J Korean Thyroid Assoc.
2012 Nov;5(2):148-156. 10.11106/jkta.2012.5.2.148.
Serial Measurements of Off-Thyroxine Serum TSH and Thyroglobulin Levels to Predict Local and/or Systemic Metastasis of Papillary Thyroid Cancer after Total Thyroidectomy
- Affiliations
-
- 1Department of Nuclear Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 2Department of Laboratory Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 3Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea. drdhkso@hanmail.net
- 4Department of Nuclear Medicine, Soonchunhyang University Hospital, Cheonan, Korea.
- KMID: 2095105
- DOI: http://doi.org/10.11106/jkta.2012.5.2.148
Abstract
- BACKGROUND AND OBJECTIVES
Off-thyroxine serum thyroglobulin (Tg) level is important to predict metastatic disease (MD) in papillary thyroid cancer (PTC); however, it is unclear whether a single off-thyroxine Tg level is sufficient for predicting MD. In this study, we determined whether serial measurement of off-thyroxine serum Tg level can predict metastasis in PTC patients after total thyroidectomy.
MATERIALS AND METHODS
We enrolled 140 PTC patients in whom serum thyroid-stimulating hormone (TSH) and Tg levels were measured 7 days before radio-iodine (RAI) treatment (TSHA and TgA) and on the day of RAI treatment (TSHB and TgB) with withholding L-thyroxine for 4 weeks before RAI treatment. The values of TSHinc (TSHB-TSHA) and Tginc (TgB-TgA), Tgratio (TgB/TgA), Tginc/TSHinc and Tgratio/TSHinc were calculated. Tginc/TSHinc and Tgratio/TSHinc were tested if those parameters can predict MD in patients with TSHA>30 microIU/mL and TgA<10 ng/mL.
RESULTS
Forty-four patients had MD and 96 had no evidence of MD (non-MD). MD group showed higher levels of TgA, TgB, Tginc, Tginc/TSHinc and Tgratio/TSHinc compared with non-MD group. A significant correlation was found between TSHinc and Tgratio (r=0.669) in MD group. In 43 patients with TSHA>30 microIU/mL and TgA<10 ng/mL (MD, 9; non-MD, 34), both Tginc/TSHinc (100%) and Tgratio/TSHinc (89%) had higher sensitivities for predicting MD than TgB (78%).
CONCLUSION
With the increment in serum Tg corrected for the increment in serum TSH, serial measurements of off-thyroxine serum TSH and Tg levels can help predict PTC metastasis.
Keyword
MeSH Terms
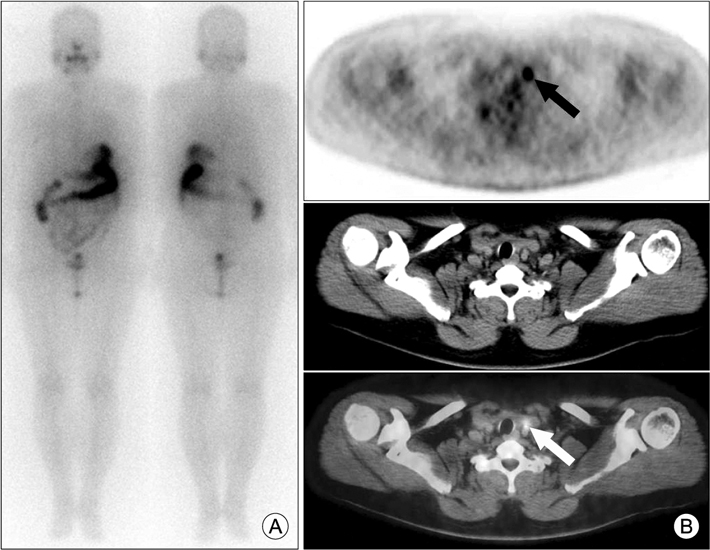
Figure
Reference
-
1. Iervasi A, Iervasi G, Carpi A, Zucchelli GC. Serum thyroglobulin measurement: clinical background and main methodological aspects with clinical impact. Biomed Pharmacother. 2006. 60(8):414–424.
Article2. Francis Z, Schlumberger M. Serum thyroglobulin determination in thyroid cancer patients. Best Pract Res Clin Endocrinol Metab. 2008. 22(6):1039–1046.
Article3. Van Herle AJ, Uller RP, Matthews NI, Brown J. Radioimmunoassay for measurement of thyroglobulin in human serum. J Clin Invest. 1973. 52(6):1320–1327.
Article4. Torrens JI, Burch HB. Serum thyroglobulin measurement. Utility in clinical practice. Endocrinol Metab Clin North Am. 2001. 30(2):429–467.5. Eustatia-Rutten CF, Smit JW, Romijn JA, van der Kleij-Corssmit EP, Pereira AM, Stokkel MP, et al. Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis. Clin Endocrinol (Oxf). 2004. 61(1):61–74.
Article6. Mazzaferri EL, Robbins RJ, Spencer CA, Braverman LE, Pacini F, Wartofsky L, et al. A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 2003. 88(4):1433–1441.
Article7. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19(11):1167–1214.
Article8. Mazzaferri EL. Empirically treating high serum thyroglobulin levels. J Nucl Med. 2005. 46(7):1079–1088.9. Silberstein EB. The problem of the patient with thyroglobulin elevation but negative iodine scintigraphy: the TENIS syndrome. Semin Nucl Med. 2011. 41(2):113–120.
Article10. Lin Y, Li T, Liang J, Li X, Qiu L, Wang S, et al. Predictive value of preablation stimulated thyroglobulin and thyroglobulin/thyroid-stimulating hormone ratio in differentiated thyroid cancer. Clin Nucl Med. 2011. 36(12):1102–1105.
Article11. Robbins RJ, Srivastava S, Shaha A, Ghossein R, Larson SM, Fleisher M, et al. Factors influencing the basal and recombinant human thyrotropin-stimulated serum thyroglobulin in patients with metastatic thyroid carcinoma. J Clin Endocrinol Metab. 2004. 89(12):6010–6016.
Article12. Spencer CA, LoPresti JS, Fatemi S, Nicoloff JT. Detection of residual and recurrent differentiated thyroid carcinoma by serum thyroglobulin measurement. Thyroid. 1999. 9(5):435–441.
Article13. Bachelot A, Cailleux AF, Klain M, Baudin E, Ricard M, Bellon N, et al. Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid. 2002. 12(8):707–711.
Article14. Pellegriti G, Scollo C, Regalbuto C, Attard M, Marozzi P, Vermiglio F, et al. The diagnostic use of the rhTSH/thyroglobulin test in differentiated thyroid cancer patients with persistent disease and low thyroglobulin levels. Clin Endocrinol (Oxf). 2003. 58(5):556–561.
Article15. Ma C, Xie J, Kuang A. Is empiric 131I therapy justified for patients with positive thyroglobulin and negative 131I whole-body scanning results? J Nucl Med. 2005. 46(7):1164–1170.16. Kim WG, Ryu JS, Kim EY, Lee JH, Baek JH, Yoon JH, et al. Empiric high-dose 131-iodine therapy lacks efficacy for treated papillary thyroid cancer patients with detectable serum thyroglobulin, but negative cervical sonography and 18F-fluorodeoxyglucose positron emission tomography scan. J Clin Endocrinol Metab. 2010. 95(3):1169–1173.
Article17. Pacini F, Agate L, Elisei R, Capezzone M, Ceccarelli C, Lippi F, et al. Outcome of differentiated thyroid cancer with detectable serum Tg and negative diagnostic (131)I whole body scan: comparison of patients treated with high (131)I activities versus untreated patients. J Clin Endocrinol Metab. 2001. 86(9):4092–4097.
Article18. Robbins RJ, Chon JT, Fleisher M, Larson SM, Tuttle RM. Is the serum thyroglobulin response to recombinant human thyrotropin sufficient, by itself, to monitor for residual thyroid carcinoma? J Clin Endocrinol Metab. 2002. 87(7):3242–3247.
Article19. Park EK, Chung JK, Lim IH, Park do J, Lee DS, Lee MC, et al. Recurrent/metastatic thyroid carcinomas false negative for serum thyroglobulin but positive by posttherapy I-131 whole body scans. Eur J Nucl Med Mol Imaging. 2009. 36(2):172–179.
Article20. Ministry of Health and Welfare. The Korea central cancer registry. Annual report of cancer statistics in Korea in 2008. 2010. Seoul, Korea: Ministry of Health and Welfare.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Serum Thyroglobulin in Patients with Papillary Thyroid Carcinoma
- Predictors Associated with the Maintenance of Normal Thyroid Function after Unilateral Total Thyroidectomy in Patients with Papillary Thyroid Microcarcinoma
- Serial Changes of Serum Thyroid-Stimulating Hormone after Total Thyroidectomy or Withdrawal of Suppressive Thyroxine Therapy in Patients with Differentiated Thyroid Cancer
- Factors That Influence TSH Levels after Thyrogen Injection before RAI Therapy
- Serum Thyroglobulin Levels Predicting Recurrence and Distant Metastasis after Surgery in Patients with Differentiated Thyroid Cancer