J Korean Med Sci.
2015 Aug;30(8):1017-1024. 10.3346/jkms.2015.30.8.1017.
Interaction Effect between Weight Perception and Comorbidities on Weight Control Behavior in Overweight and Obese Adults: Is There a Sex Difference?
- Affiliations
-
- 1Department of Preventive Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. parksw@cu.ac.kr
- 2Department of Preventive Medicine, School of Medicine, Kyungpook National University, Daegu, Korea.
- KMID: 2164494
- DOI: http://doi.org/10.3346/jkms.2015.30.8.1017
Abstract
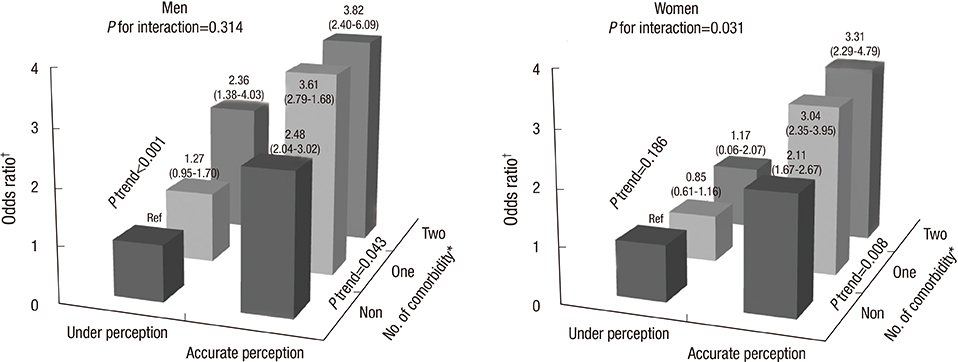
- We investigated the interaction effect between body weight perception and chronic disease comorbidities on body weight control behavior in overweight/obese Korean adults. We analyzed data from 9,138 overweight/obese adults > or =20 yr of age from a nationally representative cross-sectional survey. Multiple logistic regression using an interaction model was performed to estimate the effect of chronic disease comorbidities on weight control behavior regarding weight perception. Adjusted odds ratios for weight control behavior tended to increase significantly with an increasing number of comorbidities in men regardless of weight perception (P<0.05 for trend), suggesting no interaction. Unlike women who perceived their weight accurately, women who under-perceived their weight did not show significant improvements in weight control behavior even with an increasing number of comorbidities. Thus, a significant interaction between weight perception and comorbidities was found only in women (P=0.031 for interaction). The effect of the relationship between accurate weight perception and chronic disease comorbidities on weight control behavior varied by sex. Improving awareness of body image is particularly necessary for overweight and obese women to prevent complications.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
*Body Image
Body Mass Index
Comorbidity
Educational Status
Female
Health Behavior
Humans
Male
Middle Aged
Obesity/*epidemiology/*prevention & control
Patient Compliance/*statistics & numerical data
Prevalence
Republic of Korea/epidemiology
Risk Factors
Sex Characteristics
Sex Distribution
Smoking/epidemiology
Socioeconomic Factors
Treatment Outcome
*Weight Perception
Weight Reduction Programs/*utilization
Young Adult
Figure
Cited by 1 articles
-
Relationships between Obesity, Body Image Perception, and Weight Control in Adult Women
Hyunju Chae
Korean J Women Health Nurs. 2019;25(2):129-142. doi: 10.4069/kjwhn.2019.25.2.129.
Reference
-
1. Haslam DW, James WP. Obesity. Lancet. 2005; 366:1197–1209.2. Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Arterioscler Thromb Vasc Biol. 2006; 26:968–976.3. World Health Organization. Global health risks mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization;2009.4. Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011; 12:131–141.5. Kim DM, Ahn CW, Nam SY. Prevalence of obesity in Korea. Obes Rev. 2005; 6:117–121.6. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2011: Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Korean Ministry of Health and Welfare;2012.7. Korea Centers for Disease Control and Prevention. Epidemiology and management of cardiocerebrovascular disease. Osong, Korea: Korea Centers for Disease Control and Prevention;2013.8. Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997-2007. Korean Circ J. 2009; 39:467–476.9. Shin MH, Oh HK, Ahn YO. Ten year trend of cancer incidence in Seoul, Korea: 1993--2002. J Prev Med Public Health. 2008; 41:92–99.10. Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord. 1992; 16:397–415.11. Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989; 105:260–275.12. Yoo S, Cho HJ, Khang YH. General and abdominal obesity in South Korea, 1998-2007: gender and socioeconomic differences. Prev Med. 2010; 51:460–465.13. Joh HK, Oh J, Lee HJ, Kawachi I. Gender and socioeconomic status in relation to weight perception and weight control behavior in Korean adults. Obes Facts. 2013; 6:17–27.14. Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. Int J Obes (Lond). 2011; 35:1063–1070.15. Anderson LA, Eyler AA, Galuska DA, Brown DR, Brownson RC. Relationship of satisfaction with body size and trying to lose weight in a national survey of overweight and obese women aged 40 and older, United States. Prev Med. 2002; 35:390–396.16. Lemon SC, Rosal MC, Zapka J, Borg A, Andersen V. Contributions of weight perceptions to weight loss attempts: differences by body mass index and gender. Body Image. 2009; 6:90–96.17. Gregory CO, Blanck HM, Gillespie C, Maynard LM, Serdula MK. Perceived health risk of excess body weight among overweight and obese men and women: differences by sex. Prev Med. 2008; 47:46–52.18. Duncan DT, Wolin KY, Scharoun-Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011; 8:20.19. Kim DS, Kim HS, Cho Y, Cho SI. The effects of actual and perceived body weight on unhealthy weight control behaviors and depressed mood among adult women in Seoul, Korea. J Prev Med Public Health. 2008; 41:323–330.20. Jones M, Grilo CM, Masheb RM, White MA. Psychological and behavioral correlates of excess weight: misperception of obese status among persons with Class II obesity. Int J Eat Disord. 2010; 43:628–632.21. Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self-perception of weight in overweight adolescents. Pediatrics. 2010; 125:e452–e458.22. Skinner AC, Weinberger M, Mulvaney S, Schlundt D, Rothman RL. Accuracy of perceptions of overweight and relation to self-care behaviors among adolescents with type 2 diabetes and their parents. Diabetes Care. 2008; 31:227–229.23. Forman MR, Trowbridge FL, Gentry EM, Marks JS, Hogelin GC. Overweight adults in the United States: the behavioral risk factor surveys. Am J Clin Nutr. 1986; 44:410–416.24. Zhao G, Ford ES, Li C, Mokdad AH. Compliance with physical activity recommendations in US adults with diabetes. Diabet Med. 2008; 25:221–227.25. Grace SL, Barry-Bianchi S, Stewart DE, Rukholm E, Nolan RP. Physical activity behavior, motivational readiness and self-efficacy among Ontarians with cardiovascular disease and diabetes. J Behav Med. 2007; 30:21–29.26. Zhao G, Ford ES, Li C, Mokdad AH. Weight control behaviors in overweight/obese U.S. adults with diagnosed hypertension and diabetes. Cardiovasc Diabetol. 2009; 8:13.27. World Health Organization Western Pacific Region. International Association for the Study of Obesity. International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney, Australia: Health Communications Australia Pty;2000.28. Yost J, Krainovich-Miller B, Budin W, Norman R. Assessing weight perception accuracy to promote weight loss among U.S. female adolescents: a secondary analysis. BMC Public Health. 2010; 10:465.29. Green KL, Cameron R, Polivy J, Cooper K, Liu L, Leiter L, Heatherton T. Weight dissatisfaction and weight loss attempts among Canadian adults. Canadian Heart Health Surveys Research Group. CMAJ. 1997; 157:S17–S25.30. O'Brien K, Venn BJ, Perry T, Green TJ, Aitken W, Bradshaw A, Thomson R. Reasons for wanting to lose weight: different strokes for different folks. Eat Behav. 2007; 8:132–135.31. Statistics Korea. Annual report on the causes of death statistics by provinces. Daejeon, Korea: Statistics Korea;2014.32. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010; 303:2043–2050.33. Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010; 140:226–235.34. Ferrara A, Mangione CM, Kim C, Marrero DG, Curb D, Stevens M, Selby JV. Translating Research Into Action for Diabetes Study Group. Sex disparities in control and treatment of modifiable cardiovascular disease risk factors among patients with diabetes: Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care. 2008; 31:69–74.35. Cheng S, Claggett B, Correia AW, Shah AM, Gupta DK, Skali H, Ni H, Rosamond WD, Heiss G, Folsom AR, et al. Temporal trends in the population attributable risk for cardiovascular disease: the Atherosclerosis Risk in Communities Study. Circulation. 2014; 130:820–828.36. Cachelin FM, Rebeck RM, Chung GH, Pelayo E. Does ethnicity influence body-size preference? A comparison of body image and body size. Obes Res. 2002; 10:158–166.37. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.38. Chen Y, Copeland WK, Vedanthan R, Grant E, Lee JE, Gu D, Gupta PC, Ramadas K, Inoue M, Tsugane S, et al. Association between body mass index and cardiovascular disease mortality in east Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. BMJ. 2013; 347:f5446.39. Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, Kim EM, Suh SH, Shin HJ, Lee KR, et al. 2014 clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab (Seoul). 2014; 29:405–409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Parental Control Over Their Child's Weight among Elementary School Children Being Overweight or Obese
- Body Mass Index and Weight Loss in Overweight and Obese Korean Women: The Mediating Role of Body Weight Perception
- Gender Differences in the Effects of Weight, Weight Perception, and Weight Satisfaction on Depression in Adolescents
- A Study on the Effect of Adult Female's Personality Type on Health Control Behavior and Obesity Stress
- Factors Associated with Distorted Self-perception of Body Weight in Korean Adults