J Korean Ophthalmol Soc.
2009 Mar;50(3):376-382. 10.3341/jkos.2009.50.3.376.
Short-term Clinical Outcome of Patterned Scanning Laser Photocoagulation With Short Exposure Time in Diabetic Retinopathy
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. hjwin@lycos.co.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- 3Department of Ophthalmology, Seoul Metropolitan Boramae Hospital, Seoul, Korea.
- 4Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2111247
- DOI: http://doi.org/10.3341/jkos.2009.50.3.376
Abstract
-
PURPOSE: To investigate the clinical effect and complications of patterned scanning laser photocoagulation with short exposure time in diabetic retinopathy.
METHODS
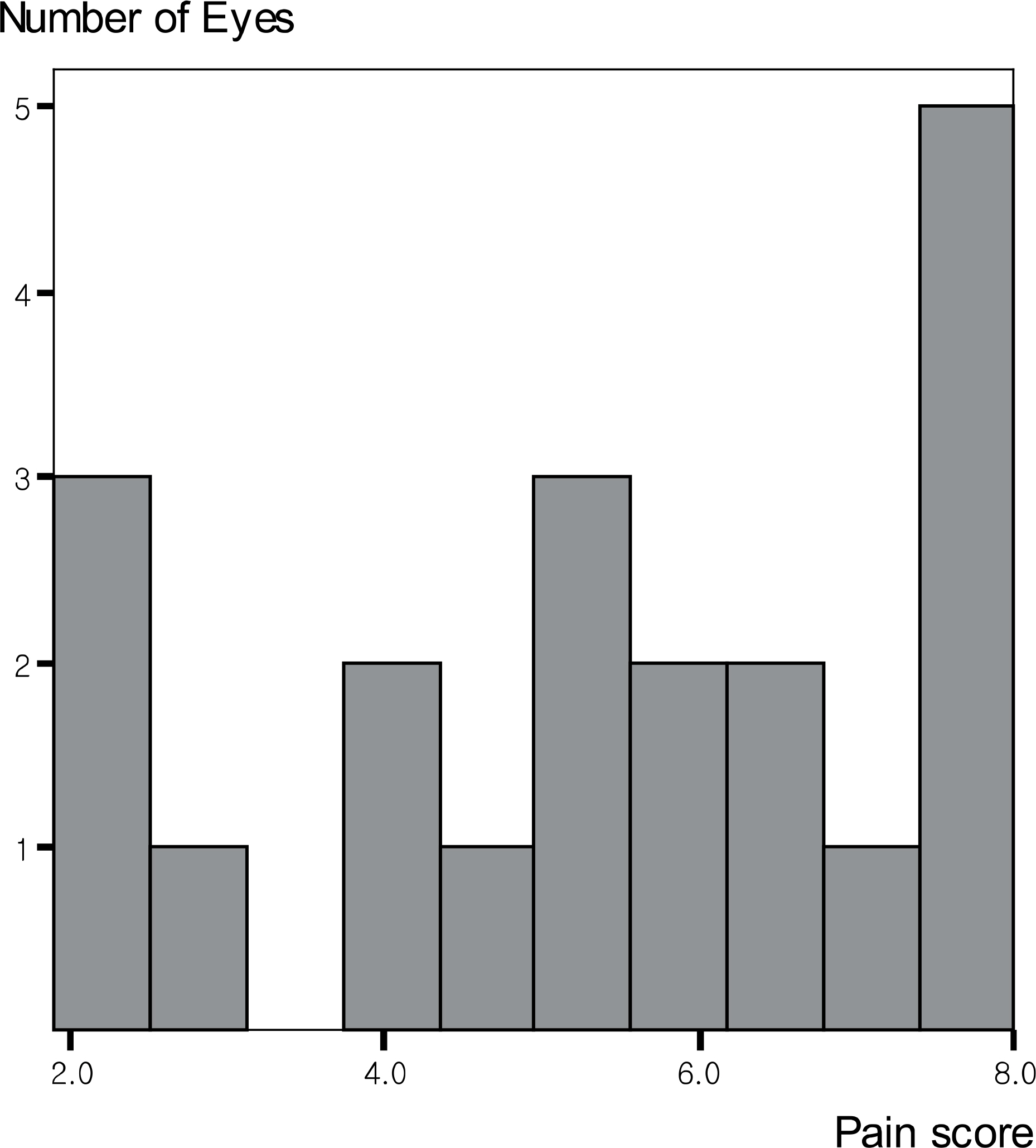
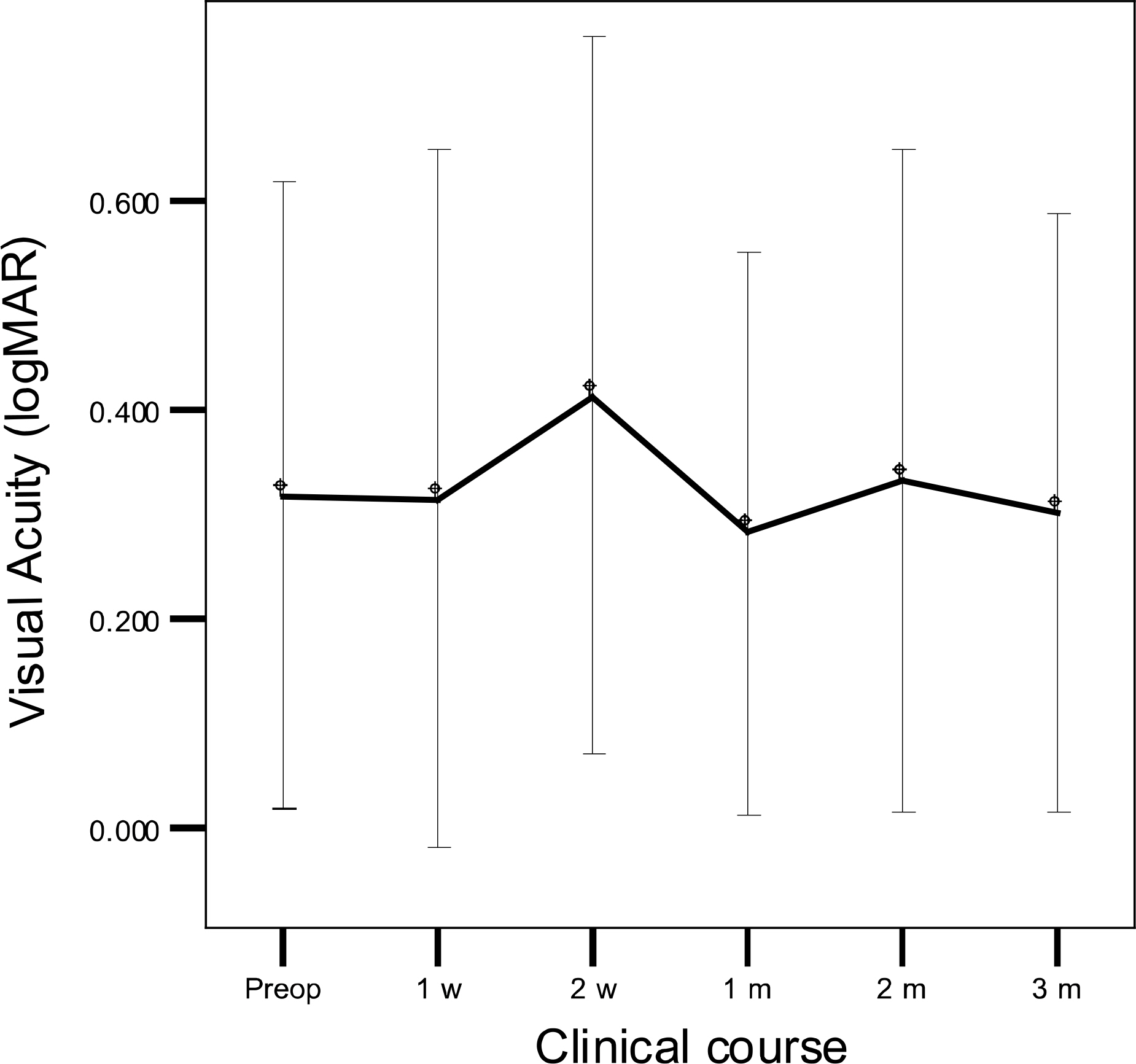
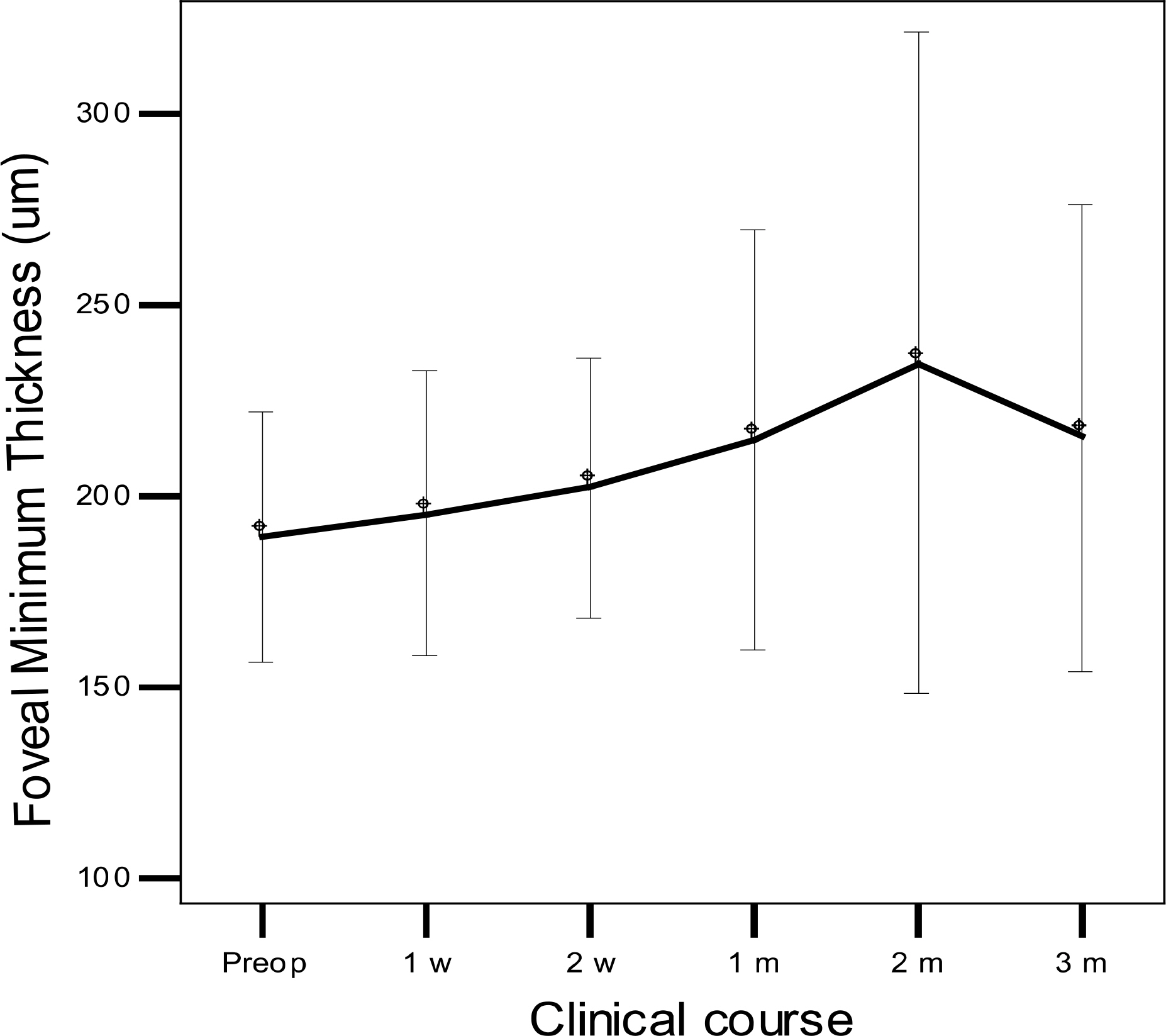
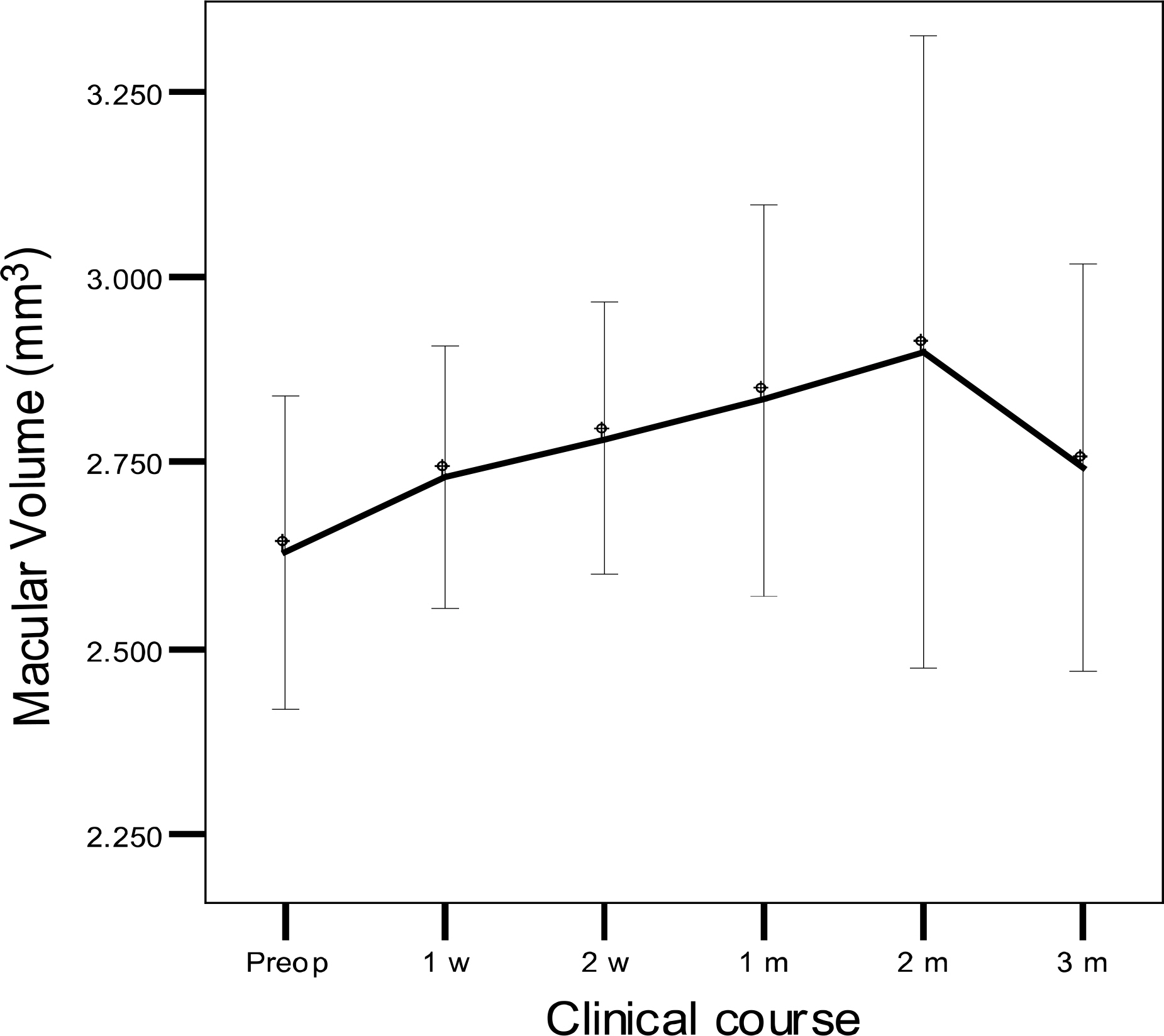
A prospective study was performed on patients with diabetic retinopathy who required panretinal photocoagulation (PRP). Twenty-nine eyes of twenty five consecutive patients underwent patterned scanning laser photocoagulation with exposure time of 0.02 sec over the entire retina. Pain score at treatment, best-corrected visual acuity, the development of macular edema, regression of neovascularization in fluorescein angiography, and related complications were monitored during a three-month follow-up.
RESULTS
Treatment time for PRP was much reduced to 6.1 min on the entire retina. Pain during the photocoagulation was moderate, and enabled patients to finish PRP with ease. During a three-month follow-up, visual acuity was well preserved. Foveal minimum thickness increased at 1 month after treatment and maintained in a study period of three months. Macular volume showed significant increase (3.6%) at 1 month after treatment, maximum increase (9.8%) at 2 months, and persistent increase (4.9%) at 3 months. In every patient with very severe nonproliferative diabetic retinopathy, retina was maintained, and in 10 of 18 eyes with proliferative diabetic retinopathy, neovascularization regressed during follow-up period. No significant complication occurred except a transient vitreous hemorrhage in one eye.
CONCLUSIONS
Patterned scanning laser photocoagulation with short exposure time may induce transient macular edema, but the visual acuity was preserved without any other significant complication. It is considered to be a safe and efficient treatment method in diabetic retinopathy.
MeSH Terms
Figure
Cited by 3 articles
-
Effect of Focal and Grid Pattern PASCAL Photocoagulation Treatment in Diabetic Macular Edema
Jae Kwan Park, Woo Jin Jeung
J Korean Ophthalmol Soc. 2011;52(2):197-202. doi: 10.3341/jkos.2011.52.2.197.Short-Term Clinical Outcomes of Laser Trabeculoplasty Using a 577-nm Wavelength Laser
Jong Min Kim, Kyong Jin Cho, Sung Eun Kyung, Moo Hwan Chang
J Korean Ophthalmol Soc. 2014;55(4):563-569. doi: 10.3341/jkos.2014.55.4.563.Comparison of the Effects of Patterned and Conventional Panretinal Photocoagulation on Diabetic Retinopathy
Ji-Wook Yang, Young-Chun Lee
J Korean Ophthalmol Soc. 2010;51(12):1590-1597. doi: 10.3341/jkos.2010.51.12.1590.
Reference
-
References
1. Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: Clinical application of DRS findings. DRS report no. 8. Ophthalmology. 1981; 88:583–600.2. Early Treatment of Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report No. 9. Ophthalmology. 1991; 98:766–85.3. Petrovic V, Bhisitkul RB. Lasers and diabetic retinopathy: the art of gentle destruction. Diabetes Technol Ther. 1999; 1:177–87.4. Early Treatment of Diabetic Retinopathy Study Research Group. Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: ETDRS report No. 3. Int Ophthalmol Clin. 1987; 27:254–64.5. Prendiville PL, McDonnell PJ. Complications of Laser Surgery. Int Ophthalmol Clin. 1992; 32:179–204.
Article6. Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999; 14:200–9.
Article7. Laursen ML, Moeller F, Sander B, Sjoelie AK. Subthreshold micropulse diode laser treatment in diabetic macular oedema. Br J Ophthalmol. 2004; 88:1173–9.
Article8. Framme C, Schuele G, Kobuch K, et al. Investigation of selective retina treatment (SRT) by means of 8 ns laser pulses in a rabbit model. Lasers Surg Med. 2008; 40:20–7.
Article9. Blumenkranz MS, Yellachich D, Andersen DE, et al. Semi-automated patterned scanning laser for retinal photocoagulation. Retina. 2006; 26:370–6.
Article10. L'Esperance FA. Ophthalmic lasers. 3rd ed.Vol. 1. St Louis: CV Mosby Co.;1989. p. 78–112.11. Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976; 2:175–84.
Article12. Al-Hussainy S, Dodson PM, Gibson JM. Pain response and follow-up of patients undergoing panretinal laser photocoagulation with reduced exposure times. Eye. 2008; 22:96–9.
Article13. Moon HS, Nam DH, Paik HJ. Comparison of anesthetic efficacy and intraocular pressure by volume of sub-Tenon's anesthetic in vitreoretinal surgery. J Korean Ophthalmol Soc. 2006; 47:1759–68.14. Dorin G. Evolution of retinal laser therapy: minimum intensity photocoagulation (MIP). Can the laser heal the retina without harming it? Semin Ophthalmol. 2004; 19:62–8.15. Prskavec FH, Fulmek R, Klemen C, Stelzer N. Changes in the visual field and dark adaptation following panretinal photocoagulation in diabetic retinopathy. Klin Monatsbl Augenheilkd. 1986; 189:385–7.16. Tsujikawa A, Kiryu J, Dong J, et al. Quantitative analysis of diabetic macular edema after scatter laser photocoagulation with the scanning retinal thickness analyzer. Retina. 1999; 19:59–64.
Article17. Fong DS, Girach A, Boney A. Visual side effects of successful scatter laser photocoagulation surgery for proliferative diabetic retinopathy: A literature review. Retina. 2007; 27:816–24.18. McDonald HR, Schatz H. Macular edema following panretinal photocoagulation. Retina. 1985; 5:5–10.
Article19. Shimura M, Yasuda K, Shiono T. Posterior sub-Tenon's capsule injection of triamcinolone acetonide prevents panretinal photo-coagulation-induced visual dysfunction in patients with severe diabetic retinopathy and good vision. Ophthalmology. 2006; 113:381–7.
Article20. Meyers SM. Macular edema after scatter laser photocoagulation for proliferative diabetic retinopathy. Am J Ophthalmol. 1980; 90:210–6.
Article21. Shimura M, Yasuda K, Nakazawa T, et al. Quantifying alterations of macular thickness before and after panretinal photocoagulation in patients with severe diabetic retinopathy and good vision. Opht-halmology. 2003; 110:2386–94.
Article22. Bandello F, Polito A, Del BM, et al. Light versus classic laser treatment for clinically significant diabetic macular edema. Br J Ophthalmol. 2005; 89:864–70.23. Rogell GD. Incremental panretinal photocoagulation: results in treating proliferative diabetic retinopathy. Retina. 1983; 3:308–11.24. Wei ZY, Hu SX, Tang N, et al. Effect of argon laser photo-coagulation on diabetic retinopathy. Di Yi Jun Yi Da Xue Xue Bao. 2004; 24:1313–5.25. Doft B, Blankenship G. Retinopathy risk factor regression after laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1984; 91:1453–7.
Article26. Vander JF, Duker JS, Benson WE, et al. Long-term stability and visual outcome after favorable initial response of proliferative diabetic retinopathy to panretinal photocoagulation. Ophthalmology. 1991; 98:1575–9.
Article27. Morgan CM, Schatz H. Atrophic creep of the retinal pigment epithelium after focal macular photocoagulation. Ophthalmology. 1989; 96:96–103.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ciliochoroidal Detachment After Patterned Scanning Laser Photocoagulation With Short Exposure Time
- Comparison of the Effects of Patterned and Conventional Panretinal Photocoagulation on Diabetic Retinopathy
- Comparison of the Effects of Patterned and Conventional Laser Photocoagulation in Branch Retinal Vein Occlusion
- Comparison of the Time Required for Panretinal Photocoagulation and Associated Pain between Navilas(R) and Conventional Laser Therapy in Diabetic Retinopathy
- Transscleral Diode Laser Photocoagulation for Retinopathy of Prematurity: Short-term Structural Outcome