Ann Dermatol.
2011 May;23(2):177-184. 10.5021/ad.2011.23.2.177.
Epidemiologic Study of Malassezia Yeasts in Patients with Malassezia Folliculitis by 26S rDNA PCR-RFLP Analysis
- Affiliations
-
- 1Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea. 20050078@kuh.ac.kr
- KMID: 2156659
- DOI: http://doi.org/10.5021/ad.2011.23.2.177
Abstract
- BACKGROUND
So far, studies on the inter-relationship between Malassezia and Malassezia folliculitis have been rather scarce.
OBJECTIVE
We sought to analyze the differences in body sites, gender and age groups, and to determine whether there is a relationship between certain types of Malassezia species and Malassezia folliculitis.
METHODS
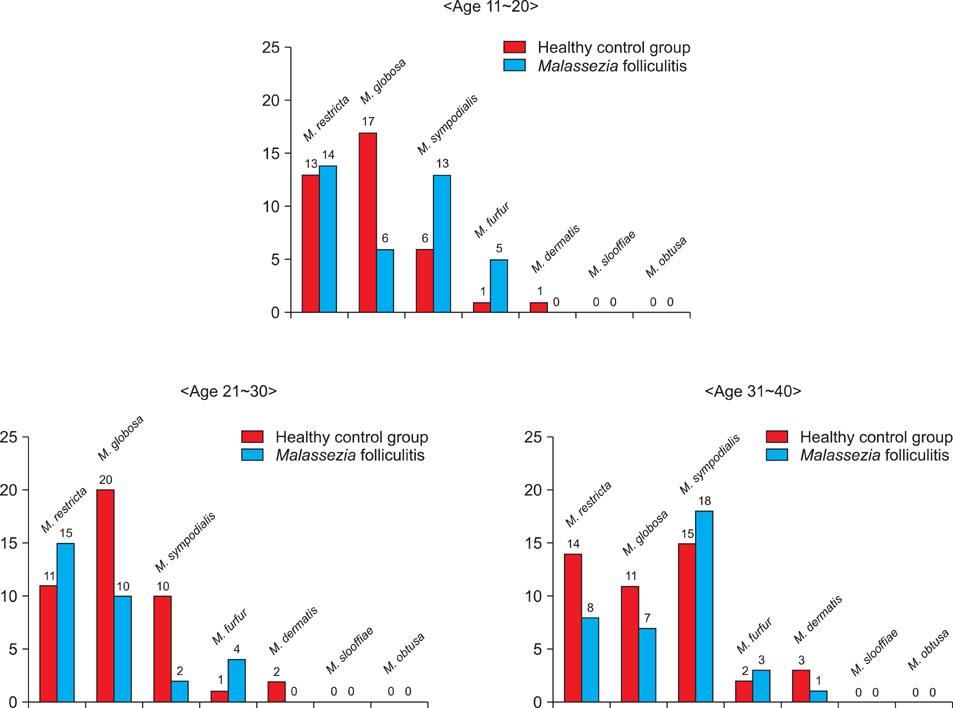
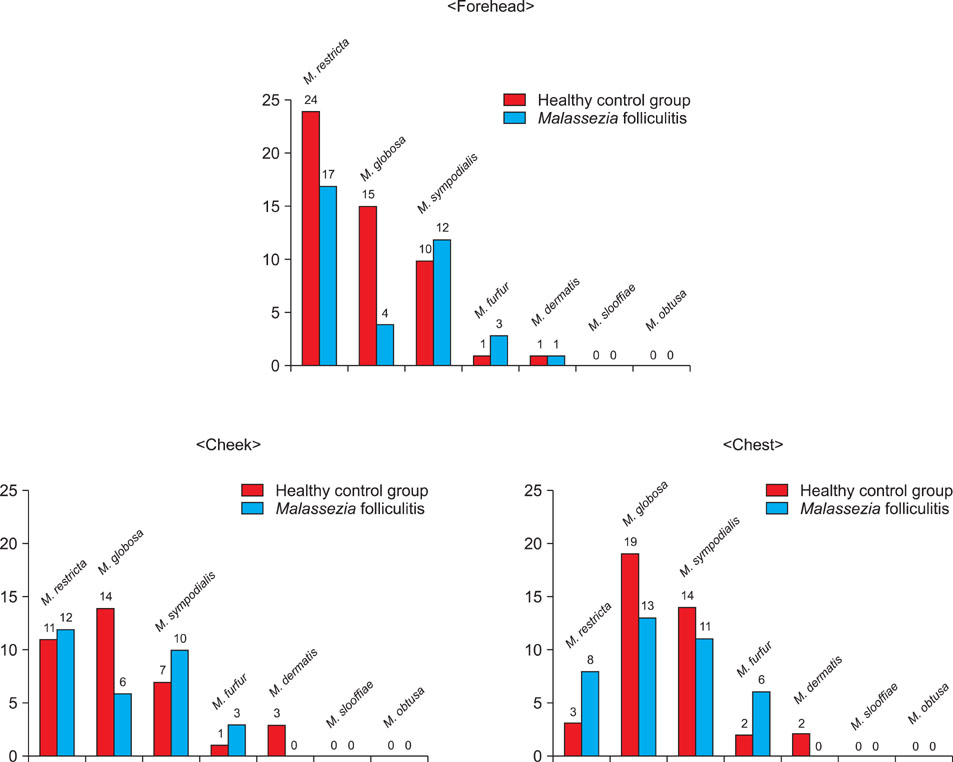
Specimens were taken from the forehead, cheek and chest of 60 patients with Malassezia folliculitis and from the normal skin of 60 age- and gender-matched healthy controls by 26S rDNA PCR-RFLP.
RESULTS
M. restricta was dominant in the patients with Malassezia folliculitis (20.6%), while M. globosa was the most common species (26.7%) in the controls. The rate of identification was the highest in the teens for the patient group, whereas it was the highest in the thirties for the control group. M. globosa was the most predominant species on the chest with 13 cases (21.7%), and M. restricta was the most commonly identified species, with 17 (28.3%) and 12 (20%) cases on the forehead and cheek, respectively, for the patient group.
CONCLUSION
Statistically significant differences were observed between the patient and control groups for the people in their teens and twenties, and in terms of the body site, on the forehead only.
MeSH Terms
Figure
Reference
-
1. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1828–1830.2. Ahn KJ. Taxonomy of the genus Malassezia. Korean J Med Mycol. 1998. 3:81–88.3. Rapelanoro R, Mortureux P, Couprie B, Maleville J, Taïeb A. Neonatal Malassezia furfur pustulosis. Arch Dermatol. 1996. 132:190–193.4. Kim KS, Kye YC, Kim SN, Ahn KJ. A case of neonatal Malassezia pustulosis induced by Malassezia sympodialis. Korean J Dermatol. 2000. 38:1427–1429.5. Ljubojević S, Skerlev M, Lipozencić J, Basta-Juzbasić A. The role of Malassezia furfur in dermatology. Clin Dermatol. 2002. 20:179–182.6. Crespo Erchiga V, Delgado Florencio V. Malassezia species in skin diseases. Curr Opin Infect Dis. 2002. 15:133–142.7. Williamson P, Kligman AM. A new method for the quantitative investigation of cutaneous bacteria. J Invest Dermatol. 1965. 45:498–503.
Article8. Kim SM, Lim SH, Jung BR, Lee YW, Choe YB, Ahn KJ. The application of colony PCR in the molecular biological analysis of Malassezia yeasts. Korean J Med Mycol. 2007. 12:180–188.9. Baillon HE. Traité de botanique médicale cryptogamique, suivi du tableau du droguier de la Faculté de médecine de Paris. 1889. Paris: Doin.10. Guého E, Midgley G, Guillot J. The genus Malassezia with description of four new species. Antonie Van Leeuwenhoek. 1996. 69:337–355.
Article11. Sugita T, Takashima M, Shinoda T, Suto H, Unno T, Tsuboi R, et al. New yeast species, Malassezia dermatis, isolated from patients with atopic dermatitis. J Clin Microbiol. 2002. 40:1363–1367.
Article12. Hirai A, Kano R, Makimura K, Duarte ER, Hamdan JS, Lachance MA, et al. Malassezia nana sp. nov., a novel lipid-dependent yeast species isolated from animals. Int J Syst Evol Microbiol. 2004. 54:623–627.
Article13. Sugita T, Takashima M, Kodama M, Tsuboi R, Nishikawa A. Description of a new yeast species, Malassezia japonica, and its detection in patients with atopic dermatitis and healthy subjects. J Clin Microbiol. 2003. 41:4695–4699.
Article14. Sugita T, Tajima M, Takashima M, Amaya M, Saito M, Tsuboi R, et al. A new yeast, Malassezia yamatoensis, isolated from a patient with seborrheic dermatitis, and its distribution in patients and healthy subjects. Microbiol Immunol. 2004. 48:579–583.
Article15. Cabañes FJ, Theelen B, Castellá G, Boekhout T. Two new lipid-dependent Malassezia species from domestic animals. FEMS Yeast Res. 2007. 7:1064–1076.16. Porro MN, Passi S, Caprill F, Nazzaro P, Morpurgo G. Growth requirements and lipid metabolism of Pityrosporum orbiculare. J Invest Dermatol. 1976. 66:178–182.17. Terui T, Kudo K, Tagami H. Cutaneous immune and inflammatory reactions to Malassezia furfur. Nippon Ishinkin Gakkai Zasshi. 1999. 40:63–67.18. Yohn JJ, Lucas J, Camisa C. Malassezia folliculitis in immunocompromised patients. Cutis. 1985. 35:536–538.19. Ahn KJ. Malassezia species cultured from the lesions of pityriasis versicolor. Korean J Dermatol. 1997. 35:736–743.20. Ahn KJ, Kim KJ, Yi GJ. Efficacy of one-week regimen of itraconazole for pityriasis versicolor. Korean J Med Mycol. 1999. 4:124–130.21. Crespo Erchiga V, Ojeda Martos A, Vera Casaño A, Crespo Erchiga A, Sanchez Fajardo F. Malassezia globosa as the causative agent of pityriasis versicolor. Br J Dermatol. 2000. 143:799–803.22. Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycol. 2000. 38:337–341.
Article23. Pechère M, Krischer J, Remondat C, Bertrand C, Trellu L, Saurat JH. Malassezia spp carriage in patients with seborrheic dermatitis. J Dermatol. 1999. 26:558–561.24. Parry ME, Sharpe GR. Seborrhoeic dermatitis is not caused by an altered immune response to Malassezia yeast. Br J Dermatol. 1998. 139:254–263.
Article25. Lee YW, Kang HJ, Ahn KJ. Malassezia species cultured from the lesions of seborrheic dermatitis. Korean J Med Mycol. 2001. 6:70–76.26. Jang SJ, Choi YB, Ahn KJ. Malassezia species cultured from the lesions of Malassezia folliculitis. Korean J Med Mycol. 2003. 8:55–62.27. Weary PE. Pityrosporum ovale: observations on some aspects of host-parasite interrelationship. Arch Dermatol. 1968. 98:408–422.28. Potter BS, Burgoon CF Jr, Johnson WC. Pityrosporum folliculitis. Report of seven cases and review of the Pityrosporum organism relative to cutaneous disease. Arch Dermatol. 1973. 107:388–391.
Article29. Bäck O, Faergemann J, Hörnqvist R. Pityrosporum folliculitis: a common disease of the young and middle-aged. J Am Acad Dermatol. 1985. 12:56–61.30. Akaza N, Akamatsu H, Sasaki Y, Kishi M, Mizutani H, Sano A, et al. Malassezia folliculitis is caused by cutaneous resident Malassezia species. Med Mycol. 2009. 47:618–624.
Article31. Watanabe S, Kano R, Sato H, Nakamura Y, Hasegawa A. The effects of Malassezia yeasts on cytokine production by human keratinocytes. J Invest Dermatol. 2001. 116:769–773.
Article32. Kim HJ, Lee MH, Ahn KJ. A case of neonatal Malassezia pustulosis identified as Malassezia sympodialis. Korean J Med Mycol. 2001. 6:229–231.33. Cuétara MS, Aguilar A, Martin L, Aspiroz C, del Palacio A. Erlotinib associated with rosacea-like folliculitis and Malassezia sympodialis. Br J Dermatol. 2006. 155:477–479.
Article34. Rhie S, Turcios R, Buckley H, Suh B. Clinical features and treatment of Malassezia folliculitis with fluconazole in orthotopic heart transplant recipients. J Heart Lung Transplant. 2000. 19:215–219.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Nested PCR and RFLP for Identification and Classification of Malassezia Yeasts from Healthy Human Skin
- The Application of 26S rDNA PCR-RFLP in the Identification and Classification of Malassezia Yeast
- Epidemiologic Study of Malassezia Yeasts in Seborrheic Dermatitis Patients by the Analysis of 26S rDNA PCR-RFLP
- Epidemiologic Study of Malassezia Yeasts in Acne Patients by Analysis of 26S rDNA PCR-RFLP
- Molecular Analysis of Malassezia Microflora on the Skin of the Patients with Atopic Dermatitis