J Breast Cancer.
2015 Dec;18(4):404-408. 10.4048/jbc.2015.18.4.404.
Primary Neuroendocrine Carcinoma of the Breast with Clinical Features of Inflammatory Breast Carcinoma: A Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea. pay526@naver.com
- 2Kangwon National University Graduate School, Chuncheon, Korea.
- 3Department of Pathology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- KMID: 2176294
- DOI: http://doi.org/10.4048/jbc.2015.18.4.404
Abstract
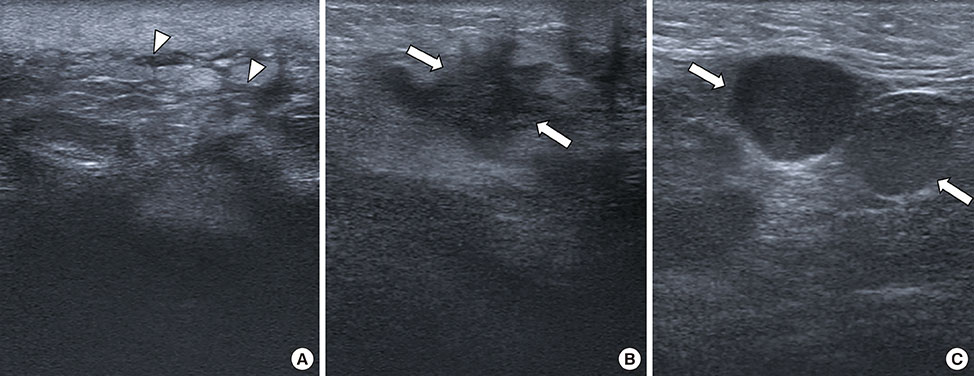
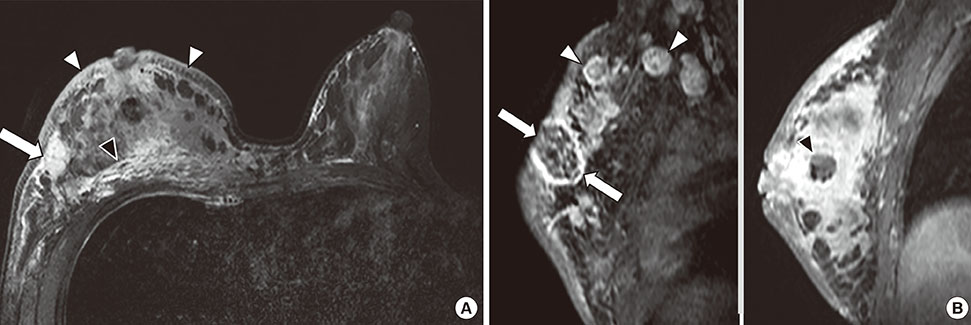
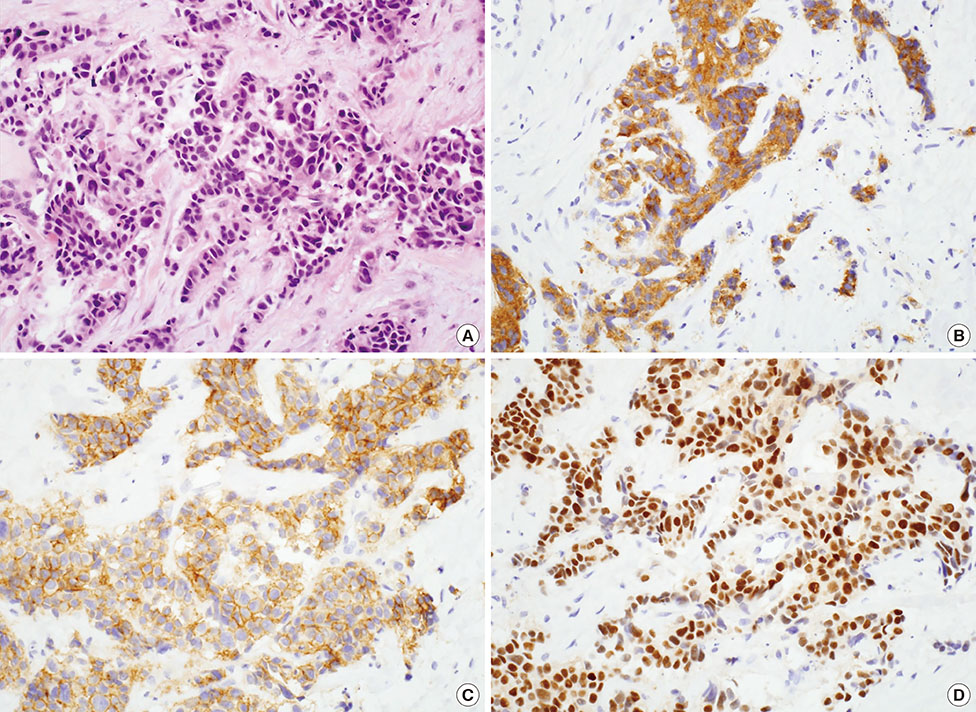
- Primary neuroendocrine carcinoma of the breast (NECB) is a very rare type of invasive breast carcinoma. Most NECBs appear on breast imaging as solid masses of varied shapes and margins, and have worse clinical outcomes than does invasive ductal carcinoma, not otherwise specified. However, there have been no reports to date regarding NECB with features of inflammatory breast carcinoma. Here, we describe the clinical, radiol-ogic, and pathologic findings of the first reported case of primary NECB presenting as inflammatory breast carcinoma. The patient complained of diffuse right breast enlargement and erythema. Mammography identified severe breast edema and axillary lymphadenopathy. Ultrasound detected an irregular, angular, hypoechoic mass with dermal lymphatic dilatation. On magnetic resonance imaging, the mass had rim enhancement and the entire right breast showed heterogeneous enhancement with malignant kinetic features. Pathology identified the mass as a primary NECB with positive for synaptophysin, CD56, estrogen and progesterone receptors.
MeSH Terms
Figure
Reference
-
1. Kim JW, Woo OH, Cho KR, Seo BK, Yong HS, Kim A, et al. Primary large cell neuroendocrine carcinoma of the breast: radiologic and pathologic findings. J Korean Med Sci. 2008; 23:1118–1120.
Article2. Zhang Y, Chen Z, Bao Y, Du Z, Li Q, Zhao Y, et al. Invasive neuroendocrine carcinoma of the breast: a prognostic research of 107 Chinese patients. Neoplasma. 2013; 60:215–222.
Article3. Ellis IO, Schnitt SJ, Sastre-Garau X. Invasive breast carcinoma. In : Tavassoli FA, Devilee P, editors. International Agency for Research on Cancer. World Health Organization. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. Lyon: IARC Press;2003. p. 13–59.4. Valentim MH, Monteiro V, Marques JC. Primary neuroendocrine breast carcinoma: a case report and literature review. Radiol Bras. 2014; 47:125–127.
Article5. Günhan-Bilgen I, Zekioglu O, Ustün EE, Memis A, Erhan Y. Neuroendocrine differentiated breast carcinoma: imaging features correlated with clinical and histopathological findings. Eur Radiol. 2003; 13:788–793.
Article6. Bussolati G, Badve S. Carcinomas with neuroendocrine features. In : Lakhani SR, Schnitt SJ, Tan PH, van de Vijver MJ, editors. WHO Classification of Tumours of the Breast. 4th ed. Lyon: IARC Press;2012. p. 62–63.7. Wei B, Ding T, Xing Y, Wei W, Tian Z, Tang F, et al. Invasive neuroendocrine carcinoma of the breast: a distinctive subtype of aggressive mammary carcinoma. Cancer. 2010; 116:4463–4473.8. Kwon SY, Bae YK, Gu MJ, Choi JE, Kang SH, Lee SJ, et al. Neuroendocrine differentiation correlates with hormone receptor expression and decreased survival in patients with invasive breast carcinoma. Histopathology. 2014; 64:647–659.
Article9. Breast cancer staging, 7th edition. American Joint Committee on Cancer;Accessed April 24th, 2015. https://cancerstaging.org/references-tools/quickreferences/Documents/BreastMedium.pdf.10. Buttar A, Mittal K, Khan A, Bathini V. Effective role of hormonal therapy in metastatic primary neuroendocrine breast carcinoma. Clin Breast Cancer. 2011; 11:342–345.
Article11. Ochoa R, Sudhindra A, Garcia-Buitrago M, Romilly AP, Cortes J, Gomez H, et al. Small-cell cancer of the breast: what is the optimal treatment? A report and review of outcomes. Clin Breast Cancer. 2012; 12:287–292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Neuroendocrine Carcinoma of the Breast: A Case Report and Literature Review
- Primary Neuroendocrine Carcinoma in the Breast: A Case Report
- Small-cell neuroendocrine carcinoma of the breast
- Primary Breast Carcinoma with Neuroendocrine Features: Imaging Features on Mammography and Ultrasonography
- Primary Small Cell Neuroendocrine Carcinoma of the Breast: A Case Report With Literature Review