Chonnam Med J.
2012 Aug;48(2):96-102. 10.4068/cmj.2012.48.2.96.
Effects on Intubating Conditions of Pretreatment with Remifentanil before Administration of Cisatracurium
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea. shkwak@jnu.ac.kr
- KMID: 2172210
- DOI: http://doi.org/10.4068/cmj.2012.48.2.96
Abstract
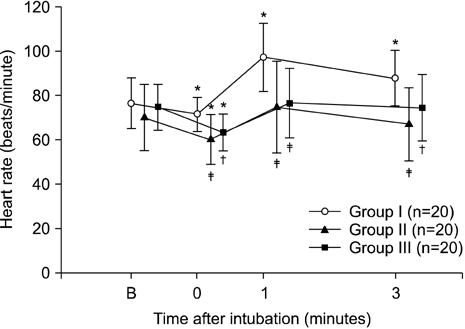
- Cisatracurium provides superior hemodynamic stability with only minor release of histamine, and its metabolism via Hoffman elimination is independent of organ function. However, use of cisatracurium is limited because of reportedly slower onset and unsatisfactory intubating conditions. Many studies have shown that remifentanil might provide reliable intubating conditions; thus, we hypothesized that pretreatment with remifentanil before administration of cisatracurium might result in acceptable intubating conditions. Sixty healthy patients scheduled for elective surgery were enrolled and randomly divided into three groups: saline (Group I, n=20), remifentanil 0.5 microg/kg (Group II, n=20), and remifentanil 1.0 microg/kg (Group III, n=20). The anesthesia was induced with propofol 2.0 microg/kg given intravenously over 30 s followed by injection over 30 s of a different dose of remifentanil according to the study protocol. We examined the intubating condition by jaw relaxation, vocal cord state, and diaphragmatic response 90 s after administering cisatracurium. We also measured mean blood pressure, heart rate, and the onset time, which is the interval from the end of neuromuscular blocking agent administration until suppression of maximal T1 on a train-of four sequence. The mean values of the intubating condition after endotracheal intubation in Groups II and III were significantly lower than that in Group I (p<0.005), although the overall onset time of cisatracurium did not differ significantly between the three groups. Our results suggest that supplementation with remifentanil in an induction regimen with cisatracurium improves the quality of the intubating condition even though the onset time of cisatracurium is not shortened.
MeSH Terms
Figure
Reference
-
1. Sluga M, Ummenhofer W, Studer W, Siegemund M, Marsch SC. Rocuronium versus succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. Anesth Analg. 2005. 101:1356–1361.
Article2. Kleinman W NG, Nitti JT, Raya J. Morgan GE MM, Murray MJ, editors. Neuromuscular blocking agents. Clinical anesthesilogy. 2006. 4th ed. New York: Lange Medical Books;205.3. Mellinghoff H, Radbruch L, Diefenbach C, Buzello W. A comparison of cisatracurium and atracurium: onset of neuromuscular block after bolus injection and recovery after subsequent infusion. Anesth Analg. 1996. 83:1072–1075.4. Wastila WB, Maehr RB, Turner GL, Hill DA, Savarese JJ. Comparative pharmacology of cisatracurium (51W89), atracurium, and five isomers in cats. Anesthesiology. 1996. 85:169–177.
Article5. Canfell PC, Castagnoli N Jr, Fahey MR, Hennis PJ, Miller RD. The metabolic disposition of laudanosine in dog, rabbit, and man. Drug Metab Dispos. 1986. 14:703–708.6. Parker CJ, Hunter JM. Pharmacokinetics of atracurium and laudanosine in patients with hepatic cirrhosis. Br J Anaesth. 1989. 62:177–183.
Article7. Kisor DF, Schmith VD, Wargin WA, Lien CA, Ornstein E, Cook DR. Importance of the organ-independent elimination of cisatracurium. Anesth Analg. 1996. 83:1065–1071.
Article8. Correa CM, Sudo GZ, Sudo RT. Hemodynamic effects of atracurium and cisatracurium and the use of diphenhydramine and cimetidine. Rev Bras Anestesiol. 2010. 60:52–63.
Article9. Kirov K, Motamed C, Decailliot F, Behforouz N, Duvaldestin P. Comparison of the neuromuscular blocking effect of cisatracurium and atracurium on the larynx and the adductor pollicis. Acta Anaesthesiol Scand. 2004. 48:577–581.
Article10. Lighthall GK, Jamieson MA, Katolik J, Brock-Utne JG. A comparison of the onset and clinical duration of high doses of cisatracurium and rocuronium. J Clin Anesth. 1999. 11:220–225.
Article11. Schwarz S, Ilias W, Lackner F, Mayrhofer O, Foldes FF. Rapid tracheal intubation with vecuronium: the priming principle. Anesthesiology. 1985. 62:388–391.12. Mirakhur RK, Lavery GG, Gibson FM, Clarke RS. Intubating conditions after vecuronium and atracurium given in divided doses (the priming technique). Acta Anaesthesiol Scand. 1986. 30:347–350.
Article13. Albert F, Hans P, Bitar Y, Brichant JF, Dewandre PY, Lamy M. Effects of ephedrine on the onset time of neuromuscular block and intubating conditions after cisatracurium: preliminary results. Acta Anaesthesiol Belg. 2000. 51:167–171.14. Leykin Y, Pellis T, Lucca M, Gullo A. Effects of ephedrine on intubating conditions following priming with rocuronium. Acta Anaesthesiol Scand. 2005. 49:792–797.
Article15. Tan CH, Onisong MK, Chiu WK. The influence of induction technique on intubating conditions 1 min after rocuronium administration: a comparison of a propofol-ephedrine combination and propofol. Anaesthesia. 2002. 57:223–226.
Article16. Klemola UM, Mennander S, Saarnivaara L. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand. 2000. 44:465–469.
Article17. Stevens JB, Wheatley L. Tracheal intubation in ambulatory surgery patients: using remifentanil and propofol without muscle relaxants. Anesth Analg. 1998. 86:45–49.18. Taha S, Siddik-Sayyid S, Alameddine M, Wakim C, Dahabra C, Moussa A, et al. Propofol is superior to thiopental for intubation without muscle relaxants. Can J Anaesth. 2005. 52:249–253.
Article19. Ross AK, Davis PJ, Dear Gd GL, Ginsberg B, McGowan FX, Stiller RD, et al. Pharmacokinetics of remifentanil in anesthetized pediatric patients undergoing elective surgery or diagnostic procedures. Anesth Analg. 2001. 93:1393–1401.
Article20. Plaud B, Debaene B, Donati F. The corrugator supercilii, not the orbicularis oculi, reflects rocuronium neuromuscular blockade at the laryngeal adductor muscles. Anesthesiology. 2001. 95:96–101.
Article21. Cooper R, Mirakhur RK, Clarke RS, Boules Z. Comparison of intubating conditions after administration of Org 9246 (rocuronium) and suxamethonium. Br J Anaesth. 1992. 69:269–273.
Article22. Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008. (2):CD002788.
Article23. Khuenl-Brady K, Castagnoli KP, Canfell PC, Caldwell JE, Agoston S, Miller RD. The neuromuscular blocking effects and pharmacokinetics of ORG 9426 and ORG 9616 in the cat. Anesthesiology. 1990. 72:669–674.
Article24. Robertson EN, Driessen JJ, Booij LH. Pharmacokinetics and pharmacodynamics of rocuronium in patients with and without renal failure. Eur J Anaesthesiol. 2005. 22:4–10.
Article25. van Miert MM, Eastwood NB, Boyd AH, Parker CJ, Hunter JM. The pharmacokinetics and pharmacodynamics of rocuronium in patients with hepatic cirrhosis. Br J Clin Pharmacol. 1997. 44:139–144.
Article26. Amin AM, Mohammad MY, Ibrahim MF. Comparative study of neuromuscular blocking and hemodynamic effects of rocuronium and cisatracurium under sevoflurane or total intravenous anesthesia. Middle East J Anesthesiol. 2009. 20:39–51.27. Lin SP, Chang KY, Chen YJ, Lin SM, Chang WK, Chan KH, et al. Priming with rocuronium to accelerate the onset time of cisatracurium during intubation. J Chin Med Assoc. 2009. 72:15–19.
Article28. Bluestein LS, Stinson LW Jr, Lennon RL, Quessy SN, Wilson RM. Evaluation of cisatracurium, a new neuromuscular blocking agent, for tracheal intubation. Can J Anaesth. 1996. 43:925–931.
Article29. Belmont MR, Lien CA, Quessy S, Abou-Donia MM, Abalos A, Eppich L, et al. The clinical neuromuscular pharmacology of 51W89 in patients receiving nitrous oxide/opioid/barbiturate anesthesia. Anesthesiology. 1995. 82:1139–1145.
Article30. Mandal P. Intubating conditions after cisatracurium administration: a dose response study in adults. J Anaesth Clin Pharmacol. 2002. 18:147.31. Egan TD, Minto CF, Hermann DJ, Barr J, Muir KT, Shafer SL. Remifentanil versus alfentanil: comparative pharmacokinetics and pharmacodynamics in healthy adult male volunteers. Anesthesiology. 1996. 84:821–833.32. Klemola UM, Mennander S, Saarnivaara L. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand. 2000. 44:465–469.
Article33. Cha JW, Kwak SH, Kim SJ, Choi JI, Kim CM, Jeong ST, et al. Optimal dose of remifentanil to blunt hemodynamic response to laryngoscopy and endotracheal intubation during induction of anesthesia with propofol. Korean J Anesthesiol. 2006. 51:292–296.
Article34. Lee JR, Jung CW, Lee JH, Choi IY, Seo KS, Kim HK, et al. Optimal dose of remifentanil to suppress cardiovascular responses to laryngoscopic endotracheal intubation. Korean J Anesthesiol. 2005. 49:780–785.
Article35. McAtamney D, O'Hare R, Hughes D, Carabine U, Mirakhur R. Evaluation of remifentanil for control of haemodynamic response to tracheal intubation. Anaesthesia. 1998. 53:1223–1227.
Article36. Thompson JP, Rowbotham DJ. Remifentanil-an opioid for the 21st century. Br J Anaesth. 1996. 76:341–343.
Article37. McKeating K, Bali IM, Dundee JW. The effects of thiopentone and propofol on upper airway integrity. Anaesthesia. 1988. 43:638–640.
Article38. Barker P, Langton JA, Wilson IG, Smith G. Movements of the vocal cords on induction of anaesthesia with thiopentone or propofol. Br J Anaesth. 1992. 69:23–25.
Article39. Eames WO, Rooke GA, Wu RS, Bishop MJ. Comparison of the effects of etomidate, propofol, and thiopental on respiratory resistance after tracheal intubation. Anesthesiology. 1996. 84:1307–1311.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The dose effect of ephedrine on the onset time and intubating conditions after cisatracurium administration
- Anesthesiologist's satisfaction using between cisatracurium and rocuronium for the intubation in the anesthesia induced by remifentanil and propofol
- The effect of low dose ketamine and priming of cisatracurium on the intubating condition and onset time of cisatracurium
- Comparison of etomidate and propofol on intubating conditions and the onset time associated with cisatracurium administration
- Tracheal Intubation without the Use of Muscle Relaxants: Remifentanil in Combination with Propofol