Korean J Urol.
2015 Aug;56(8):565-571. 10.4111/kju.2015.56.8.565.
Clinical features and prognosis of prostate cancer with high-grade prostatic intraepithelial neoplasia
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cskim@amc.seoul.kr
- 2Department of Urology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2164407
- DOI: http://doi.org/10.4111/kju.2015.56.8.565
Abstract
- PURPOSE
To evaluate the clinical features and biochemical recurrence (BCR) in prostate cancer (PCa) with high-grade prostatic intraepithelial neoplasia (HGPIN).
MATERIALS AND METHODS
We retrospectively analyzed the medical records of 893 patients who underwent a radical prostatectomy for PCa between 2011 and 2012 at Asan Medical Center; 752 of these patients who did not receive neoadjuvant or adjuvant therapy and were followed up for more than 1 year were included. The cohort was divided into two groups-patients with and without HGPIN-and their characteristics were compared. The Cox proportional hazards model was used to analyze factors affecting BCR.
RESULTS
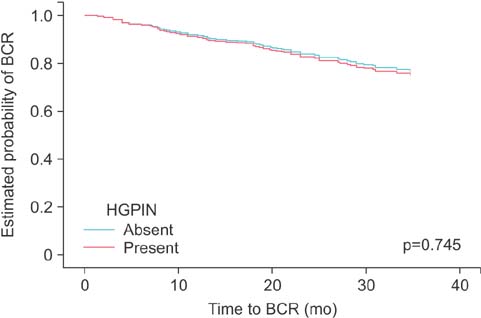
In total, 652 study patients (86.7%) had HGPIN. There were no significant differences in preoperative factors between the two groups, including age (p=0.369) and preoperative prostate-specific antigen concentration (p=0.234). Patients with HGPIN had a higher Gleason score (p=0.012), more frequent multiple tumor (p=0.013), and more perineural invasion (p=0.012), but no other postoperative pathologic characteristics were significantly different between the two groups. There were no significant differences in BCR (13.0% vs. 11.5%, p=0.665) and HGPIN was not associated with BCR (p=0.745). In multivariate analysis, only the T stage (p<0.001) was associated with BCR.
CONCLUSIONS
PCa patients with HGPIN have a higher Gleason score, more frequent multiple tumors, and more perineural invasion than those without HGPIN. The presence of HGPIN is not an independent predictor of BCR.
MeSH Terms
Figure
Reference
-
1. Bostwick DG, Brawer MK. Prostatic intra-epithelial neoplasia and early invasion in prostate cancer. Cancer. 1987; 59:788–794.2. Haggman MJ, Macoska JA, Wojno KJ, Oesterling JE. The relationship between prostatic intraepithelial neoplasia and prostate cancer: critical issues. J Urol. 1997; 158:12–22.3. Epstein JI, Herawi M. Prostate needle biopsies containing prostatic intraepithelial neoplasia or atypical foci suspicious for carcinoma: implications for patient care. J Urol. 2006; 175(3 Pt 1):820–834.4. Herawi M, Kahane H, Cavallo C, Epstein JI. Risk of prostate cancer on first re-biopsy within 1 year following a diagnosis of high grade prostatic intraepithelial neoplasia is related to the number of cores sampled. J Urol. 2006; 175:121–124.5. Al-Hussain TO, Epstein JI. Initial high-grade prostatic intraepithelial neoplasia with carcinoma on subsequent prostate needle biopsy: findings at radical prostatectomy. Am J Surg Pathol. 2011; 35:1165–1167.6. Pietzak EJ 3rd, Kabarriti AE, Mucksavage P, Bavaria T, Van Arsdalen K, Malkowicz SB, et al. The presence of high-grade prostatic intraepithelial neoplasia or atypia on prostate biopsy does not adversely affect prostatectomy outcomes for patients otherwise eligible for active surveillance. Urology. 2014; 84:1442–1447.7. Casey RG, Catto JW, Cheng L, Cookson MS, Herr H, Shariat S, et al. Diagnosis and management of urothelial carcinoma in situ of the lower urinary tract: a systematic review. Eur Urol. 2015; 67:876–888.8. Horst KC, Smitt MC, Goffinet DR, Carlson RW. Predictors of local recurrence after breast-conservation therapy. Clin Breast Cancer. 2005; 5:425–438.9. WHO Guidelines for treatment of cervical intraepithelial neoplasia 2-3 and adenocarcinoma in situ: cryotherapy, large loop excision of the transformation zone, and cold knife conization. Geneva: World Health Organization;2014.10. Moore CK, Karikehalli S, Nazeer T, Fisher HA, Kaufman RP Jr, Mian BM. Prognostic significance of high grade prostatic intraepithelial neoplasia and atypical small acinar proliferation in the contemporary era. J Urol. 2005; 173:70–72.11. Thompson IM Jr, Leach R. Prostate cancer and prostatic intraepithelial neoplasia: true, true, and unrelated? J Clin Oncol. 2013; 31:515–516.12. Humphrey PA. High grade prostatic intraepithelial neoplasia in prostate needle biopsy. J Urol. 2013; 189:315–316.13. Gallo F, Chiono L, Gastaldi E, Venturino E, Giberti C. Prognostic significance of high-grade prostatic intraepithelial neoplasia (HGPIN): risk of prostatic cancer on repeat biopsies. Urology. 2008; 72:628–632.14. Pierorazio PM, Lambert SM, Matsukhani M, Sprenkle PC, McCann TR, Katz AE, et al. High-grade prostatic intraepithelial neoplasia is an independent predictor of outcome after radical prostatectomy. BJU Int. 2007; 100:1066–1070.15. Jung JH, Lee JW, Arkoncel FR, Cho NH, Yusoff NA, Kim KJ, et al. Significance of perineural invasion, lymphovascular invasion, and high-grade prostatic intraepithelial neoplasia in robot-assisted laparoscopic radical prostatectomy. Ann Surg Oncol. 2011; 18:3828–3832.16. Ingels A, Ploussard G, Allory Y, Abbou C, de la Taille A, Salomon L. Concomitant high-grade prostatic intraepithelial neoplasia is associated with good prognosis factors and oncologic outcome after radical prostatectomy. Urol Int. 2014; 92:264–269.17. López JI. Prostate adenocarcinoma detected after high-grade prostatic intraepithelial neoplasia or atypical small acinar proliferation. BJU Int. 2007; 100:1272–1276.18. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.19. Epstein JI, Srigley J, Grignon D, Humphrey P. Association of Directors of Anatomic and Surgical Pathology. Recommendations for the reporting of prostate carcinoma: Association of Directors of Anatomic and Surgical Pathology. Am J Clin Pathol. 2008; 129:24–30.20. Recommendations for the reporting of resected prostate carcinomas. Association of Directors of Anatomic and Surgical Pathology Agency. Pathol Int. 1997; 47:268–271.21. Srigley JR, Amin MB, Epstein JI, Grignon DJ, Humphrey PA, Renshaw AA, et al. Updated protocol for the examination of specimens from patients with carcinomas of the prostate gland. Arch Pathol Lab Med. 2006; 130:936–946.22. Bostwick DG, Liu L, Brawer MK, Qian J. High-grade prostatic intraepithelial neoplasia. Rev Urol. 2004; 6:171–179.23. McNeal JE, Bostwick DG. Intraductal dysplasia: a premalignant lesion of the prostate. Hum Pathol. 1986; 17:64–71.24. Qian J, Wollan P, Bostwick DG. The extent and multicentricity of high-grade prostatic intraepithelial neoplasia in clinically localized prostatic adenocarcinoma. Hum Pathol. 1997; 28:143–148.25. Auskalnis S, Milonas D, Jievaltas M, Vaiciunas K, Mickevicius A, Gudinaviciene I. The role of high-grade prostatic intraepithelial neoplasia for biochemical relapse of prostate carcinoma after radical prostatectomy. Medicina (Kaunas). 2010; 46:604–610.26. Sfoungaristos S, Perimenis P. Implication of high grade intraepithelial neoplasia in adverse pathology after radical prostatectomy. Prague Med Rep. 2012; 113:156–165.27. Masterson TA, Cheng L, Mehan RM, Koch MO. Tumor focality does not predict biochemical recurrence after radical prostatectomy in men with clinically localized prostate cancer. J Urol. 2011; 186:506–510.28. Iremashvili V, Pelaez L, Manoharan M, Acosta K, Rosenberg DL, Soloway MS. Tumor focality is not associated with biochemical outcome after radical prostatectomy. Prostate. 2012; 72:762–768.29. Tollefson MK, Karnes RJ, Kwon ED, Lohse CM, Rangel LJ, Mynderse LA, et al. Prostate cancer Ki-67 (MIB-1) expression, perineural invasion, and gleason score as biopsy-based predictors of prostate cancer mortality: the Mayo model. Mayo Clin Proc. 2014; 89:308–318.30. Lee JT, Lee S, Yun CJ, Jeon BJ, Kim JM, Ha HK, et al. Prediction of perineural invasion and its prognostic value in patients with prostate cancer. Korean J Urol. 2010; 51:745–751.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High-Grade Prostatic Intraepithelial Neoplasia
- Significance of Atypical Small Acinar Proliferation and High-Grade Prostatic Intraepithelial Neoplasia in Prostate Biopsy
- Clinical significance of prostatic intraepithelial neoplasia
- Expression of Prostatic Carcinoma Oncogene PTI - 1 in Prostatic Carcinoma , Prostatic Intraepithelial Neoplasia and Benign Prostatic Hyperplasia Using in situ PCR
- Relationship of Prostate Specific Antigen & Prostate Specific Antigen Density and Prostatic Intraepithelial Neoplasia in Patient with Benign Prostatic Hyperplasia and Prostatic Cancer