J Breast Cancer.
2015 Dec;18(4):356-364. 10.4048/jbc.2015.18.4.356.
Safety Results of Docetaxel-(Taxotere(R))-Based Chemotherapy in Early Breast Cancer Patients of Asia-Pacific Region: Asia-Pacific Breast Initiative II
- Affiliations
-
- 1Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sbkim3@amc.seoul.kr
- 2Clinical Oncology, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China.
- 3Medical Oncology, National Cancer Hospital, Hanoi, Vietnam.
- 4Division of Hematology/Oncology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
- 5Department of Breast Surgery, Shanghai Fudan University Cancer Hospital, Shanghai, China.
- KMID: 2176284
- DOI: http://doi.org/10.4048/jbc.2015.18.4.356
Abstract
- PURPOSE
The goal of this registry was to collect patient characteristics and safety data from patients from the Asia-Pacific region with early breast cancer receiving adjuvant chemotherapy containing docetaxel (Taxotere(R)).
METHODS
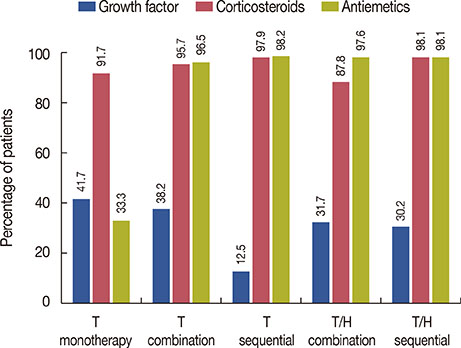
This registry was open-label, international, longitudinal, multicenter, and observational in design and included a prospective group of consecutive early breast cancer patients with an intermediate-to-high risk of recurrence being treated with various docetaxel-based (anthracycline and non-anthracycline) adjuvant chemotherapy regimens during 2009-2013 in real-world clinical settings.
RESULTS
The analysis included 1,712 patients, 79% of whom received docetaxel-based, anthracycline-containing regimens, while 21% received non-anthracycline-containing regimens. Patients receiving adjuvant docetaxel-based chemotherapy were followed for 1.5 years. Chemotherapy-related adverse events (AEs) were reported by 76.2% of patients (anthracycline-containing vs. non-anthracycline-containing regimens: 76.8% vs. 74.1%). Serious AEs were reported in 12% of patients (12.3% vs. 10%). National Cancer Institute Common Terminology Criteria for Adverse Events grade 3 or higher neutropenia was reported in 20% of patients (21.6% vs. 13.9%), leukopenia in 7.4% of patients (5.4% vs. 14.8%), and vomiting in 1.6% of patients (1.8% vs. 0.6%). Treatment-related death was reported in 27 patients (1.6%), while only 3% of patients had a relapse. Low-density lipoprotein cholesterol/high-density lipoprotein cholesterol (HDL-C) and total cholesterol/HDL-C ratios increased after chemotherapy. A clinically insignificant reduction of 1.9% in left ventricular ejection fraction, from 66.43 to 64.53, was observed 1.5 years after therapy was completed.
CONCLUSION
The Asia-Pacific Breast initiative II registry identified a variety of important facts regarding patient population characteristics, disease epidemiology and treatment response for early breast cancer patients of the Asia-Pacific region receiving docetaxel-based chemotherapy. Docetaxel-based chemotherapy did not show any significant safety concerns for early breast cancer patients of the Asia-Pacific region, and thus may represent a safe adjuvant chemotherapy regimen for these patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Akram M, Siddiqui SA. Breast cancer management: past, present and evolving. Indian J Cancer. 2012; 49:277–282.
Article2. de Boer RH, Chan A, Tran B, Wilcken N. Use of non-anthracycline regimens in early stage breast cancer in Australia. Asia Pac J Clin Oncol. 2011; 7:4–10.
Article3. Jensen BV, Skovsgaard T, Nielsen SL. Functional monitoring of anthracycline cardiotoxicity: a prospective, blinded, long-term observational study of outcome in 120 patients. Ann Oncol. 2002; 13:699–709.
Article4. Crown J, O'Leary M, Ooi WS. Docetaxel and paclitaxel in the treatment of breast cancer: a review of clinical experience. Oncologist. 2004; 9:Suppl 2. 24–32.
Article5. Martin M, Pienkowski T, Mackey J, Pawlicki M, Guastalla JP, Weaver C, et al. Adjuvant docetaxel for node-positive breast cancer. N Engl J Med. 2005; 352:2302–2313.
Article6. Pant S, Chilukuri MP, Ramaswamy B. Docetaxel for the post-surgery treatment of patients with node-positive breast cancer. Ther Clin Risk Manag. 2008; 4:419–424.7. Alken S, Kelly CM. Benefit risk assessment and update on the use of docetaxel in the management of breast cancer. Cancer Manag Res. 2013; 5:357–365.8. Youlden DR, Cramb SM, Yip CH, Baade PD. Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Biol Med. 2014; 11:101–115.9. Green M, Raina V. Epidemiology, screening and diagnosis of breast cancer in the Asia-Pacific region: current perspectives and important considerations. Asia Pac J Clin Oncol. 2008; 4:Suppl 3. S5–S13.
Article10. Singh JC, Jhaveri K, Esteva FJ. HER2-positive advanced breast cancer: optimizing patient outcomes and opportunities for drug development. Br J Cancer. 2014; 111:1888–1898.
Article11. Jones SE, Savin MA, Holmes FA, O'Shaughnessy JA, Blum JL, Vukelja S, et al. Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol. 2006; 24:5381–5387.
Article12. Eiermann W, Pienkowski T, Crown J, Sadeghi S, Martin M, Chan A, et al. Phase III study of doxorubicin/cyclophosphamide with concomitant versus sequential docetaxel as adjuvant treatment in patients with human epidermal growth factor receptor 2-normal, node-positive breast cancer: BCIRG-005 trial. J Clin Oncol. 2011; 29:3877–3884.
Article13. Volkova M, Russell R 3rd. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Curr Cardiol Rev. 2011; 7:214–220.
Article14. Alexopoulos CG, Pournaras S, Vaslamatzis M, Avgerinos A, Raptis S. Changes in serum lipids and lipoproteins in cancer patients during chemotherapy. Cancer Chemother Pharmacol. 1992; 30:412–416.
Article