J Korean Ophthalmol Soc.
2010 Dec;51(12):1590-1597.
Comparison of the Effects of Patterned and Conventional Panretinal Photocoagulation on Diabetic Retinopathy
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea School of Medicine, Seoul, Korea. yclee@cmcnu.or.kr
Abstract
- PURPOSE
To compare the therapeutic effects and complications after panretinal photocoagulation (PRP) and discomforts of patients using patterned PRP versus conventional PRP for diabetic retinopathy.
METHODS
Eighty patients who required PRP due to diabetic retinopathy were enrolled in a prospective randomized controlled study. The patients were randomly divided into two groups: a patterned PRP group in which PRP was performed with a short laser exposure time (0.02 seconds) and a conventional PRP group with a long exposure time (0.2 seconds). At the 1-year follow-up visit, the progressions of diabetic retinopathy, best-corrected visual acuity, and central macular thickness were evaluated. All patients were questioned about the grade of pain during PRP. In addition, the complications after PRP were investigated.
RESULTS
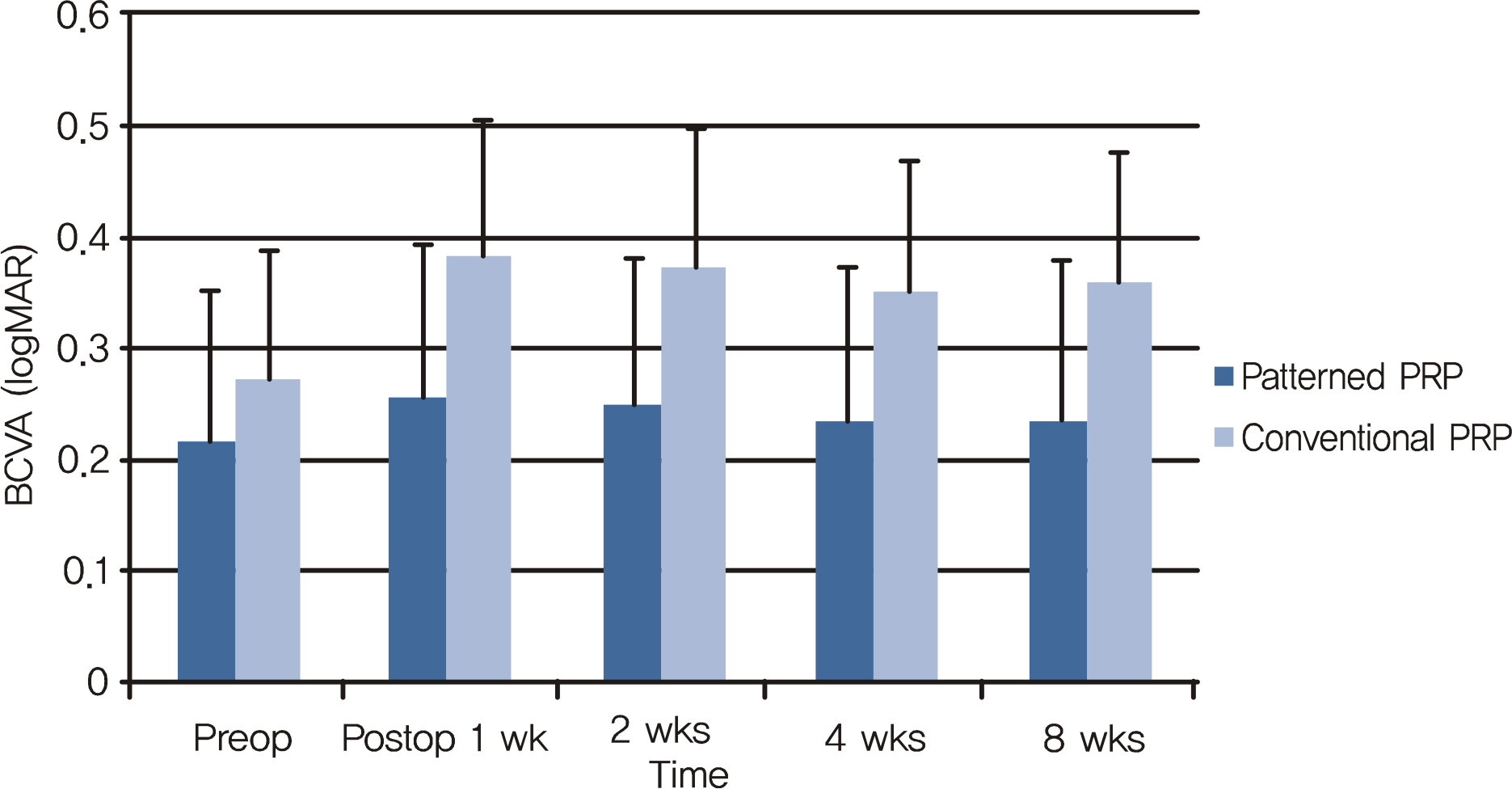
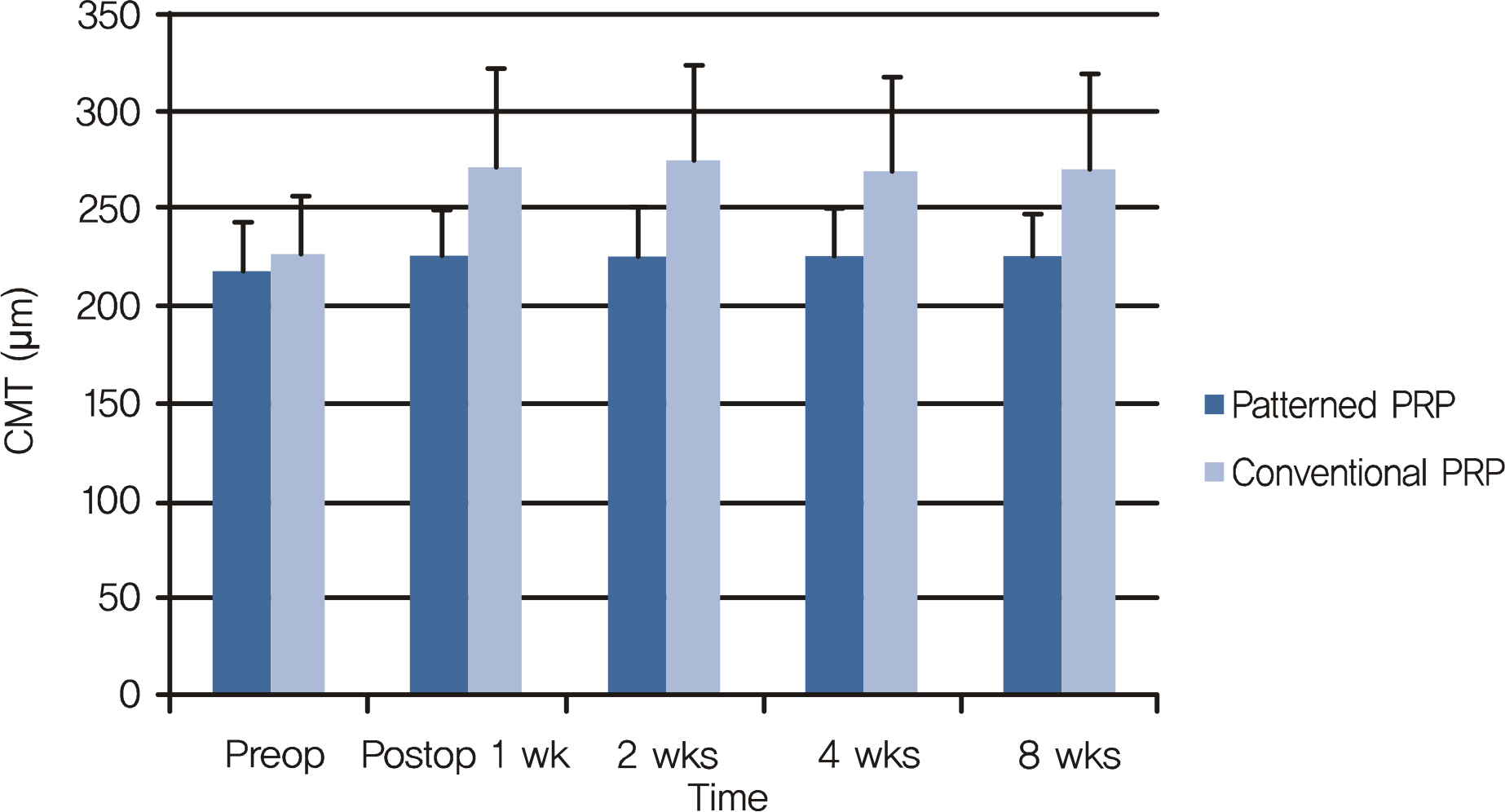
There were no statistical differences in clinical characteristics between both groups. The progression of diabetic retinopathy was not different in both groups at the 1-year follow-up visit. The best-corrected visual acuities at 1, 2, 4, and 8 weeks after PRP were decreased in both groups and, in the conventional PRP group, the decrements of visual acuity were greater than in the patterned PRP group. The increments of central macular thickness were also greater in the conventional PRP group than the patterned PRP group.
CONCLUSIONS
When patterned PRP is performed using a short laser exposure time, the efficacy in the treatment of diabetic retinopathy is similar to that of the conventional PRP using a longer laser exposure time. Moreover, patterned PRP is less painful, and fewer complications.
MeSH Terms
Figure
Reference
-
References
1. Wessing A, Meyer-Schwickerath G. Treatment of diabetic retinopathy by light-coagulation. Diabetologia. 1969; 5:312–7.2. Beetham WP, Aiello LM, Balodimos MC, Koncz L. Ruby laser photocoagulation of early diabetic neovascular retinopathy: preliminary report of long-term controlled study. Arch Ophthalmol. 1970; 83:261–72.3. Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of Diabetic Retinopathy Study (DRS) findings. DRS report no.8. Ophthalmology. 1981; 88:583–600.4. Early Treatment Diabetic Retinopathy Study Research Group. Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report No. 3. Int Ophthalmol Clic. 1987; 27:254–64.5. McDonald HR, Schatz H. Macular edema following panretinal photocoagulation. Retina. 1985; 5:5–10.
Article6. Khosla PK, Rao V, Tewari HK, Kumar A. Contrast sensitivity in diabetic retinopathy after panretinal photocoagulation. Ophthalmic Surg. 1994; 25:516–20.
Article7. Pahor D. Visual field loss after argon laser panretinal photocoagulation in diabetic retinopathy: full- versus mild-scatter coagulation. Int Ophthalmol. 1998; 22:313–9.8. Yuki T, Kimura Y, Nanbu S, et al. Ciliary body and choroidal detachment after laser photocoagulation for diabetic retinopathy. A high-frequency ultrasound study. Ophthalmology. 1997; 104:1259–64.9. Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976; 2:175–84.
Article10. Patz A. Studies on retinal neovascularization. Invest Ophthalmol Vis Sci. 1980; 19:1133–8.11. Molnar J, Oastry S, Tsacopuolos M. Effect of laser photocoagulation on oxygenation of the retina in miniature pigs. Invest Ophthalmol Vis Sci. 1985; 26:1410–4.12. Yoshimura N, Matsumoto M, Shimizy H, et al. Photocoagulated human retinal pigment epithelial cells produce an inhibitor of vascular endothelial cell proliferation. Invest Ophthalmol Vis Sci. 1995; 36:1686–91.13. Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002; 109:920–7.
Article14. Wu L, Martinez-Castellanos MA, Quiroz-Mercado H, et al. Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol. 2008; 246:81–7.
Article15. Chun DW, Heier JS, Topping TM, et al. A pilot study of multiple intravitreal injections of ranibizumab in patients with center-in-volving clinically significant diabetic macular edema. Ophthalmology. 2006; 113:1706–12.
Article16. Moorman CM, Hamilton AMP. Clinical applications of the micro-pulse diode laser. Eye. 1999; 13:145–50.
Article17. Bandello F, Brancoto R, Menchini U, et al. Light panretinal photocoagulation (LPRP) versus classic panretinal photocoagulation (CPRP) in proliferative diabetic retinopathy. Semin Ophthalmol. 2001; 16:12–8.
Article18. Wade EC, Blankenship GW. The effect of short versus long exposure times of argon laser panretinal photocoagulation on proliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 1990; 228:226–31.
Article19. Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999; 14:200–9.
Article20. Paulus YM, Jain A, Gariano RF, et al. Healing of retinal photocoagulation lesions. Invest Ophthalmol Vis Sci. 2008; 49:5540–5.
Article21. Cuthbertson FM, Newsom RS, Wainwright AC. Kinetic anesthesia for laser surgery. Eye. 2005; 19:1205–7.22. Vaideanu D, Taylor P, McAndrew P, et al. Double masked randomized controlled trial to assess the effectiveness of paracetamol in reducing pain in panretinal photocoagulation. Br J Ophthalmol. 2006; 90:713–7.23. Weinberger D, Ron Y, Lichter H, et al. Analgesic effect of topical sodium diclofenac 0.1% drops during retinal laser photocoagulation. Br J Ophthalmol. 2000; 84:135–7.
Article24. Al-Hussainy S, Dodson PM, Gibson JM. Pain response and follow-up of patients undergoing panretinal laser photocoagulation with reduced exposure times. Eye. 2008; 22:96–9.
Article25. Sanghvi C, McLauchlan R, Delgado C, et al. Initial experience with the Pascal photocoagulator: a pilot study of 75 procedures. Br J Ophthalmol. 2008; 92:1061–4.
Article26. Cho BJ, Kim TW, Woo SJ, et al. Short-term clinical outcome of patterned scanning laser photocoagulation with short exposure time in diabetic retinopathy. J Korean Ophthalmol Soc. 2009; 50:376–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Time Required for Panretinal Photocoagulation and Associated Pain between Navilas(R) and Conventional Laser Therapy in Diabetic Retinopathy
- A Case of Ciliochoroidal Detachment After Patterned Scanning Laser Photocoagulation With Short Exposure Time
- Change in Subfoveal Choroidal Thickness after Patterned Panretinal Photocoagulation in Patients with Diabetic Retinopathy
- Retinal Vascular Caliber Changes in Diabetic Retinopathy after Panretinal Photocoagulation and Additive Bevacizumab Injections
- Macular Thickness and Visual Acuity Before and After Panretinal Photocoagulation in Severe Diabetic Retinopathy