Ann Rehabil Med.
2015 Dec;39(6):922-930. 10.5535/arm.2015.39.6.922.
Can MRI Findings Help to Predict Neurological Recovery in Paraplegics With Thoracolumbar Fracture?
- Affiliations
-
- 1Department of Rehabilitation Medicine, Konkuk University School of Medicine and Konkuk University Medical Center, Seoul, Korea. mdlis@nate.com
- KMID: 2165618
- DOI: http://doi.org/10.5535/arm.2015.39.6.922
Abstract
OBJECTIVE
To evaluate the usefulness of various magnetic resonance imaging (MRI) findings in the prognosis of neurological recovery in paraplegics with thoracolumbar fracture using association analysis with clinical outcomes and electrodiagnostic features.
METHODS
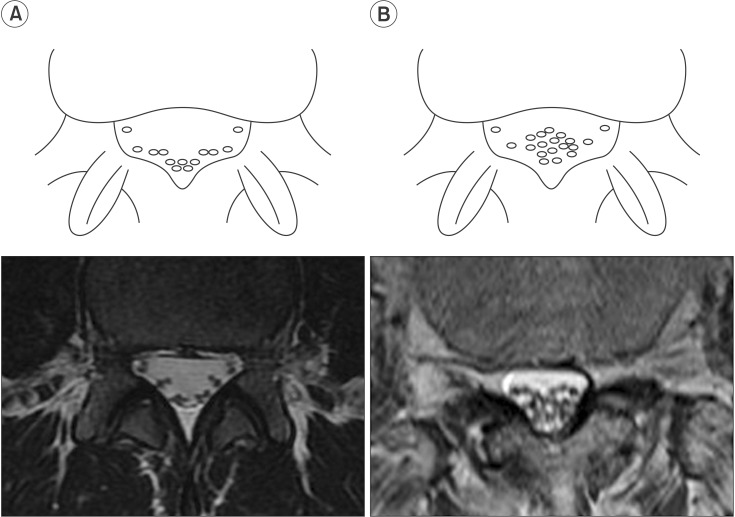
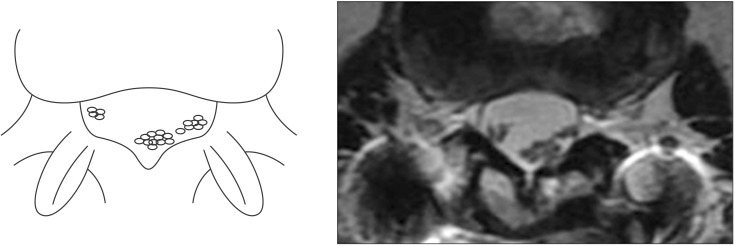
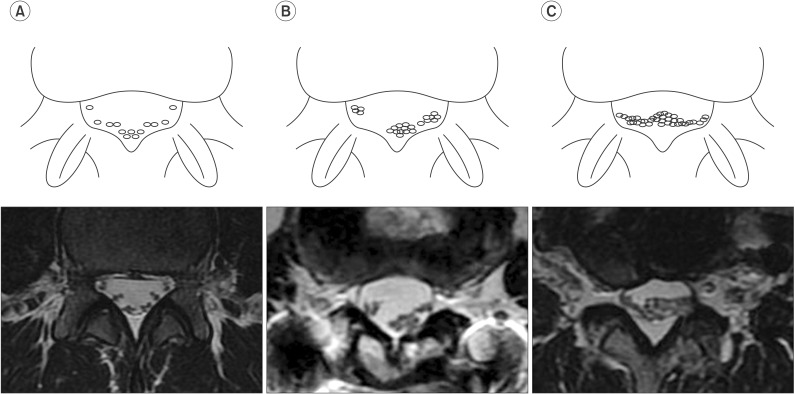
This retrospective study involved 30 patients treated for paraplegia following thoracolumbar fracture. On axial and sagittal T2-weighted MRI scans, nerve root sedimentation sign, root aggregation sign, and signal intensity changes in the conus medullaris were independently assessed by two raters. A positive sedimentation sign was defined as the absence of nerve root sedimentation. The root aggregation sign was defined as the presence of root aggregation in at least one axial MRI scan. Clinical outcomes including the American Spinal Injury Association impairment scale, ambulatory capacity, and electrodiagnostic features were used for association analysis.
RESULTS
Inter-rater reliability of the nerve root sedimentation sign and the root aggregation sign were kappa=0.67 (p=0.001) and kappa=0.78 (p<0.001), respectively. A positive sedimentation sign was significantly associated with recovery of ambulatory capacity after a rehabilitation program (chi2=4.854, p=0.028). The presence of the root aggregation sign was associated with reduced compound muscle action potential amplitude of common peroneal and tibial nerves in nerve conduction studies (chi2=5.026, p=0.025).
CONCLUSION
A positive sedimentation sign was significantly associated with recovery of ambulatory capacity and not indicative of persistent paralysis. The root aggregation sign suggested the existence of significant cauda equina injuries.
MeSH Terms
Figure
Reference
-
1. Prabhakar MM, Rao BS, Patel L. Thoracolumbar burst fracture with complete paraplegia: rationale for second-stage anterior decompression and fusion regarding functional outcome. J Orthop Traumatol. 2009; 10:83–90. PMID: 19468683.
Article2. Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation for thoracolumbar fractures. J Am Acad Orthop Surg. 2004; 12:424–435. PMID: 15615508.
Article3. Kirkpatrick AW, McKevitt E. Thoracolumbar spine fractures: is there a problem? Can J Surg. 2002; 45:21–24. PMID: 11837916.4. Kingwell SP, Curt A, Dvorak MF. Factors affecting neurological outcome in traumatic conus medullaris and cauda equina injuries. Neurosurg Focus. 2008; 25:E7. PMID: 18980481.
Article5. Holmes JF, Miller PQ, Panacek EA, Lin S, Horne NS, Mower WR. Epidemiology of thoracolumbar spine injury in blunt trauma. Acad Emerg Med. 2001; 8:866–872. PMID: 11535478.
Article6. Malas MA, Salbacak A, Buyukmumcu M, Seker M, Koyluoglu B, Karabulut AK. An investigation of the conus medullaris termination level during the period of fetal development to adulthood. Kaibogaku Zasshi. 2001; 76:453–459. PMID: 11729672.7. Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medicolegal position. Eur Spine J. 2011; 20:690–697. PMID: 21193933.
Article8. Tomkins-Lane CC, Quint DJ, Gabriel S, Melloh M, Haig AJ. Nerve root sedimentation sign for the diagnosis of lumbar spinal stenosis: reliability, sensitivity, and specificity. Spine (Phila Pa 1976). 2013; 38:E1554–E1560. PMID: 23970109.9. Macedo LG, Wang Y, Battie MC. The sedimentation sign for differential diagnosis of lumbar spinal stenosis. Spine (Phila Pa 1976). 2013; 38:827–831. PMID: 23197008.
Article10. Staub LP, Barz T, Melloh M, Lord SJ, Chatfield M, Bossuyt PM. Clinical validation study to measure the performance of the Nerve Root Sedimentation Sign for the diagnosis of lumbar spinal stenosis. Contemp Clin Trials. 2011; 32:470–474. PMID: 21300180.
Article11. Barz T, Staub LP, Melloh M, Hamann G, Lord SJ, Chatfield MD, et al. Clinical validity of the nerve root sedimentation sign in patients with suspected lumbar spinal stenosis. Spine J. 2014; 14:667–674. PMID: 24055611.
Article12. Barz T, Melloh M, Staub LP, Lord SJ, Lange J, Roder CP, et al. Nerve root sedimentation sign: evaluation of a new radiological sign in lumbar spinal stenosis. Spine (Phila Pa 1976). 2010; 35:892–897. PMID: 20308945.13. Barz T, Melloh M, Staub LP, Lord SJ, Lange J, Merk HR. Increased intraoperative epidural pressure in lumbar spinal stenosis patients with a positive nerve root sedimentation sign. Eur Spine J. 2014; 23:985–990. PMID: 24166020.
Article14. Takahashi M, Sakamoto Y, Miyawaki M, Bussaka H. Increased MR signal intensity secondary to chronic cervical cord compression. Neuroradiology. 1987; 29:550–556. PMID: 3124018.
Article15. Mehalic TF, Pezzuti RT, Applebaum BI. Magnetic resonance imaging and cervical spondylotic myelopathy. Neurosurgery. 1990; 26:217–227. PMID: 2308669.
Article16. Matsuda Y, Miyazaki K, Tada K, Yasuda A, Nakayama T, Murakami H, et al. Increased MR signal intensity due to cervical myelopathy: analysis of 29 surgical cases. J Neurosurg. 1991; 74:887–892. PMID: 1903439.17. Al-Mefty O, Harkey LH, Middleton TH, Smith RR, Fox JL. Myelopathic cervical spondylotic lesions demonstrated by magnetic resonance imaging. J Neurosurg. 1988; 68:217–222. PMID: 3339437.
Article18. Okada Y, Ikata T, Yamada H, Sakamoto R, Katoh S. Magnetic resonance imaging study on the results of surgery for cervical compression myelopathy. Spine (Phila Pa 1976). 1993; 18:2024–2029. PMID: 8272953.
Article19. Wada E, Yonenobu K, Suzuki S, Kanazawa A, Ochi T. Can intramedullary signal change on magnetic resonance imaging predict surgical outcome in cervical spondylotic myelopathy? Spine (Phila Pa 1976). 1999; 24:455–462. PMID: 10084183.
Article20. Curt A, Dietz V. Ambulatory capacity in spinal cord injury: significance of somatosensory evoked potentials and ASIA protocol in predicting outcome. Arch Phys Med Rehabil. 1997; 78:39–43. PMID: 9014955.
Article21. Crozier KS, Cheng LL, Graziani V, Zorn G, Herbison G, Ditunno JF Jr. Spinal cord injury: prognosis for ambulation based on quadriceps recovery. Paraplegia. 1992; 30:762–767. PMID: 1484726.
Article22. Hussey RW, Stauffer ES. Spinal cord injury: requirements for ambulation. Arch Phys Med Rehabil. 1973; 54:544–547. PMID: 4759444.23. Court-Brown CM, McQueen MM, Tornetta P. Trauma. Philadelphia: Lippincott Williams & Wilkins;2006. p. 226–227.24. Kostuik JP, Harrington I, Alexander D, Rand W, Evans D. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986; 68:386–391. PMID: 2936744.
Article25. Curt A, Dietz V. Nerve conduction study in cervical spinal cord injury: significance for hand function. NeuroRehabilitation. 1996; 7:165–173. PMID: 24525886.
Article26. Chiodo A, Haig AJ, Yamakawa KS, Quint D, Tong H, Choksi VR. Magnetic resonance imaging vs. electrodiagnostic root compromise in lumbar spinal stenosis: a masked controlled study. Am J Phys Med Rehabil. 2008; 87:789–797. PMID: 18806507.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Study of Radiologic Changes after Conservative Treatment in Compression fracture and Stable Bursting Fracture of Thoracolumbar Spine
- A Clinical Study of Fractures and Fracture - Dislocations of the Thoracolumbar Spine Injuries
- MRI Findings of Posterior Ligament Complex Injury in Thorcolumbar Bursting Fractures
- Surgical Results of Stabilization of the Thoracolumbar Spine Fracture with the Internal Skeletal Fixation System
- Surgical Planning for Thoracolumar Spine Fracture