J Korean Surg Soc.
2010 Dec;79(6):486-490. 10.4174/jkss.2010.79.6.486.
Cervical Epidural Anesthesia for Arteriovenous Bridge Graft at Upper Arm in Chronic Renal Failure Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea. syok2377@naver.com
- 2Department of General Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- KMID: 2096606
- DOI: http://doi.org/10.4174/jkss.2010.79.6.486
Abstract
- PURPOSE
Cervical epidural analgesia is used for pain control in head and neck or upper arm. But it is not commonly used for the purpose of pure regional anesthesia for upper arm surgery. Therefore, we investigated the usefulness of cervical epidural anesthesia (CEA) as a method of regional anesthesia for arteriovenous bridge graft (AVBG) for hemodialysis at upper arm and evaluated the effects of CEA on hemodynamics and respiration.
METHODS
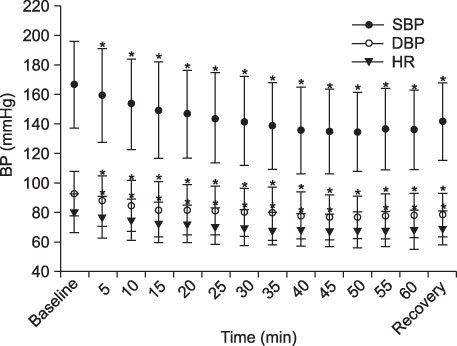
One hundred-fifty chronic renal failure patients scheduled for AVBG were randomly assigned. In the sitting position, an epidural catheter was inserted at C6-7 or C7-T1 and 15 ml of 0.375% ropivacaine with fentanyl 20microg was injected. Analgesic level, blood pressure and heart rate were measured at 5-minute intervals after injection of the drug. Arterial blood sampling was taken for aBGA before and twenty minutes after CEA.
RESULTS
Average anesthetic dermatomalsensory levels were C3.4+/-1.2~T5.7+/-2.8. During surgery, hypotension was noted in 49% of patients. It was treated with ephedrine or phenylephrine i.v. Baseline PaCO2 changed from 42.4+/-2.9 mmHg to 44.6+/-3.6 mmHg.
CONCLUSION
The above results suggest that CEA is suitable for AVBG at upper arm as a regional anesthesia.
Keyword
MeSH Terms
-
Amides
Analgesia, Epidural
Anesthesia, Conduction
Anesthesia, Epidural
Arm
Arteriovenous Shunt, Surgical
Blood Gas Analysis
Blood Pressure
Catheters
Ephedrine
Fentanyl
Head
Heart Rate
Hemodynamics
Humans
Hypotension
Kidney Failure, Chronic
Neck
Phenylephrine
Renal Dialysis
Transplants
Amides
Ephedrine
Fentanyl
Phenylephrine
Figure
Reference
-
1. Catchlove RF, Braha R. The use of cervical epidural nerve blocks in the management of chronic head and neck pain. Can Anaesth Soc J. 1984. 31:188–191.2. Cicala RS, Thoni K, Angel JJ. Long-term results of cervical epidural steroid injections. Clin J Pain. 1989. 5:143–145.3. Castagnera L, Maurette P, Pointillart V, Vital JM, Erny P, Sénégas J. Long-term results of cervical epidural steroid injection with and without morphine in chronic cervical radicular pain. Pain. 1994. 58:239–243.4. Gil SH, Hwang KH, Park W. Clinical study of continuous cervical epidural anesthesia with bupivacaine. J Korean Pain Soc. 1988. 1:20–27.5. Hong JG, Lee C, Park CH, Kim WT. Bupivacaine versus bupivacaine-fentanyl for cervical epidural anesthesia. Korean J Anesthesiol. 1997. 32:44–50.6. Crawford OB, Buckingham WW, Ottosen P, Brasher CA. Peridural anesthesia in thoracic surgery; a review of 677 cases. Anesthesiology. 1951. 12:73–84.7. Crawford OB, Brasher C, Buckingham WW. Peridural anesthesia for thoracic surgery. Anesthesiology. 1957. 18:241–249.8. Biboulet P, Deschodt J, Capdevila X, Landreau L, Aubas P, du Cailar J, et al. Hemodynamic effects of 0.375% versus 0.25% bupivacaine during cervical epidural anesthesia for hand surgery. Reg Anesth. 1995. 20:33–40.9. Bonnet F, Derosier JP, Pluskwa F, Abhay K, Gaillard A. Cervical epidural anaesthesia for carotid artery surgery. Can J Anaesth. 1990. 37:353–358.10. Capdevila X, Biboulet P, Rubenovitch J, Serre-Cousine O, Peray P, Deschodt J, et al. The effects of cervical epidural anesthesia with bupivacaine on pulmonary function in conscious patients. Anesth Analg. 1998. 86:1033–1038.11. Wittich DJ Jr, Berny JJ, Davis RK. Cervical epidural anesthesia for head and neck surgery. Laryngoscope. 1984. 94:615–619.12. Brockway MS, Bannister J, McClure JH, McKeown D, Wildsmith JA. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth. 1991. 66:31–37.13. Han KR, Kim C, Park SK, Kim JS. Distance to the adult cervical epidural space. Reg Anesth Pain Med. 2003. 28:95–97.14. Ok SY, Ryoo SH, Baek YH, Kim SH, Kim SI, Kim SC, et al. Drip infusion method as a useful indicator for identification of the epidural space. Korean J Anesthesiol. 2009. 57:181–184.15. Dogliotti AM. Segmental peridural spinal anesthesia: a new method of block anesthesia. Am J Surg. 1933. 20:107–118.16. Weber S, Bennett CR, Jones NF. Improvement in blood flow during lower extremity microsurgical free tissue transfer associated with epidural anesthesia. Anesth Analg. 1988. 67:703–705.17. Scott GR, Rothkopf DM, Walton RL. Efficacy of epidural anesthesia in free flaps to the lower extremity. Plast Reconstr Surg. 1993. 91:673–677.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drip infusion method as a useful indicator for identification of the epidural space
- Comparison of Methods to Confirm the Cervical Epidural Space
- Ischemic Monomelic Neuropathy of Both Upper Extremity: A Complication of Hemodialysis Access Procedure
- Venous Backflow in a Patent Polytetrafluoroethylene Arteriovenous Graft: A case report
- A Case of Septic Pulmonary Embolism in an End-Stage Renal Failure Patient with Infected Arterio-venous Graft for Hemodialysis