J Korean Ophthalmol Soc.
2010 Oct;51(10):1368-1373.
Comparison of the Effects of Patterned and Conventional Laser Photocoagulation in Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, The Catholic University of Korea School of Medicine, Seoul, Korea. quintet@catholic.ac.kr
Abstract
- PURPOSE
To compare the clinical effect and complications between patterned laser photocoagulation with short exposure time and conventional laser photocoagulation for neovascularization in branch retinal vein occlusion (BRVO).
METHODS
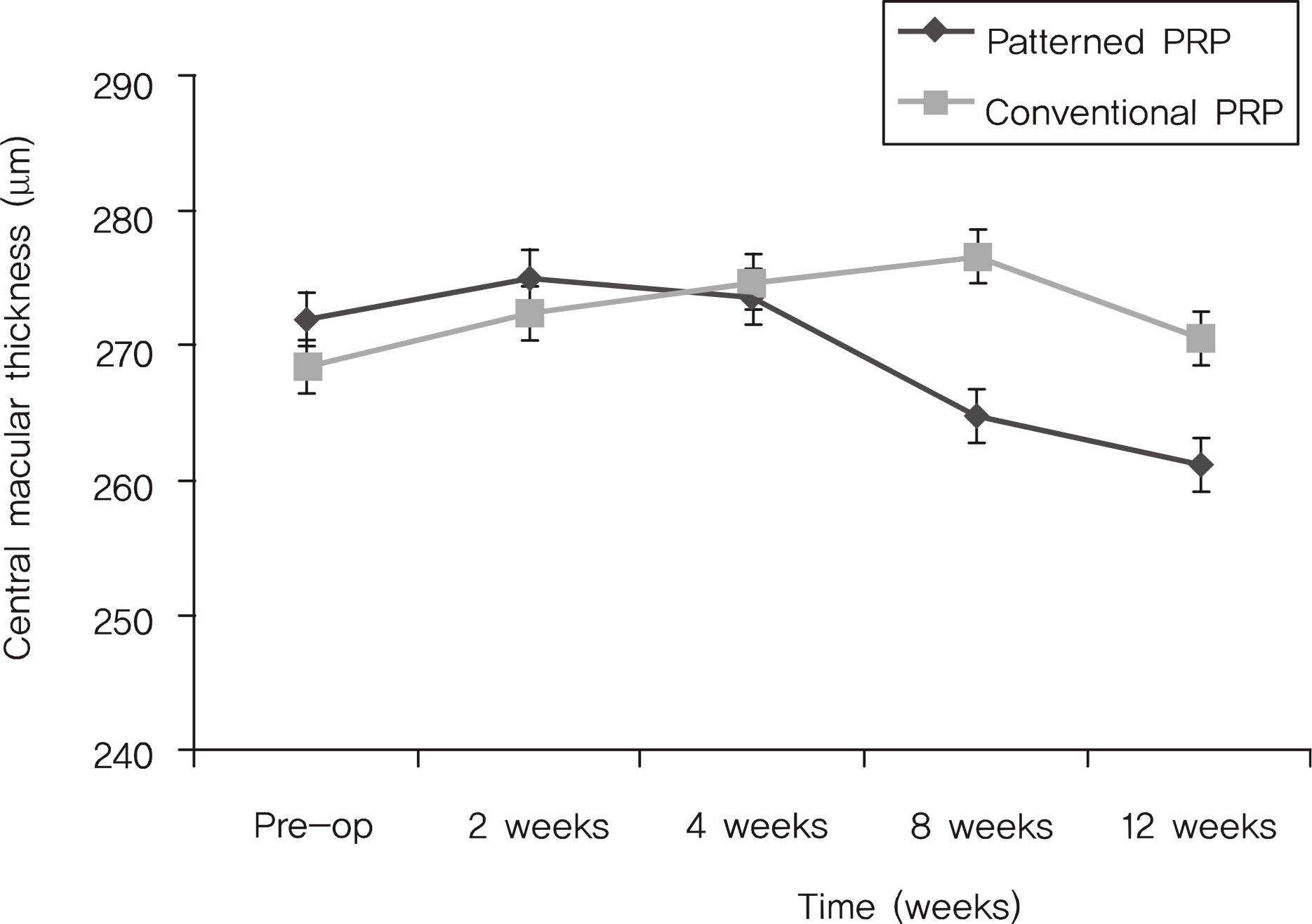
A prospective study was conducted on 36 patients (39 eyes) who required laser photocoagulation for neovascularization due to BRVO. The patients were divided into 2 groups, the patterned laser photocoagulation group (laser exposure time 0.02 sec, 3 x 3 array patterned photocoagulation) and conventional laser photocoagulation group (laser exposure time 0.2 sec). Other laser parameters (burn intensity and spot size) were the same. Pain score at the time of treatment was monitored after the laser photocoagulation. In addition, best-corrected visual acuity as well as central macular thickness measurements were performed before the treatment and after 2, 4, 8, and 12 weeks. The regression of neovascularization in fluorescein angiography was monitored during follow-up periods.
RESULTS
The patterned laser photocoagulation group had a greater reduction in pain during laser photocoagulation, and a decreased change in central macular thickness after laser photocoagulation than the conventional laser photocoagulation group. In particular, the patterned laser photocoagulation group had a statistically significant difference between the 2 groups at postoperative 8 and 12 weeks. The regression rate of neovascularization between the 2 groups had no statistically significant difference.
CONCLUSIONS
Patterned laser photocoagulation with a short exposure time decreases pain and postoperative macular edema with no difference in regression of neovascularization. Patterned laser photocoagulation with a short exposure time can be considered as a useful and efficient method for neovascularization in BRVO.
MeSH Terms
Figure
Reference
-
References
1. Hamilton AM, Kohner EM, Rosen D, et al. Experimental retinal vein occlusion in rhesus monkeys. I. Clinical appearance. Br J Ophthalmol. 1979; 63:377–87.2. Hockley DJ, Tripathi RC, Ashton N. Experimental retinal vein occlusion in rhesus monkeys. III. Histopathological and electron microscopical studies. Br J Ophthalmol. 1979; 63:393–411.3. Rehak J, Rehak M. Branch retinal vein occlusion: pathogenesis, visual prognosis, and treatment modalities. Curr Eye Res. 2008; 33:111–31.
Article4. Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984; 98:271–82.5. Weiter JJ, Zuckerman R. The influence of photoreceptor-RPE complex on the inner retina: explanation for beneficial effect of photocoagulation. Ophthalmology. 1980; 87:1133–9.6. Prendiville PL, McDonell PJ. Complications of laser surgery. Int Opthalmol Clin. 1992; 32:179–204.
Article7. Sanghvi C, McLauchlan R, Delgado C, et al. Initial experience with the Pascal photocoagulator: a pilot study of 75 procedures. Br J Ophthalmol. 2008; 92:1061–4.
Article8. Cho BJ, Kim TW, Woo SJ, et al. Short-term clinical outcome of patterned scanning laser photocoagulation0 with short exposure time in diabetic retinopathy. J Korean Ophthalmol Soc. 2009; 50:376–82.9. L'Esperance FA. Ophthalmic lasers. 3rd ed.1. St Louis: CV Mosby Co.;1989. p. 78–112.10. Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976; 2:175–84.
Article11. Lee DG, Cho NC. Combination of laser treatment and intravitreal triamcinolone injection for macular edema with branch retinal vein occlusion. J Korean Ophthalmol Soc. 2005; 46:287–96.12. Yang HN, Kim YJ, Kim JC, Shin KH. Clinical evaluation for branch retinal vein occlusion. J Korean Ophthalmol Soc. 1992; 33:599–604.13. Arnarsson A, Stefnsson E. Laser treatment and the mechanism of edema reduction in branch retinal vein occlusion. Invest Ophthalmol Vis Sci. 2004; 41:877–9.14. Mainster MA. Decreasing retinal photocoagulation damage; principles and techniques. Semin Ophthalmol. 1999; 14:200–9.
Article15. Al-Hussainy S, Dodson PM, Gibson JM. Pain response and follow-up of patients undergoing panretinal laser photocoagulation with reduced exposure times. Eye. 2008; 22:96–9.
Article16. Dorin G. Evolution of retinal laser therapy: minimum intensity photocoagulation. Can the laser heal the retina without harming it? Semin Ophthalmol. 2004; 19:62–8.17. Jain A, Blumenkranz MS, Paulus Y, et al. Effects of pulse duration on size and character of lesion in retinal photocoagulation. Arch Ophthalmol. 2008; 126:78–85.18. Blumenkranz MS, Yellachich D, Andersen DE, et al. Semiautomated patterned scanning laser for retinal photocoagulation. Retina. 2006; 26:370–6.
Article19. Doft BH, Blankenship GW. Single versus multiple treatment sessions of argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1982; 89:772–9.
Article20. Mainster MA, Sliney DH, Belcher CD, Buzney SM. Laser photo-disruptors: damage mechanisms, instrument design and safety. Ophthalmology. 1983; 90:973–91.21. Schuele G, Rumohr M, Huettmann G, Brinkmann R. RPE damage thresholds and mechanisms for laser exposure in microsecond to millisecond time regimen. Invest Ophthalmol Vis Sci. 2005; 46:714–9.22. Roseman RL, Olk RJ. Krypton red laser photocoagulation for retinal branch vein occlusion. Ophthalmology. 1987; 94:1120–5.23. Lee UK, Park YH, Han DK. Argon laser photocoagulation for neovascularization in retinal vein occlusion. J Korean Ophthalmol Soc. 1998; 39:1478–84.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laser Photocoagulation for Macular Edema in Branch Retinal Vein Occlusion
- Experimental Branch Retinal Vein Occlusion in Albino Rats
- The Effect of Laser Treatment on Branch Retinal Vein Occlusion
- Eales Disease Accompanied with Branch Retinal Vein Occlusion
- An Electroretinographic Changes of Laser-induced Experimental Branch Retinal Vein Occlusion in the Rabbits