Hip Pelvis.
2015 Dec;27(4):201-208. 10.5371/hp.2015.27.4.201.
Patient Blood Management in Hip Replacement Arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University Anam Hospital, Korea University School of Medicine, Seoul, Korea. oshan@korea.ac.kr
- KMID: 2150507
- DOI: http://doi.org/10.5371/hp.2015.27.4.201
Abstract
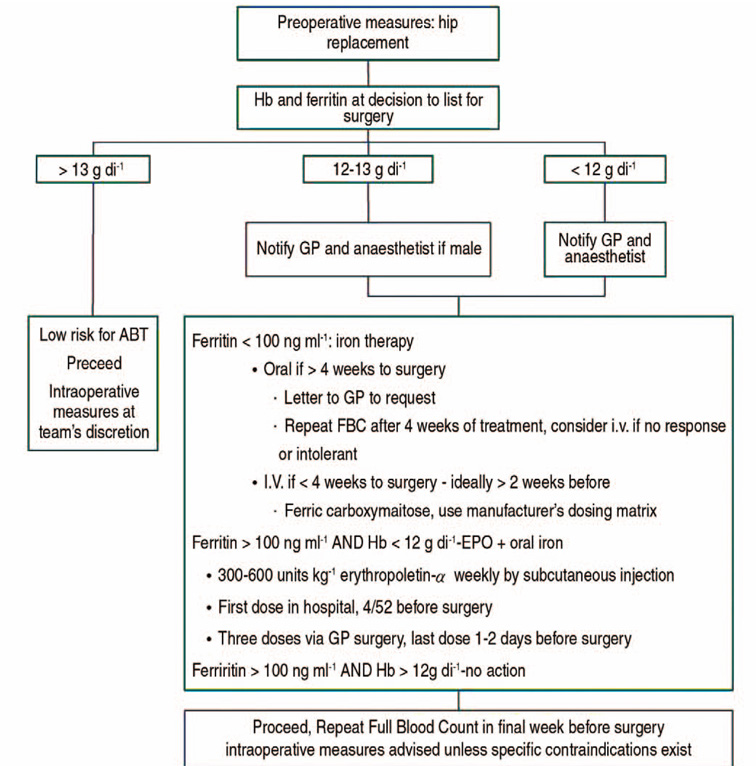
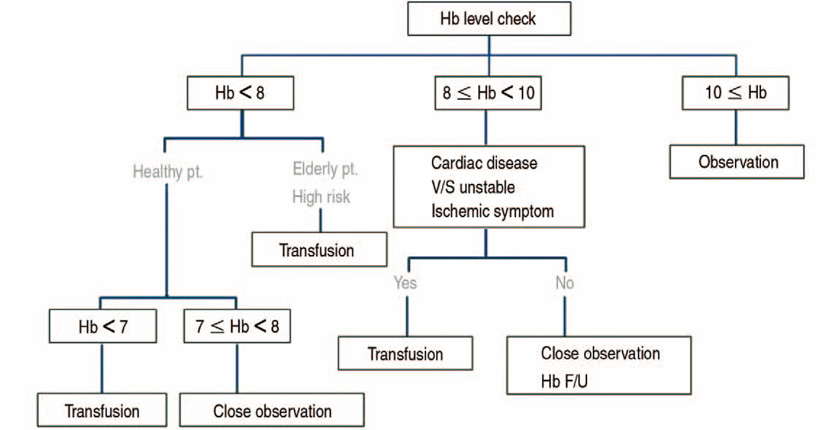
- Perioperative blood transfusions are common in total hip arthroplasty because of preoperative anemia and perioperative blood loss. Perioperative anemia and the need for allogeneic blood transfusion are related with increased morbidity. To reduce perioperative allogeneic blood transfusion, keeping the preoperative hemoglobin level above 12.0 g/dL is important in orthopedic patients. By using the anti-fibrinolytic agent or perioperative cell salvage, reduce intraoperative blood loss is very important for the reduction of perioperative blood loss. As a transfusion trigger, low hemoglobin is another important target to reduce the transfusion rate. Because blood management is closely connected with prognosis, it has become a new challenge in orthopedic surgery.
Figure
Cited by 1 articles
-
Preoperative Temporary Discontinuation of Aspirin Medication Does Not Increase the Allogeneic Transfusion Rate and Blood Loss in Primary Total Hip Arthroplasty
Myung-Rae Cho, Chung Mu Jun, Won-Kee Choi
Hip Pelvis. 2019;31(2):82-86. doi: 10.5371/hp.2019.31.2.82.
Reference
-
1. Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004; 86:561–565.2. Browne JA, Adib F, Brown TE, Novicoff WM. Transfusion rates are increasing following total hip arthroplasty: risk factors and outcomes. J Arthroplasty. 2013; 28:8 Suppl. 34–37.
Article3. Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med. 2004; 116:Suppl 7A. 58S–69S.
Article4. Karkouti K, Wijeysundera DN, Beattie WS. Reducing Bleeding in Cardiac Surgery (RBC) Investigators. Risk associated with preoperative anemia in cardiac surgery: a multicenter cohort study. Circulation. 2008; 117:478–484.
Article5. Beattie WS, Karkouti K, Wijeysundera DN, Tait G. Risk associated with preoperative anemia in noncardiac surgery: a single-center cohort study. Anesthesiology. 2009; 110:574–581.6. Blumberg N, Heal JM. Immunomodulation by blood transfusion: an evolving scientific and clinical challenge. Am J Med. 1996; 101:299–308.
Article7. Waymack JP, Gugliuzza K, Dong YL, Herndon DN. Effect of blood transfusion on immune function. IX. Effect on lymphocyte metabolism. J Surg Res. 1993; 55:269–272.8. Choat JD, Maitta RW, Tormey CA, et al. Transfusion reactions to blood and cell therapy products. In : Hoffman R, Benz EJ, Silberstein LE, Heslop HE, Weitz JI, editors. Hematology: basic principles and practice. Philadelphia, PA: Saunders/Elsevier;2013.9. Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res. 2002; 102:237–244.
Article10. Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008; 79:168–173.
Article11. Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008; 466:1710–1715.
Article12. Adams RC, Lundy JS. Anesthesia in cases of poor surgical risk: some suggestions for decreasing the risk. Anesthesiology. 1942; 9:603–607.13. Walsh M, Preston C, Bong M, Patel V, Di Cesare PE. Relative risk factors for requirement of blood transfusion after total hip arthroplasty. J Arthroplasty. 2007; 22:1162–1167.
Article14. Salido JA, Marín LA, Gómez LA, Zorrilla P, Martínez C. Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg Am. 2002; 84-A:216–220.15. Aderinto J, Brenkel IJ. Pre-operative predictors of the requirement for blood transfusion following total hip replacement. J Bone Joint Surg Br. 2004; 86:970–973.
Article16. Goodnough LT, Maniatis A, Earnshaw P, et al. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br J Anaesth. 2011; 106:13–22.
Article17. So-Osman C, Nelissen RG, Koopman-van Gemert AW, et al. Patient blood management in elective total hip- and knee-replacement surgery (Part 1): a randomized controlled trial on erythropoietin and blood salvage as transfusion alternatives using a restrictive transfusion policy in erythropoietin-eligible patients. Anesthesiology. 2014; 120:839–851.
Article18. Moonen AF, Thomassen BJ, Knoors NT, van Os JJ, Verburg AD, Pilot P. Pre-operative injections of epoetinalpha versus post-operative retransfusion of autologous shed blood in total hip and knee replacement: a prospective randomised clinical trial. J Bone Joint Surg Br. 2008; 90:1079–1083.19. Cuenca J, García-Erce JA, Martínez F, Cardona R, Pérez-Serrano L, Muñoz M. Preoperative haematinics and transfusion protocol reduce the need for transfusion after total knee replacement. Int J Surg. 2007; 5:89–94.
Article20. Yoo YC, Shim JK, Kim JC, Jo YY, Lee JH, Kwak YL. Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology. 2011; 115:929–937.
Article21. Na HS, Shin SY, Hwang JY, Jeon YT, Kim CS, Do SH. Effects of intravenous iron combined with low-dose recombinant human erythropoietin on transfusion requirements in iron-deficient patients undergoing bilateral total knee replacement arthroplasty. Transfusion. 2011; 51:118–124.
Article22. Kotzé A, Carter LA, Scally AJ. Effect of a patient blood management programme on preoperative anaemia, transfusion rate, and outcome after primary hip or knee arthroplasty: a quality improvement cycle. Br J Anaesth. 2012; 108:943–952.
Article23. Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A. Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet. 1996; 347:289–292.
Article24. Parker MJ, Livingstone V, Clifton R, McKee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007; (3):CD001825.
Article25. Slaughter TF, Greenberg CS. Antifibrinolytic drugs and perioperative hemostasis. Am J Hematol. 1997; 56:32–36.
Article26. Ho KM, Ismail H. Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: a meta-analysis. Anaesth Intensive Care. 2003; 31:529–537.
Article27. Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2012; 94:1153–1159.
Article28. Chang CH, Chang Y, Chen DW, Ueng SW, Lee MS. Topical tranexamic acid reduces blood loss and transfusion rates associated with primary total hip arthroplasty. Clin Orthop Relat Res. 2014; 472:1552–1557.
Article29. Selvaratnam V. Does pre-operative tranexamic acid increase the incidence of thromboembolism in primary lower limb arthroplasty? Open J Orthoped. 2013; 3:249–252.
Article30. Duncan CM, Gillette BP, Jacob AK, Sierra RJ, Sanchez-Sotelo J, Smith HM. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015; 30:272–276.
Article31. Kim TK, Chang CB, Koh IJ. Practical issues for the use of tranexamic acid in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014; 22:1849–1858.
Article32. Gill JB, Rosenstein A. The use of antifibrinolytic agents in total hip arthroplasty: a meta-analysis. J Arthroplasty. 2006; 21:869–873.33. Greenky M, Shaner J, Rasouli MR, Han SB, Parvizi J, Hozack WJ. Intraoperative blood salvage in revision total hip arthroplasty: who benefits most? J Arthroplasty. 2014; 29:1298–1300.
Article34. Amin A, Watson A, Mangwani J, Nawabi DH, Ahluwalia R, Loeffler M. A prospective randomised controlled trial of autologous retransfusion in total knee replacement. J Bone Joint Surg Br. 2008; 90:451–454.
Article35. Smith LK, Williams DH, Langkamer VG. Post-operative blood salvage with autologous retransfusion in primary total hip replacement. J Bone Joint Surg Br. 2007; 89:1092–1097.
Article36. Sinclair KC, Clarke HD, Noble BN. Blood management in total knee arthroplasty: a comparison of techniques. Orthopedics. 2009; 32:19.
Article37. Gonzalez-Porras JR, Colado E, Conde MP, Lopez T, Nieto MJ, Corral M. An individualized pre-operative blood saving protocol can increase pre-operative haemoglobin levels and reduce the need for transfusion in elective total hip or knee arthroplasty. Transfus Med. 2009; 19:35–42.
Article38. del Trujillo MM, Carrero A, Muñoz M. The utility of the perioperative autologous transfusion system OrthoPAT in total hip replacement surgery: a prospective study. Arch Orthop Trauma Surg. 2008; 128:1031–1038.
Article39. Moonen AF, Knoors NT, van Os JJ, Verburg AD, Pilot P. Retransfusion of filtered shed blood in primary total hip and knee arthroplasty: a prospective randomized clinical trial. Transfusion. 2007; 47:379–384.
Article40. Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999; 81:2–10.
Article41. Liu D, Dan M, Adivi N. Blood conservation strategies in total hip and knee arthroplasty. Reconstr Rev. 2014; 4:39.
Article