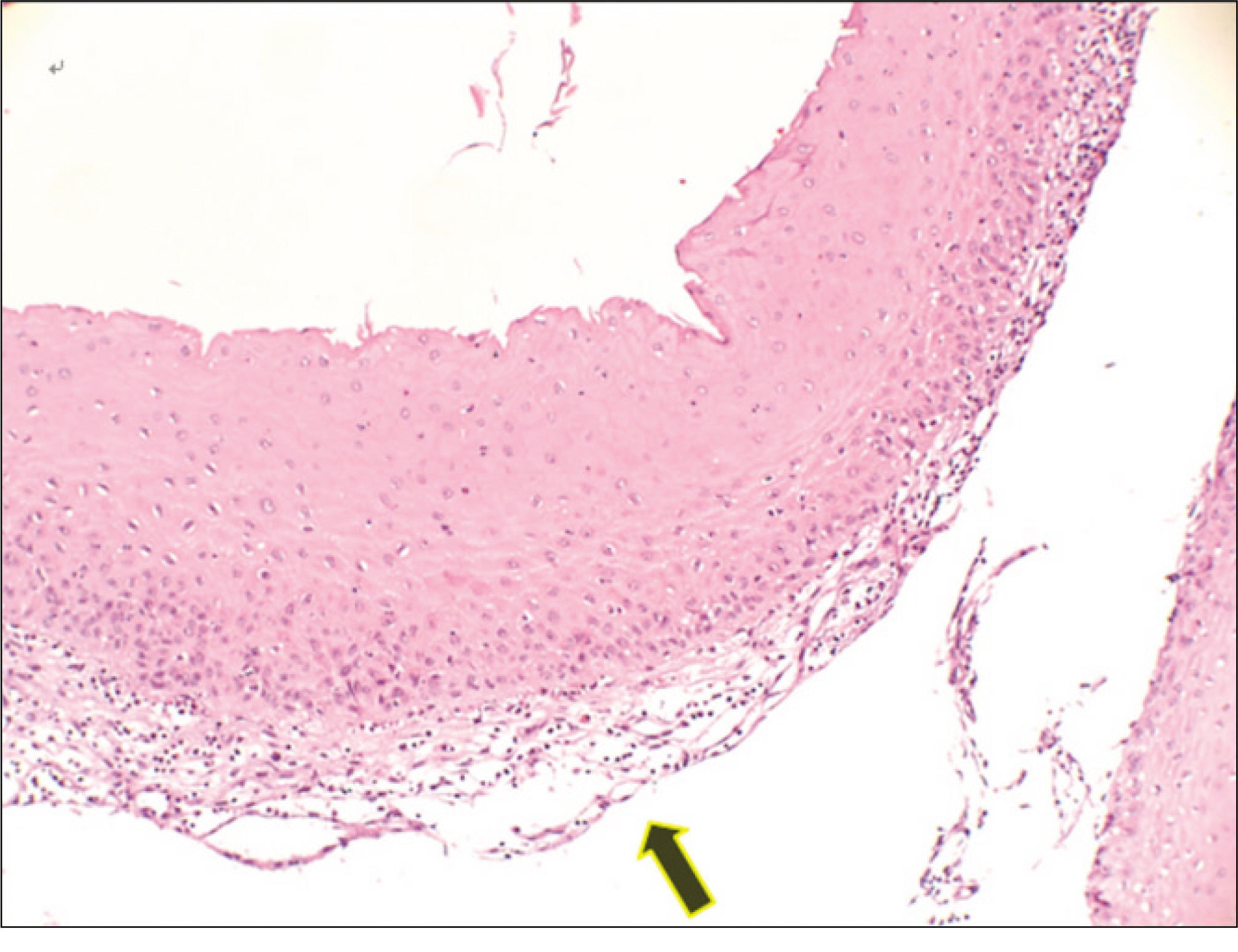
- Epidermoid cysts presents as a nodular and fluctuant subcutaneous lesion beneath the skin and are most common in acne-prone areas of the head, neck and back. This cyst often arises after localized inflammation of the hair follicle and occasionally after the implantation of epithelium following trauma and surgery including a biopsy procedure. It is often associated with Gardner syndrome, particularly before puberty. The lesion is normally treated by a surgical excision or enucleation, and recurrence is uncommon. A 27 year old woman complained of a swelling of the left parotid gland when she visited our clinic. A cystic lesion was found in the left parotid gland from the high signal intensity on the MR images. Ultrasonography showed that the cystic lesion was heterogeneous echogenic. Six months earlier, botulinum toxin was injected in her left masseter muscles six months earlier and progressive swelling of the left parotid area was noticed four months after treatment. The lesion was surgically removed. It was encapsulated by a thin wall and filled mainly with keratin. The final diagnosis was an epidermoid cyst.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Handa U, Chhabra S, Mohan H. Epidermal inclusion cyst:: cytomorphological features and differential diagnosis. Diagn Cytopathol. 2008; 36:861–3.
Article2. Thompson AC, Bradley PJ. Iatrogenic epidermoid cyst of the parotid region following ear surgery. J Laryngol Otol. 1991; 105:227–8.3. Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2009; 67:52–7.
Article4. Fliss DM, Puterman M, Tovi F. Iatrogenic cholesteatoma of the neck. Head Neck. 1989; 11:558–61.
Article5. Tovi F, Bartal N, Zirkin C. Epidermal cysts of temporal fossa: an unusual complication of ear surgery. Ann Otol Rhinol Laryngol. 1985; 94:162–4.
Article6. Tidmore T, Hirschi S, Chang CW. Floor of the mouth epidermoid cyst enlarging after pregnancy. J Otolaryngol Head Neck Surg. 2009; 38:E124–6.7. Nalini G, Nandita K, Satyawati M, Jaimanti B. Squamous cell carcinoma in a mucosal epithermal inclusion cyst. J Otolaryngol. 2004; 33:271–2.8. Van Epps KJ, Kuszyk BS, Hofmann LV, Fishman EK. Epidermoid inclusion cysts seen on CT of a patient with Gardner's syndrome. AJR Am J Roentgenol. 1999; 173:858–9.
Article9. Narisawa Y, Kohda H. Cutaneous cysts of Gardner's syndrome are similar to follicular stem cells. J Cutan Pathol. 1995; 22:115–21.
Article10. Richardson GS, Clairmont AA, Erickson ER. Cystic lesions of the parotid gland. Plast Reconstr Surg. 1978; 61:364–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Iatrogenic Epidermoid Cyst in the Temporal Bone Following Tympanoplasty through Retroauricular Approach
- Dermoid Cyst of the Parotid Gland: A Case Report
- A Case of Epidermoid Cyst of the Testicle
- Epidermoid Cyst of the Testis Demonstrating Double Target Sign: A Case Report
- A case report of the salivary duct cyst and review of literatures