Hip Pelvis.
2016 Mar;28(1):24-28. 10.5371/hp.2016.28.1.24.
Total Hip Arthroplasty in Patient with Aplastic Anemia
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yongsik@korea.com
- KMID: 2161311
- DOI: http://doi.org/10.5371/hp.2016.28.1.24
Abstract
- PURPOSE
Patients with aplastic anemia (AA) are now living longer and therefore are at increased risk for the development of osteonecrosis of the hip. However, studies on the results of total hip arthroplasty (THA) are lacking. The purpose of this study is to present the result of THA in patients with AA.
MATERIALS AND METHODS
We retrospectively reviewed the data for a group of 29 patients (45 hips) with AA who presented to our institution for THA between May 2008 and May 2012. All hips were replaced because of osteonecrosis of the femoral head. A specific prospective protocol was followed for the perioperative transfusion of platelets and blood. The clinical and radiographic evaluations were done, and the minimum follow-up period was 3 years (mean, 49.2 months; range, 36 to 84 months).
RESULTS
Three hips had excessive perioperative bleeding and hematoma formation, and then hematoma evacuations were done; one hip was finally revised because of infection of acetabular component. One patient with poorly controlled AA died due to delayed infection on the hip joint. All hips showed stable fixation, and the mean Harris hip score was improved from 54.2 points (range, 42 to 69 points) preoperatively to 90.8 points (range, 73 to 97 points) at the time of the latest follow-up.
CONCLUSION
In the present study, the durability of implant fixation was maintained and the clinical results demonstrated a sustained increase in function of the hip. Postoperatively, paying attention to bleeding and infection should be needed.
MeSH Terms
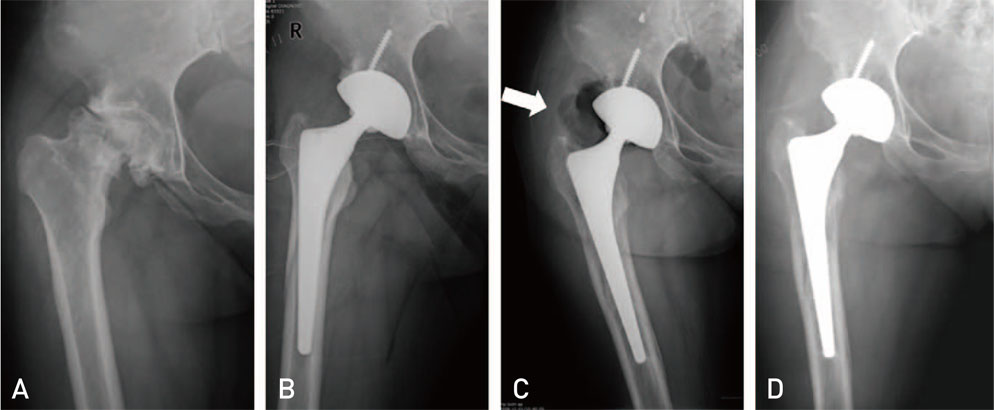
Figure
Reference
-
1. Ades L, Mary JY, Robin M, et al. Long-term outcome after bone marrow transplantation for severe aplastic anemia. Blood. 2004; 103:2490–2497.
Article2. Konopacki J, Porcher R, Robin M, et al. Long-term follow up after allogeneic stem cell transplantation in patients with severe aplastic anemia after cyclophosphamide plus antithymocyte globulin conditioning. Haematologica. 2012; 97:710–716.
Article3. Sharma S, Yang S, Rochester R, et al. Prevalence of osteonecrosis and associated risk factors in children before allogeneic BMT. Bone Marrow Transplant. 2011; 46:813–819.
Article4. Kim YS, Callaghan JJ, Kwon SY, Kim KW, Han CH, Woo YK. Arthroplasty of the hip in patients with aplastic anemia. J Bone Joint Surg Am. 2000; 82:1231–1239.
Article5. Torii Y, Hasegawa Y, Kubo T, et al. Osteonecrosis of the femoral head after allogeneic bone marrow transplantation. Clin Orthop Relat Res. 2001; (382):124–132.
Article6. Hahn JS, Chung KS, Lee SJ, et al. Surgical intervention in patients with aplastic anemia. Yonsei Med J. 1992; 33:173–182.
Article7. Kim YS, Kwon SY, Sun DH, Han SK, Maloney WJ. Modified posterior approach to total hip arthroplasty to enhance joint stability. Clin Orthop Relat Res. 2008; 466:294–299.
Article8. Harris WH. Preliminary report of results of Harris total hip replacement. Clin Orthop Relat Res. 1973; (95):168–173.
Article9. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.10. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69:45–55.
Article11. Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985; 67:1074–1085.
Article12. Dorr LD, Wan Z, Song M, Ranawat A. Bilateral total hip arthroplasty comparing hydroxyapatite coating to porouscoated fixation. J Arthroplasty. 1998; 13:729–736.
Article13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article14. Mollison PL, Engelfriet CP, Contreras M. The transfusion of platelets, leucocytes, and plasma components. In : Mollison PL, Engelfriet CP, Contreras M, editors. Blood transfusion in in clinical medicine. 9th ed. Boston: Blackwell Scientific;1993. p. 638–676.