J Korean Med Assoc.
2009 Jan;52(1):30-40. 10.5124/jkma.2009.52.1.30.
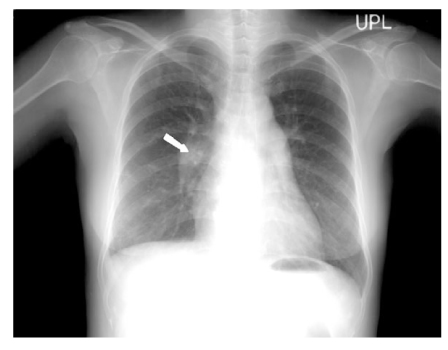
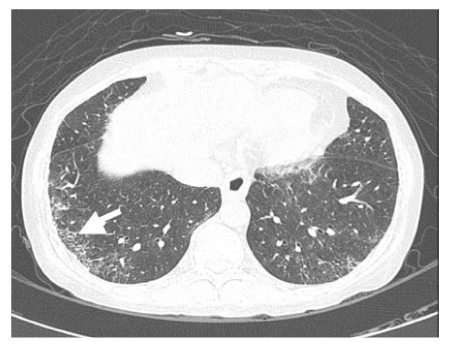
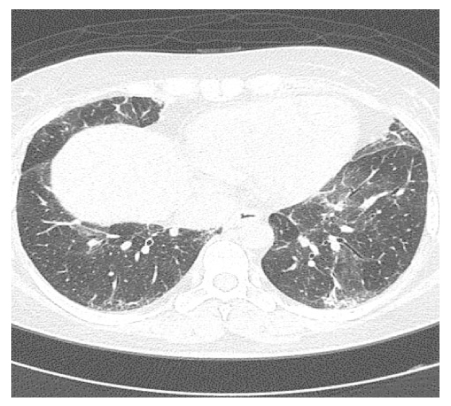
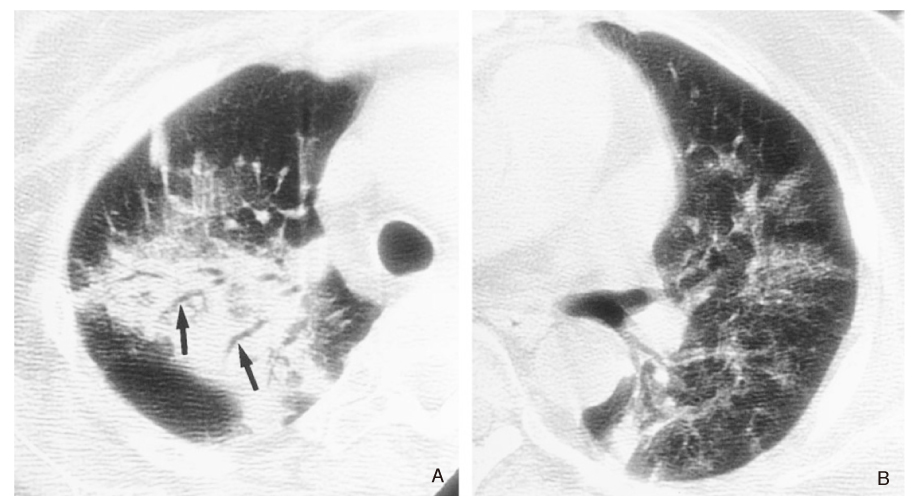
Interstitial Lung Diseases in Collagen Vascular Diseases
- Affiliations
-
- 1Department of Internal medicine, Gachon University of Medicine and Science, Korea. jsw@gilhospital.com
- KMID: 2137731
- DOI: http://doi.org/10.5124/jkma.2009.52.1.30
Abstract
- Different types of interstitial lung diseases (ILDs) develop in collagen vascular diseases (CVDs) such as scleroderma, rheumatoid arthritis, systemic lupus erythematosus, dermatopolymyositis, Sjogren's syndrome, and mixed connective tissue disease. These CVDs represent various histological patterns, including usual interstitial pneumonia, desquamative interstitial pneumonia, nonspecific interstitial pneumonia, bronchiolitis obliterance organizing pneumonia, diffuse alveolar damage, and bronchiolitis. The clinical presentations, prognosis, and response to treatment vary depending on the underlying CVDs, as well as histological patterns of ILDs. In general, the prognosis and survival rate of ILDs in CVDs are better than idiopathic ILDs. Optimal treatment also varies depending on the type of CVDs and the presence of interstitial lung disease, although in many cases, a combination of corticosteroids and cytotoxic drugs are given.
MeSH Terms
-
Adrenal Cortex Hormones
Arthritis, Rheumatoid
Bronchiolitis
Collagen
Dermatomyositis
Fibrosis
Idiopathic Pulmonary Fibrosis
Lung Diseases, Interstitial
Lupus Erythematosus, Systemic
Mixed Connective Tissue Disease
Pneumonia
Prognosis
Sjogren's Syndrome
Survival Rate
Vascular Diseases
Adrenal Cortex Hormones
Collagen
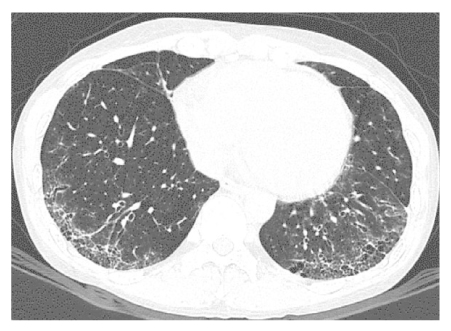
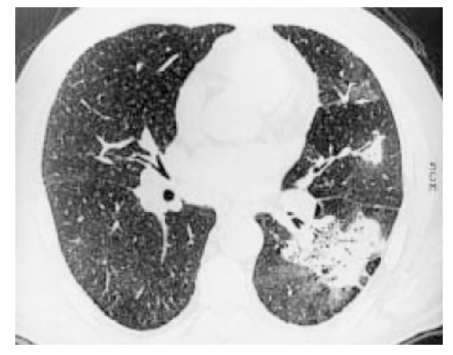
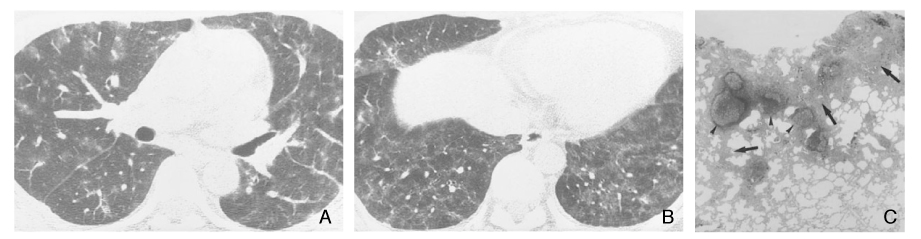
Figure
Cited by 1 articles
-
Clinical manifestations and diagnosis of rheumatoid arthritis
You Jung Ha, Soo-Kon Lee
J Korean Med Assoc. 2010;53(10):862-870. doi: 10.5124/jkma.2010.53.10.862.
Reference
-
1. Marten K, Dicken V, Kneitz C, Hohmann M, Kenn W, Hahn D, Engelke C. Intrstitial lung disease associated with collagen vascular disorders:disease quantification using a computer-aided diagnosis tool. Eur Radiol. 2008. 11:1.2. Kim DS, Yoo B, Lee JS, Kim EK, Lim CM, Lee SD, Koh Y, Kim WS, Kim WD, Colby TV, Kitiaichi M. The major histopathologic pattern of pulmonary fibrosis in scleroderma is nonspecific interstitial pneumonia. Sarcoidosis Vasc Diffuse Lung Dis. 2002. 19:121–127.3. Kim EA, Lee KS, Johkoh T, Kim TS, Suh GY, Kuon OJ, Han J. Interstitial Lung Diseases Associated with Collagen Vascular Diseases: Radiologic and Histopathologic Findings. Radio Graphics. 2002. 22:S151–S165.
Article4. Uzun Oguz, Akpolat Tekin, Erkan Levent. Pulmonary Vasculitis in Behcet disease: A Cumulative Analysis. Chest. 2005. 127:2243–2253.5. Parambil JG, Myers JL, Ryu JH. Diffuse Alveolar Damage: Uncommon Manifestation of Pulmonary Involvement in Patients With Connective Tissue Diseases. Chest. 2006. 130:553–558.6. Kang EH, Lee EB, Shin KC, Im CH, Chung DH, Han SK, Song YW. Interstitial lung disease in patients with plymyositis, dermatomyositis and amyopathic dermatomyositis. Rheumatology. 2005. 44:1282–1286.
Article7. Ayhan-Ardie F.Figen, Oken Oznur, Yorgancioglu Z.Rezan, Ustun Nilgun, Gokharman F.Dilek. Pulmonary involvement in lifelong non-somking patients with rheumatoid arthritis and ankylosing spondylitis without respiratory symtoms. Clin Rheumatol. 2006. 25:213–218.
Article8. Lamblin C, Bergoin C, Saelens T, Wallaert B. Interstitial lung diseases in collagen vascular diseases. Eur Respir J. 2001. S32. 69s–80s.9. Suda T, Fujisawa T, Enomoto N, Nakamura Y, Inui N, Naito T, Hashimoto D, Sato J, Toyoshima M, Hashizume H, Chida K. Interstitial lung diseases associated with amyopathic dermatomyositis. Eur Respir J. 2006. 28:1005–1012.
Article10. Bodolay E, Szekanecz Z, Dévényi K, Galuska L, Csípo I, Vègh J, Garai I, Szegedi G. Evaluation of interstitial lung disease in mixed connective tissue disease (MCTD). Rheutology. 2005. 44:656–661.
Article11. Wells AU, Hansell DM, Rubens MB, King AD, Cramer D, Black CM, du Bois RM. Fibrosing alveolitis in systemic sclerosis: indices of lung function in relation to extent of disease on computed tomography. Arthritis Rheum. 1997. 40:1229–1236.
Article12. Harrison NK, Glanville AR, Strickland B, Haslam PL, Corrin B, Addis BJ, Lawrence R, Millar AB, Black CM, Turner-Warwick M. Pulmonary involvement in systemic sclerosis: the detection of early changes by thin section CT scan, bronchoalveolar lavage and 99mTc-DTPA clearance. Respir Med. 1989. 83:403–414.
Article13. Bouros DE, Polychronopoulos V, Conron M, Black CM, Nicholson A, duBois RM. Histopathologic subgroups in patients with fibrosing alveolitis associated with systemic sclerosis. Eur Respir J. 1999. 14(30):s. 272S.14. Wallaert B, Aerts C, Bart F, Hatron PY, Dracon M, Tonnel AB, Voisin C. Alveolar macrophage dysfunction in systemic lupus erythematosus. Am Rev Respir Dis. 1987. 136:293–297.
Article15. Wallaert B, Hatron PY, Grosbois JM, Tonnel AB, Devulder B, Voisin C. Subclinical pulmonary involvement in collagen vascular diseases assessed by bronchoalveolar lavage. Relationship between alveolitis and subsequent changes in lung function. Am Rev Respir Dis. 1986. 133:574–580.16. White B, Wigley F, Wise R, Bleecker E. Expression of chemokines interleukin-8 (IL-8), RANTES, and macrophage inhibitory factor-1 (MIP-1) in bronchoalveolar lavage fluid of patients with systemic sclerosis (SSc). Arthritis Rheum. 1994. 37:S263.17. Rennard SI, Bitterman PB, Ozaki T, Rom WN, Crystal RG. Colchicine suppresses the release of fibroblast growth factors from alveolar macrophages in vitro. Am Rev Respir Dis. 1988. 137:181–185.
Article18. DeClerck LS, Dequeker J, Francx L, Demedts M. D-Penicillamine therapy and interstitial lung disease in scleroderma. Arthritis Rheum. 1987. 30:643–650.19. Silver RM, Warrick JH, Kinsella MB, Staudt LS, Baumann MH, Strange C. Cyclophosphamide and lowdose prednisone therapy in patients with systemic sclerosis (scleroderma) with interstitial lung disease. J Rheumatol. 1993. 20:838–844.20. Clements PJ, Lachenbruch PA, Sterz M, Danovitch G, Hawkins R, Ippoliti A, Paulus HE. Cyclosporine in systemic sclerosis. Results of a fortyeight-week open safety study in ten patients. Arthritis Rheum. 1993. 36:75–83.
Article21. Yousem SA, Colby TV, Carrington CB. Lung biopsy in rheumatoid arthritis. Am Rev Respir Dis. 1985. 131:770–777.22. McDonagh J, Greaves M, Wright AR, Heycock C, Owen JP, Kelly C. High resolution computed tomography of the lungs in patients with RA and interstitial lung disease. Br J Rheumatol. 1994. 33:118–122.
Article23. Yousem SA, Colby TV, Carrington CB. Follicular bronchitis/bronchiolitis. Human Pathol. 1985. 16:700–706.
Article24. Gosset P, Perez T, Lassalle P, Duquesnoy B, Farre JM, Tonnel AB, Capron A. Increased TNF-a secretion by alveolar macrophages from patients with rheumatoid arthritis. Am Rev Respir Dis. 1991. 143:593–597.
Article25. Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA. Bronchiolitis obliterans organizing pneumonia. N Engl J Med. 1985. 312:152–158.
Article26. Rolla G, Brussino L, Bertero MT, Colagrande P, Converso M, Bucca C, Polizzi S, Caligaris-Cappio F. Increased nitric oxide in exhaled air of patients with systemic lupus erythematosus. J Rheumatol. 1997. 24:1066–1071.27. Holgate ST, Glass DN, Haslam P, Maini RN, Turner-Warwick M. Respiratory involve-ment in systemic lupus erythematosus: A clinical and immunological study. Clin Exp Immunol. 1976. 24:385–395.28. Mino M, Noma S, Taguchi Y, Tomii K, Kohri Y, Oida K. Pulmonary involvement in polymyositis and dermato-myositis: sequential evaluation with CT. AJR. 1997. 169:83–87.
Article29. Deheinzelin D, Capelozzi VL, Kairala RA, Barbas JV, Saldiva PHN, de Carvalho CRR. Intertstitial lung disease in primary Sjögren's syndrome: clinical pathological evaluation and response to treatment. Am J Respir Crit Care Med. 1996. 15:794–799.30. Lahdensuo A, Korpela M. Pulmonary findings in patients with primary Sjögren's syndrome. Chest. 1995. 108:316–319.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulmonary Tuberculosis Presenting as Diffuse Interstitial Lung Disease Associated with the Lymphadenopathy of Mediastinum and Abdomen
- A Radiologic Approach to Diffuse Interstitial Lung Disease
- Interstitial Lung Diseases: Respiratory Review of 2013
- Treatment of connective tissue disease-associated interstitial lung disease: the pulmonologist's point of view
- Idiopathic Interstitial Pneumonias: Radiologic Findings