J Korean Ophthalmol Soc.
2014 Aug;55(8):1150-1154.
Comparison of the Time Required for Panretinal Photocoagulation and Associated Pain between Navilas(R) and Conventional Laser Therapy in Diabetic Retinopathy
- Affiliations
-
- 1Department of Ophthalmology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. 991027js@hanmail.net
Abstract
- PURPOSE
To compare the pain scale and time necessary for panretinal photocoagulation (PRP) between Navilas(R) (OD-OS, Teltow, Germany) and conventional laser in diabetic retinopathy.
METHODS
Fifteen patients who required PRP for diabetic retinopathy were enrolled in the present study. PRP was performed using Navilas(R) (5 x 5 array patterned system) in the superior, nasal and inferior areas, and using conventional laser at the temporal area 1 week later. Total time of laser application and number of laser shots were counted for calculating required time per 100 spots of each laser system. Immediately after the laser photocoagulation, patients were asked to quantify their pain on a visual analog pain scale (0 = no pain; 10 = worst pain).
RESULTS
PRP using Navilas(R) required shorter time per 100 laser spots (27.7 sec vs. 102.0 sec, p < 0.001) and subjects had lower treatment-related pain than with the conventional laser system (3.3 vs. 6.9, p < 0.001).
CONCLUSIONS
PRP using Navilas(R) can be considered as an efficient method for improving patient and operator's comfort with faster laser application and lower treatment-related pain.
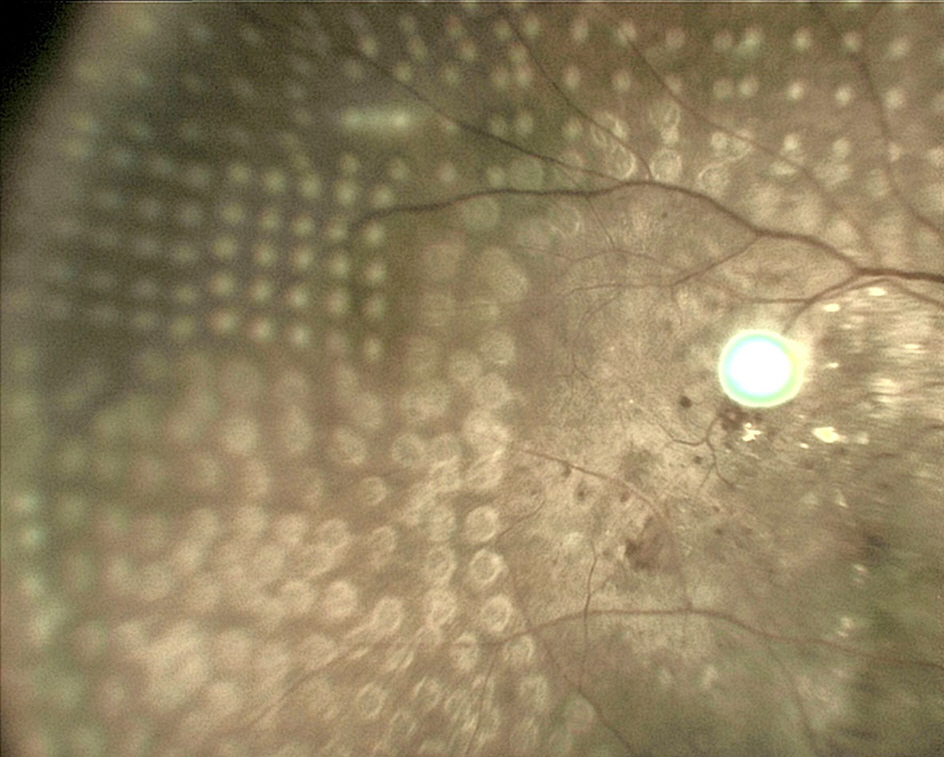
Figure
Reference
-
References
1. Kemt M, Cheuteu RE, Cserhati S, et al. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol. 2012; 6:289–96.2. Nakamura Y, Mitamura Y, Ogata K, et al. Functional and morphological changes of macula after subthreshold micropulse diode laser photocoagulation for diabetic macular oedema. Eye (Lond). 2010; 24:784–8.
Article3. Bolz M, Kriechbaum K, Simader C, et al. In vivo retinal morphology after grid laser treatment in diabetic macular edema. Ophthalmology. 2010; 117:538–44.
Article4. Chhablani J, Kozak I, Barteselli G, El-Emam S. A novel navigated laser system brings new efficacy to the treatment of retinovascular disorders. Oman J Ophthalmol. 2013; 6:18–22.
Article5. Chalam KV, Murthy RK, Brar V, et al. Evaluation of a novel, non contact, automated focal laser with integrated (NAVILAS) fluorescein angiography for diabetic macular edema. Middle East Afr J Ophthalmol. 2012; 19:158–62.
Article6. Kozak I, Oster SF, Cortes MA, et al. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology. 2011; 118:1119–24.
Article7. Neubauer AS, Langer J, Liegl R, et al. Navigated macular laser decreases retreatment rate for diabetic macular edema: a comparison with conventional macular laser. Clin Ophthalmol. 2013; 7:121–8.8. Ober MD, Kernt M, Cortes MA, Kozak I. Time required for navigated macular laser photocoagulation treatment with the Navilas. Graefes Arch Clin Exp Ophthalmol. 2013; 251:1049–53.
Article9. MeyerSchwickerath G. Light coagulation; a method for treatment and prevention of the retinal detachment. Albrecht Von Graefes Arch Ophthalmol. 1954; 156:234.10. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981; 88:583–600.11. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1987; 94:761–74.12. Pahor D. Visual field loss after argon laser panretinal photocoagulation in diabetic retinopathy: full- versus mild-scatter coagulation. Int Ophthalmol. 1998; 22:313–9.13. Lewis H, Schachat AP, Haimann MH, et al. Choroidal neovascularization after laser photocoagulation for diabetic macular edema. Ophthalmology. 1990; 97:503–10.
Article14. Yuki T, Kimura Y, Nanbu S, et al. Ciliary body and choroidal detachment after laser photocoagulation for diabetic retinopathy. A high-frequency ultrasound study. Ophthalmology. 1997; 104:1259–64.15. Kernt M, Cheuteu R, Vounotrypidis E, et al. Focal and panretinal photocoagulation with a navigated laser (NAVILAS®). Acta Ophthalmol. 2011; 89:e662–4.
Article16. Kozak I, Kim JS, Oster SF, et al. Focal navigated laser photo-coagulation in retinovascular disease: clinical results in initial case series. Retina. 2012; 32:930–5.17. Yang JW, Lee YC. Comparison of the effects of patterned and conventional panretinal photocoagulation on diabetic retinopathy. J Korean Ophthalmol Soc. 2010; 51:1590–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Effects of Patterned and Conventional Panretinal Photocoagulation on Diabetic Retinopathy
- The Comparison of Retinal Blood Flow and Foveal Avascular Zone between the Eyes with Panretinal Photocoagulation and the Eyes without PRP using Scanning Laser Ophthalmoscope[SLO] in Diabetic Retinopathy
- Peripheral Scatter Treatment in Diabetic Retinopathy
- Clinical Analysis of Panretinal Photocoagulation for Diabetic Retinopathy
- Diode Laser Panretinal Photocoagulation in Diabetic Retinopathy