J Korean Med Sci.
2013 Jan;28(1):114-119. 10.3346/jkms.2013.28.1.114.
Prognostic Usefulness of Eosinopenia in the Pediatric Intensive Care Unit
- Affiliations
-
- 1Department of Pediatrics and Institute of Allergy, Severance Biomedical Science Institute, Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea. kwkim@yuhs.ac
- KMID: 2158010
- DOI: http://doi.org/10.3346/jkms.2013.28.1.114
Abstract
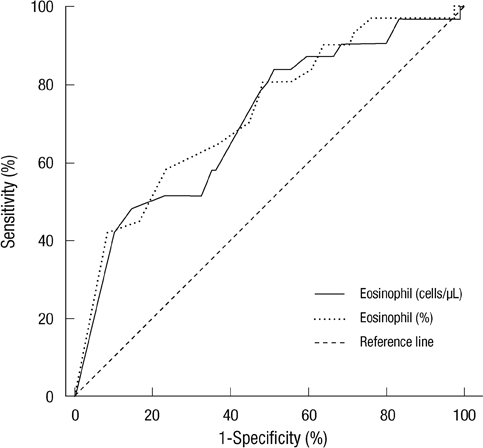
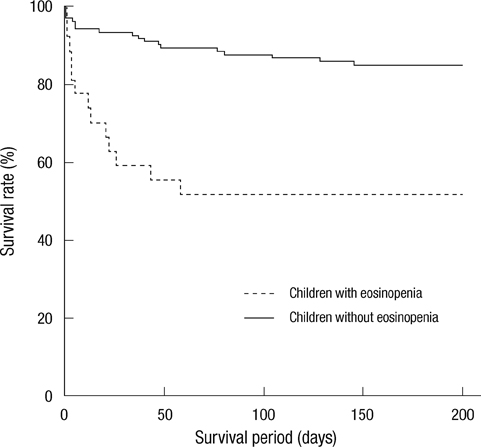
- Eosinopenia, a biomarker for infection, has recently been shown to be a predictor of adult mortality in the intensive care unit (ICU). Our study assessed the usefulness of eosinopenia as a mortality and an infection biomarker in the pediatric ICU (PICU). We compared the PICU mortality scores, eosinophil count and percentage at ICU admission between children who survived and those who did not survive and between children with infection and those without infection. A total of 150 patients were evaluated. The initial eosinophil count and percentage were significantly lower in the group that did not survive when compared to those that did survive (P < 0.001; P < 0.001). However, there was no significant difference in the eosinophil count and percentage seen in patients with and without infection. Eosinopenia, defined as an eosinophil count < 15 cells/microL and an eosinophil percentage < 0.25%, (hazard ratio [HR]: 2.96; P = 0.008) along with a Pediatric Index of Mortality (PIM) 2 (HR: 1.03; P = 0.004) were both determined to be independent predictors of mortality in the PICU. The presence of eosinopenia at the ICU admission can be a useful biomarker for mortality in children, but is not useful as a biomarker for infection.
Keyword
MeSH Terms
Figure
Reference
-
1. Kirkham FJ, Newton CR, Whitehouse W. Paediatric coma scales. Dev Med Child Neurol. 2008. 50:267–274.2. Lacroix J, Cotting J. Severity of illness and organ dysfunction scoring in children. Pediatr Crit Care Med. 2005. 6:S126–S134.3. Slater A, Shann F, Pearson G. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003. 29:278–285.4. Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med. 1996. 24:743–752.5. Leteurtre S, Duhamel A, Grandbastien B, Proulx F, Cotting J, Gottesman R, Joffe A, Wagner B, Hubert P, Martinot A, et al. Daily estimation of the severity of multiple organ dysfunction syndrome in critically ill children. CMAJ. 2010. 182:1181–1187.6. Hwang HS, Lee NY, Han SB, Kwak GY, Lee SY, Chung SY, Kang JH, Jeong DC. Performance effectiveness of pediatric index of mortality 2 (PIM2) and pediatric risk of mortality III (PRISM III) in pediatric patients with intensive care in single institution: Retrospective study. Korean J Pediatr. 2008. 51:1158–1164.7. Park BH, Park MS, Kim YS, Kim SK, Kang YA, Jung JY, Lim JE, Kim EY, Chang J. Prognostic utility of changes in N-terminal pro-brain natriuretic peptide combined with sequential organ failure assessment scores in patients with acute lung injury/acute respiratory distress syndrome concomitant with septic shock. Shock. 2011. 36:109–114.8. Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, Kim SJ, Lee KA. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012. 37:242–246.9. Schetz MR, Van den Berghe G. Do we have reliable biochemical markers to predict the outcome of critical illness? Int J Artif Organs. 2005. 28:1197–1210.10. Abidi K, Belayachi J, Derras Y, Khayari ME, Dendane T, Madani N, Khoudri I, Zeggwagh AA, Abouqal R. Eosinopenia, an early marker of increased mortality in critically ill medical patients. Intensive Care Med. 2011. 37:1136–1142.11. Merino CA, Martinez FT, Cardemil F, Rodriguez JR. Absolute eosinophils count as a marker of mortality in patients with severe sepsis and septic shock in an intensive care unit. J Crit Care. 2012. 27:394–399.12. Levinson AT, Casserly BP, Levy MM. Reducing mortality in severe sepsis and septic shock. Semin Respir Crit Care Med. 2011. 32:195–205.13. Bass DA, Gonwa TA, Szejda P, Cousart MS, DeChatelet LR, McCall CE. Eosinopenia of acute infection: Production of eosinopenia by chemotactic factors of acute inflammation. J Clin Invest. 1980. 65:1265–1271.14. Bass DA. Behavior of eosinophil leukocytes in acute inflammation. II. Eosinophil dynamics during acute inflammation. J Clin Invest. 1975. 56:870–879.15. Spreng M. Possible health effects of noise induced cortisol increase. Noise Health. 2000. 2:59–64.16. Holland M, Alkhalil M, Chandromouli S, Janjua A, Babores M. Eosinopenia as a marker of mortality and length of stay in patients admitted with exacerbations of chronic obstructive pulmonary disease. Respirology. 2010. 15:165–167.17. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005. 6:2–8.18. Krishnan J, Morrison W, Simone S, Ackerman A. Implications of thrombocytopenia and platelet course on pediatric intensive care unit outcomes. Pediatr Crit Care Med. 2008. 9:502–505.19. Ogura H, Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, Mayumi T, Murata A, Ikeda T, et al. SIRS-associated coagulopathy and organ dysfunction in critically ill patients with thrombocytopenia. Shock. 2007. 28:411–417.20. Gil H, Magy N, Mauny F, Dupond JL. Value of eosinopenia in inflammatory disorders: an "old" marker revisited. Rev Med Interne. 2003. 24:431–435.21. Lopez de Toro Martin Consuegra I, Sanchez Casado M, Rodriguez Villar S, Raigal Cano A, Lopez Reina Torrijos P, Velasco Ramos A, Sanchez Rodriguez P, Cabezas Martin H. Evaluation of eosinopenia as an infection marker in critical care patients. Med Intensiva. 2010. 34:246–253.22. Montesanti M, Testa G, Biagi C, Bartolini F. Pattern of circulating eosinophils in allergic children suffering from infectious disease. Minerva Pediatr. 1997. 49:187–191.23. Montesanti M, Testa G, Biagi C, Bartolini F. Trend of circulating eosinophils in healthy children and children suffering from infectious diseases. A retrospective study. Minerva Pediatr. 1997. 49:179–186.24. Wibrow BA, Ho KM, Flexman JP, Keil AD, Kohrs DL. Eosinopenia as a diagnostic marker of bloodstream infection in hospitalised paediatric and adult patients: a case-control study. Anaesth Intensive Care. 2011. 39:224–230.25. Abidi K, Khoudri I, Belayachi J, Madani N, Zekraoui A, Zeggwagh AA, Abouqal R. Eosinopenia is a reliable marker of sepsis on admission to medical intensive care units. Crit Care. 2008. 12:R59.26. Shaaban H, Daniel S, Sison R, Slim J, Perez G. Eosinopenia: Is it a good marker of sepsis in comparison to procalcitonin and C-reactive protein levels for patients admitted to a critical care unit in an urban hospital? J Crit Care. 2010. 25:570–575.27. Zahar JR, Timsit JF, Garrouste-Orgeas M, Francais A, Vesin A, Descorps-Declere A, Dubois Y, Souweine B, Haouache H, Goldgran-Toledano D. Outcomes in severe sepsis and patients with septic shock: pathogen species and infection sites are not associated with mortality. Crit Care Med. 2011. 39:1886–1895.