Ann Rehabil Med.
2013 Apr;37(2):269-273. 10.5535/arm.2013.37.2.269.
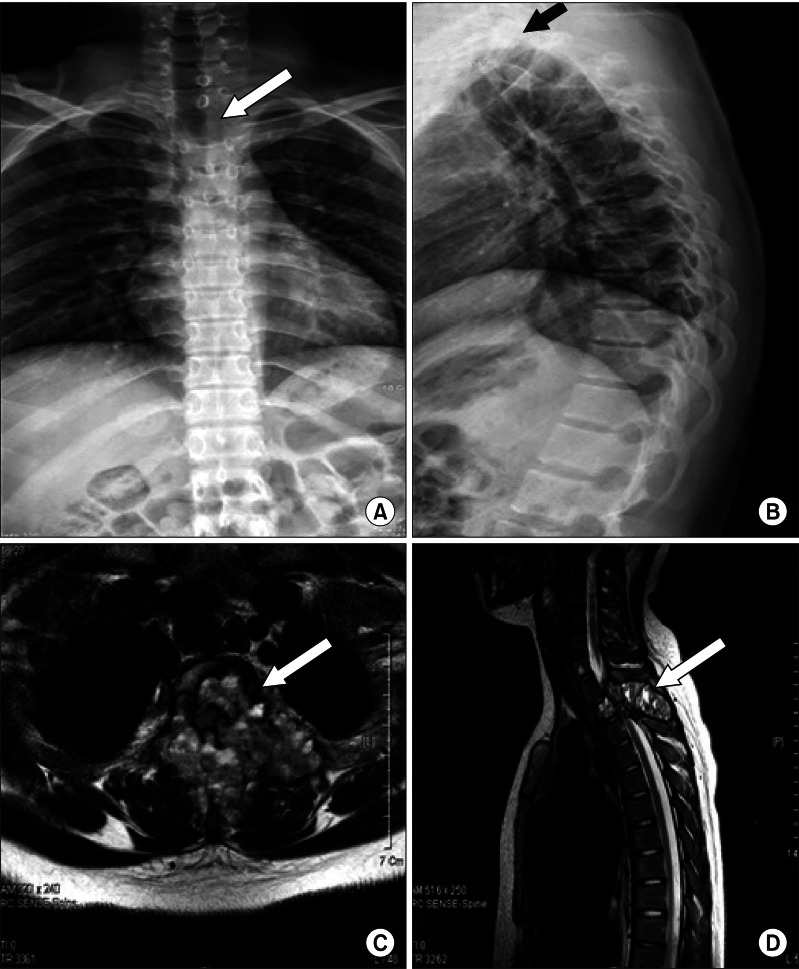
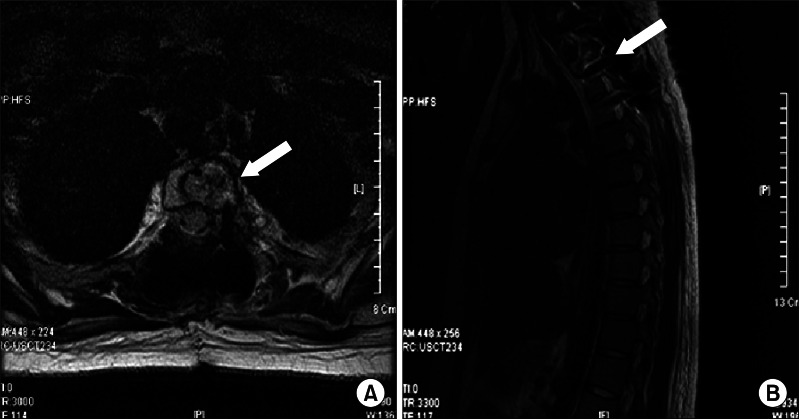
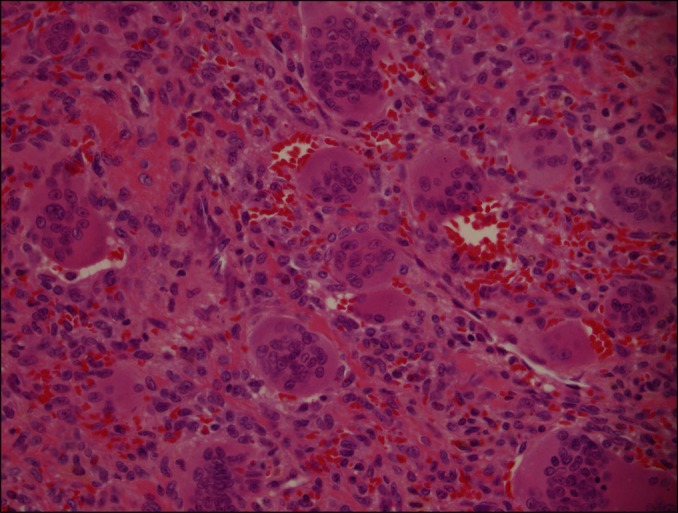
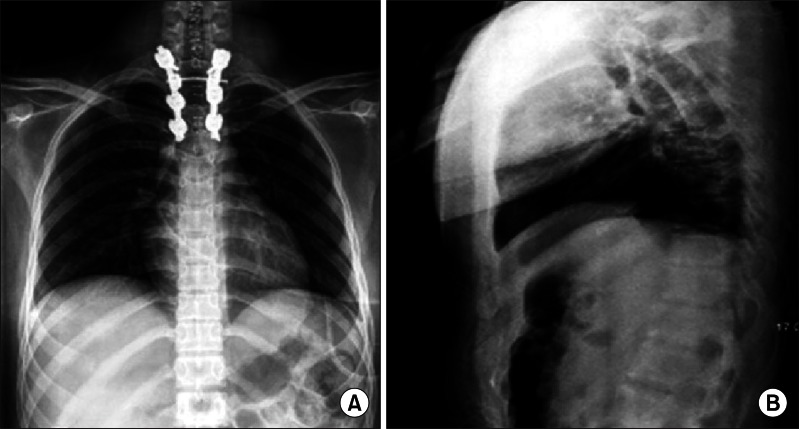
Spinal Cord Injury due to the Giant Cell Tumor of the Second Thoracic Vertebra: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Kyung Hee University College of Medicine, Seoul, Korea. grace2010@hanmail.net
- 2Department of Pathology, Kyung Hee University College of Medicine, Seoul, Korea.
- KMID: 2165781
- DOI: http://doi.org/10.5535/arm.2013.37.2.269
Abstract
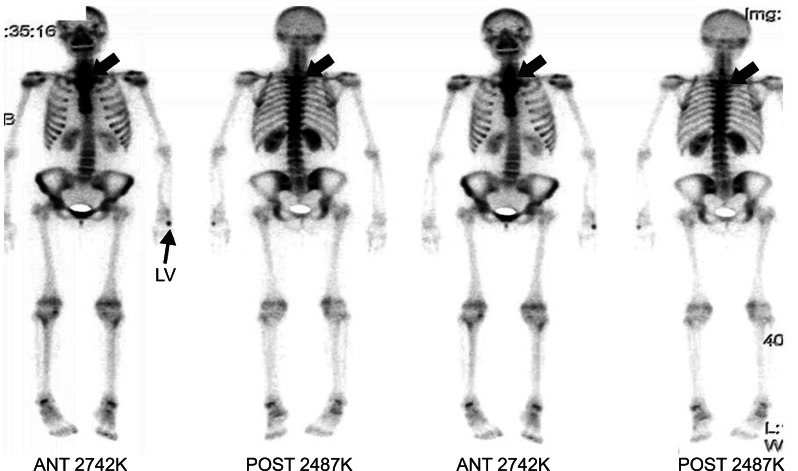
- Giant cell tumor (GCT) is a relatively rare neoplasm. In GCT, the bone affection of the axial skeleton is extremely rare. Most GCT arises in the meta-epiphyseal ends of the long bones. Its peak incidence is between 30 to 40 years of age. GCT is usually classified as benign, but shows locally aggressive behavior and may occasionally undergo a malignant transformation. The patients with GCT in the spine often complain of the lower back pains, as the tumors primarily involve the sacrum. We report a case of an adolescent female complaining of the upper back pain with a sudden weakness of the lower extremities, later diagnosed with the GCT of the T2 vertebra. The present patient showed American Spinal Injury Association Impairment Scale (AIS) D before the surgery, which changed to AIS E after the treatments including the surgery, radiation therapy and rehabilitation.
Keyword
MeSH Terms
Figure
Reference
-
1. Hunter CL, Pacione D, Hornyak M, Murali R. Giant-cell tumors of the cervical spine: case report. Neurosurgery. 2006; 59:E1142–E1143. PMID: 17143206.2. Sanjay BK, Sim FH, Unni KK, McLeod RA, Klassen RA. Giant-cell tumours of the spine. J Bone Joint Surg Br. 1993; 75:148–154. PMID: 8421014.
Article3. Balke M, Henrichs MP, Gosheger G, Ahrens H, Streitbuerger A, Koehler M, et al. Giant cell tumors of the axial skeleton. Sarcoma. 2012; 2012:410973. PMID: 22448122.
Article4. Refai D, Dunn GP, Santiago P. Giant cell tumor of the thoracic spine: case report and review of the literature. Surg Neurol. 2009; 71:228–233. PMID: 18207522.
Article5. Mendenhall WM, Zlotecki RA, Scarborough MT, Gibbs CP, Mendenhall NP. Giant cell tumor of bone. Am J Clin Oncol. 2006; 29:96–99. PMID: 16462511.
Article6. Terry RY, Lindsay JR. Terry RY, Lindsay JR, editors. Tumors and tumor-like processes. Essentials of skeletal radiology. 2005. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;p. 1224.8. Martin C, McCarthy EF. Giant cell tumor of the sacrum and spine: series of 23 cases and a review of the literature. Iowa Orthop J. 2010; 30:69–75. PMID: 21045974.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Herniation of the Thoracic Spinal Cord: A Case Report
- Metastatic Thoracic Intramedullary Small Cell Carcinoma: Case Report
- A Giant Cell Tumor of the Lumbar Vertebra: One Case Report
- Trachea, Esophagus, and Spinal Cord Injury Caused by Stab Wound: A case report
- Total Spondylectomy of a Lumber Vertebra with Giant Cell Tumor: One Case Report