Endocrinol Metab.
2011 Dec;26(4):297-302. 10.3803/EnM.2011.26.4.297.
Association between Serum Thyroid Stimulating Hormone Level and Papillary Thyroid Microcarcinoma in Korean Euthyroid Patients
- Affiliations
-
- 1Haedong Internal Medicine Clinic, Daegu, Korea.
- 2Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. jed15@cu.ac.kr
- 3Department of Pathology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2169259
- DOI: http://doi.org/10.3803/EnM.2011.26.4.297
Abstract
- BACKGROUND
Thyroid cancer is a common disease and its prevalence is increasing. Recent reports have shown that an elevated thyrotropin (thyroid stimulating hormone, TSH) level is associated with thyroid cancer risk. However, the association between TSH level and thyroid cancer risk is not yet known for euthyroid patients diagnosed with papillary thyroid microcarcinoma (PTMC).
METHODS
Our study included 425 patients who underwent thyroid surgery and were diagnosed with PTMC between 2008 and 2009. Control group patients were diagnosed with benign nodules < or = 1 cm in size by US-guided fine needle aspiration. Nodules with one or more suspected malignant-ultrasonographic feature(s) were excluded from this study. Patients who were not euthyroid or who took thyroid medication were also excluded.
RESULTS
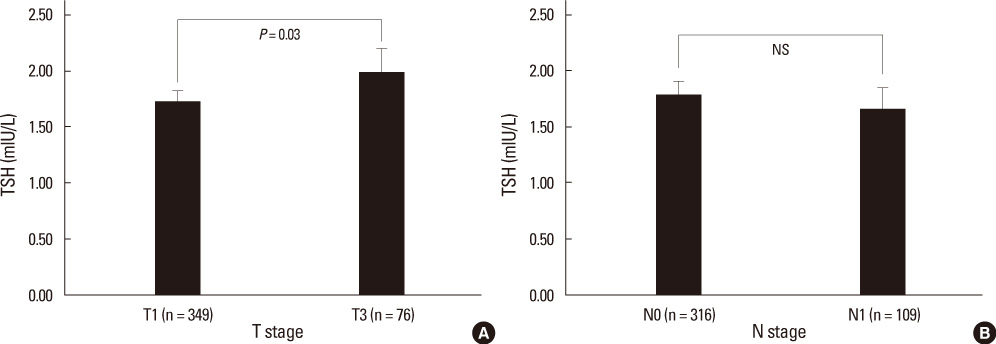
The mean age of all patients was 48.5 +/- 11.0 years and 88.8% were women. The mean age of those with PTMC was significantly lower than that of the control group. The mean TSH level was 1.78 +/- 0.93 mIU/L, and the mean free T4 level was 15.96 +/- 2.32 pmol/L. There was no difference in TSH level between the PTMC and control groups (1.77 +/- 0.93 mIU/L vs. 1.79 +/- 0.91 mIU/L, P = 0.829). After adjusting for age, TSH level was not correlated with tumor size (r = 0.02, P = 0.678) in the PTMC group. Moreover, the TSH level did not differ between patients with stage I and stage III-IV carcinoma (stage I, 1.77 +/- 0.95 mIU/L; stage III-IV, 1.79 +/- 0.87 mIU/L; P = 0.856).
CONCLUSION
TSH levels are not elevated in euthyroid PTMC patients. Thus, further evaluation is needed before serum TSH can be used as a tumor marker for small nodules < or = 1 cm in size in euthyroid patients.
MeSH Terms
Figure
Reference
-
1. Sherman SI. Thyroid carcinoma. Lancet. 2003. 361:501–511.2. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006. 295:2164–2167.3. Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989. 63:908–911.4. Yamamoto Y, Maeda T, Izumi K, Otsuka H. Occult papillary carcinoma of the thyroid. A study of 408 autopsy cases. Cancer. 1990. 65:1173–1179.5. Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg. 2008. 32:747–753.6. Strate SM, Lee EL, Childers JH. Occult papillary carcinoma of the thyroid with distant metastases. Cancer. 1984. 54:1093–1100.7. Kim TY, Hong SJ, Kim JM, Gu Kim W, Gong G, Ryu JS, Kim WB, Yun SC, Shong YK. Prognostic parameters for recurrence of papillary thyroid microcarcinoma. BMC Cancer. 2008. 8:296.8. Choi YJ, Park YL, Koh JH. Prevalence of thyroid cancer at a medical screening center: pathological features of screen-detected thyroid carcinomas. Yonsei Med J. 2008. 49:748–756.9. Lim AK, Daykin J, Holder R, Sheppard MC, Franklyn JA. Measurement of serum TSH in the investigation of patients presenting with thyroid enlargement. QJM. 1998. 91:687–689.10. Boelaert K, Horacek J, Holder RL, Watkinson JC, Sheppard MC, Franklyn JA. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab. 2006. 91:4295–4301.11. Jonklaas J, Nsouli-Maktabi H, Soldin SJ. Endogenous thyrotropin and triiodothyronine concentrations in individuals with thyroid cancer. Thyroid. 2008. 18:943–952.12. Fiore E, Rago T, Provenzale MA, Scutari M, Ugolini C, Basolo F, Di Coscio G, Berti P, Grasso L, Elisei R, Pinchera A, Vitti P. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer. 2009. 16:1251–1260.13. Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, Chen H. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab. 2008. 93:809–814.14. Gerschpacher M, Göbl C, Anderwald C, Gessl A, Krebs M. Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid. 2010. 20:389–392.15. Patel SG, Shah JP. TNM staging of cancers of the head and neck: striving for uniformity among diversity. CA Cancer J Clin. 2005. 55:242–258.16. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.17. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994. 97:418–428.18. Sipos JA, Mazzaferri EL. The therapeutic management of differentiated thyroid cancer. Expert Opin Pharmacother. 2008. 9:2627–2637.19. Biondi B, Filetti S, Schlumberger M. Thyroid-hormone therapy and thyroid cancer: a reassessment. Nat Clin Pract Endocrinol Metab. 2005. 1:32–40.20. Derwahl M, Broecker M, Kraiem Z. Clinical review 101: thyrotropin may not be the dominant growth factor in benign and malignant thyroid tumors. J Clin Endocrinol Metab. 1999. 84:829–834.21. Shi Y, Zou M, Farid NR. Expression of thyrotrophin receptor gene in thyroid carcinoma is associated with a good prognosis. Clin Endocrinol (Oxf). 1993. 39:269–274.22. Yoshihara A, Noh JY, Ohye H, Sato S, Sekiya K, Kosuga Y, Suzuki M, Matsumoto M, Kunii Y, Watanabe N, Mukasa K, Ito K, Ito K. Reference limits for serum thyrotropin in a Japanese population. Endocr J. 2011. 58:585–588.23. Papini E, Petrucci L, Guglielmi R, Panunzi C, Rinaldi R, Bacci V, Crescenzi A, Nardi F, Fabbrini R, Pacella CM. Long-term changes in nodular goiter: a 5-year prospective randomized trial of levothyroxine suppressive therapy for benign cold thyroid nodules. J Clin Endocrinol Metab. 1998. 83:780–783.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ectopic Thyroid Papillary Carcinoma with Incidental Papillary Thyroid Microcarcinoma
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma
- Risk Factors for Hypothyroidism after Thyroid Lobectomy with Papillary Thyroid Crcinoma according to Existence of Thyroiditis
- Clinical implications of preoperative thyrotropin serum concentrations in patients who underwent thyroidectomy for nonfunctioning nodule(s)
- Relationship between Serum TSH Level within the Normal Reference Range and the Metabolic Syndrome